Ann Rehabil Med.
2016 Apr;40(2):244-251. 10.5535/arm.2016.40.2.244.
Sonoanatomical Change of Phrenic Nerve According to Posture During Ultrasound-Guided Stellate Ganglion Block
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Korea University Guro Hospital, Seoul, Korea. rehab46@korea.ac.kr
- KMID: 2309923
- DOI: http://doi.org/10.5535/arm.2016.40.2.244
Abstract
OBJECTIVE
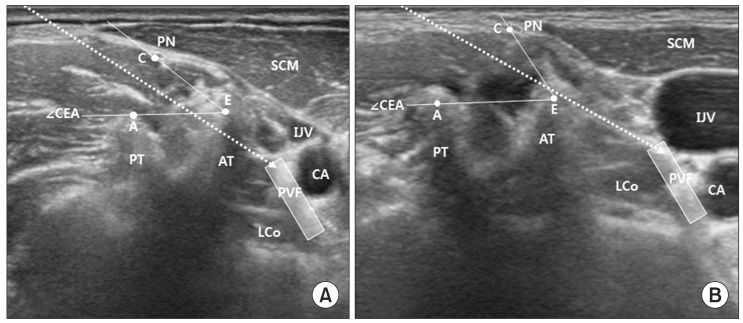
To evaluate the risk of phrenic nerve injury during ultrasound-guided stellate ganglion block (US-SGB) according to sonoanatomy of the phrenic nerve, and determine a safer posture for needle insertion by assessing its relationship with surrounding structure according to positional change.
METHODS
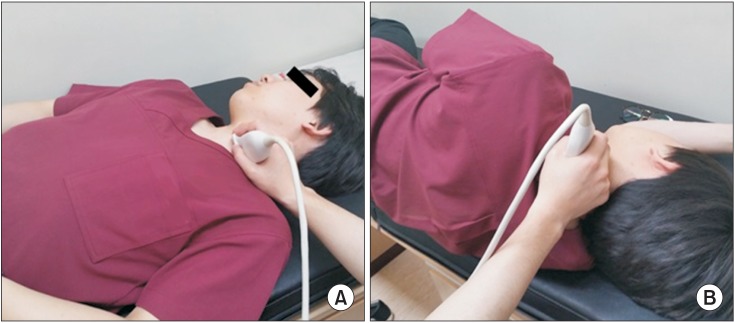
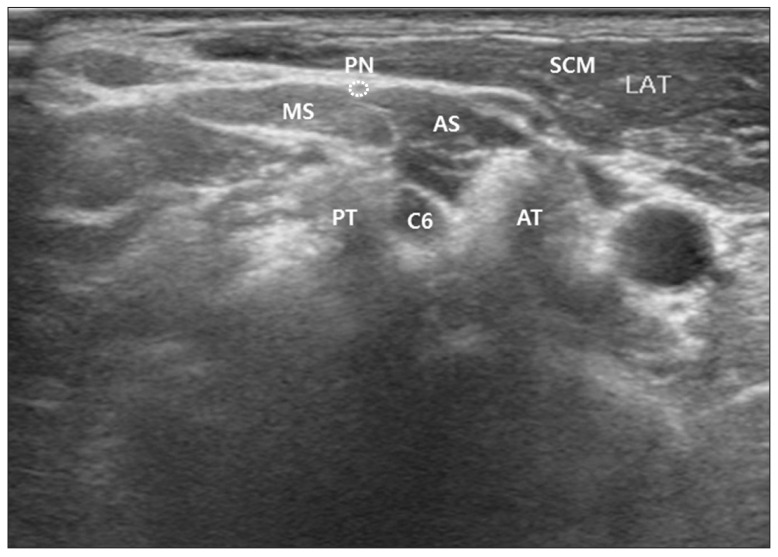
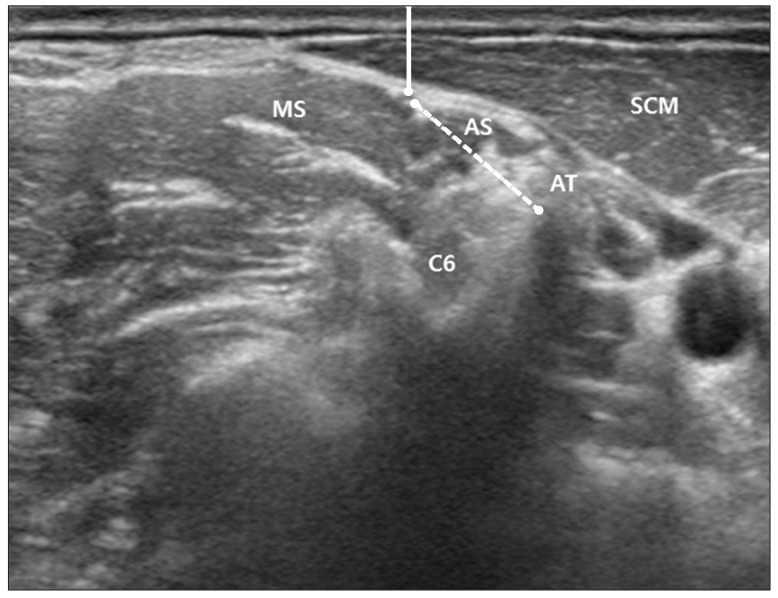
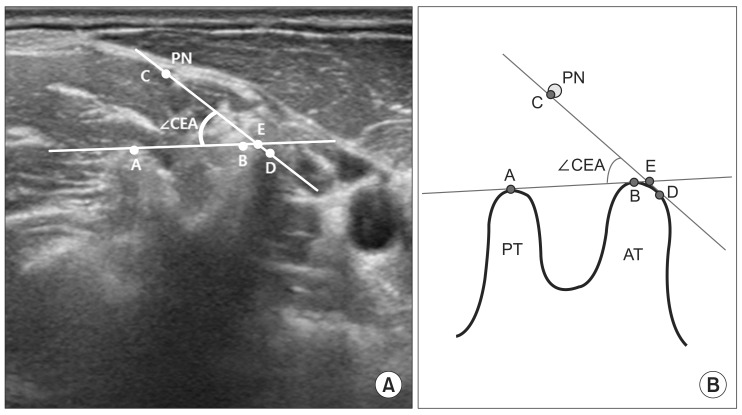
Twenty-nine healthy volunteers were recruited and underwent ultrasound in two postures, i.e., supine position with the neck extension and head rotation, and lateral decubitus position. The transducer was placed at the anterior tubercle of the C6 level to identify phrenic nerve. The cross-sectional area (CSA), depth from skin, distance between phrenic nerve and anterior tubercle of C6 transverse process, and the angle formed by anterior tubercle, posterior tubercle and phrenic nerve were measured.
RESULTS
The phrenic nerve was clearly identified in the intermuscular fascia layer between the anterior scalene and sternocleidomastoid muscles. The distance between the phrenic nerve and anterior tubercle was 10.33±3.20 mm with the supine position and 9.20±3.31 mm with the lateral decubitus position, respectively. The mean CSA and skin depth of phrenic nerve were not statistically different between the two positions. The angle with the supine position was 48.37°±27.43°, and 58.89°±30.02° with the lateral decubitus position. The difference of angle between the two positions was statistically significant.
CONCLUSION
Ultrasound is a useful tool for assessing the phrenic nerve and its anatomical relation with other cervical structures. In addition, lateral decubitus position seems to be safer by providing wider angle for needle insertion than the supine position in US-SGB.
Keyword
MeSH Terms
Figure
Reference
-
1. Elias M. Cervical sympathetic and stellate ganglion blocks. Pain Physician. 2000; 3:294–304. PMID: 16906187.
Article2. Kessler J, Schafhalter-Zoppoth I, Gray AT. An ultrasound study of the phrenic nerve in the posterior cervical triangle: implications for the interscalene brachial plexus block. Reg Anesth Pain Med. 2008; 33:545–550. PMID: 19258969.
Article3. Canella C, Demondion X, Delebarre A, Moraux A, Cotten H, Cotten A. Anatomical study of phrenic nerve using ultrasound. Eur Radiol. 2010; 20:659–665. PMID: 19727747.
Article4. Gofeld M, Bhatia A, Abbas S, Ganapathy S, Johnson M. Development and validation of a new technique for ultrasound-guided stellate ganglion block. Reg Anesth Pain Med. 2009; 34:475–479. PMID: 19920422.
Article5. Narouze SN. Ultrasound-guided cervical spine injections: ultrasound "prevents" whereas contrast fluoroscopy "detects" intravascular injections. Reg Anesth Pain Med. 2012; 37:127–130. PMID: 22354064.6. Narouze SN, Vydyanathan A, Kapural L, Sessler DI, Mekhail N. Ultrasound-guided cervical selective nerve root block: a fluoroscopy-controlled feasibility study. Reg Anesth Pain Med. 2009; 34:343–348. PMID: 19574867.7. Saranteas T, Paraskeuopoulos T, Anagnostopoulou S, Kanellopoulos I, Mastoris M, Kostopanagiotou G. Ultrasound anatomy of the cervical paravertebral space: a preliminary study. Surg Radiol Anat. 2010; 32:617–622. PMID: 20082079.
Article8. Siegenthaler A, Mlekusch S, Schliessbach J, Curatolo M, Eichenberger U. Ultrasound imaging to estimate risk of esophageal and vascular puncture after conventional stellate ganglion block. Reg Anesth Pain Med. 2012; 37:224–227. PMID: 22157739.
Article9. Abdi S, Zhou Y, Patel N, Saini B, Nelson J. A new and easy technique to block the stellate ganglion. Pain Physician. 2004; 7:327–331. PMID: 16858470.
Article10. Wallace MS, Milholland AV. Contralateral spread of local anesthetic withstellate ganglion block. Reg Anesth. 1993; 18:55–59. PMID: 8095400.11. Mak PH, Irwin MG, Ooi CG, Chow BF. Incidence of diaphragmatic paralysis following supraclavicular brachial plexus block and its effect on pulmonary function. Anaesthesia. 2001; 56:352–356. PMID: 11284823.
Article12. Robaux S, Bouaziz H, Boisseau N, Raucoules-Aime M, Laxenaire MC. S.O.S. Regional Hot Line Service. Persistent phrenic nerve paralysis following interscalene brachial plexus block. Anesthesiology. 2001; 95:1519–1521. PMID: 11748414.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bilateral Horner's Syndrome after a Stellate Ganglion Block
- Computerized Tomography - guided Percutaneous Radiofrequency
- Stellate Ganglion Block for the Treatment of Classic Migraine: A case report
- Thermographic Follow up of the Stellate Ganglion Block: Case Report
- Ultrasound-Guided Pain Interventions: A Review of Techniques for Peripheral Nerves