Stroke Prevention in Atrial Fibrillation: Focus on Asian Patients
- Affiliations
-
- 1Institute of Cardiovascular Sciences, University of Birmingham, Birmingham, United Kingdom. g.y.h.lip@bham.ac.uk
- 2Department of Cardiology, Chinese PLA Medical School, Beijing, China.
- 3Division of Cardiology, Department of Internal Medicine, Soon Chun Hyang University Hospital Seoul, Seoul, Korea.
- 4Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- 5Aalborg Thrombosis Research Unit, Department of Clinical Medicine, Aalborg University, Aalborg, Denmark.
- KMID: 2417690
- DOI: http://doi.org/10.4070/kcj.2018.0190
Abstract
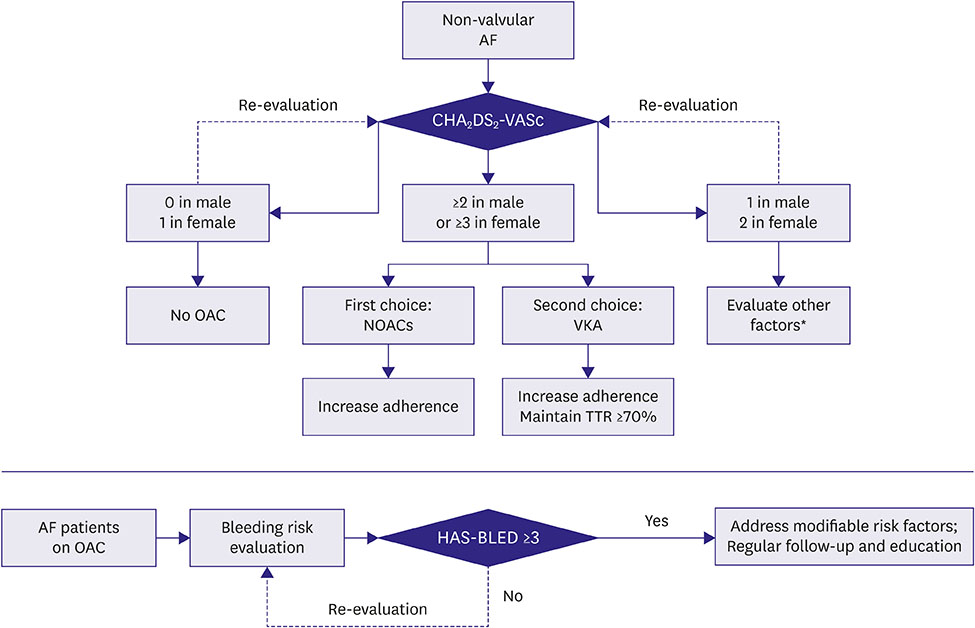
- Atrial fibrillation (AF) is the most common arrhythmia conferring a fivefold increased risk of stroke. Stroke prevention is the cornerstone of management of patients with AF. Asians have a generally higher incidence of AF-related risks of stroke and bleeding (particularly intracranial bleeding), compared with non-Asians. Despite the well-documented efficacy and relative safety of oral anticoagulation for stroke prevention among Asians, the suboptimal use of oral anticoagulation remains common. The current narrative review aims to provide a summary of the available evidence on stroke prevention among patients with AF focused on the Asia region, regarding stroke and bleeding risk evaluation, the performance of oral anticoagulation, and current use of thromboprophylaxis.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Cardiovascular Research Using the Korean National Health Information Database
Eue-Keun Choi
Korean Circ J. 2020;50(9):754-772. doi: 10.4070/kcj.2020.0171.Real World Comparison of Rivaroxaban and Warfarin in Korean Patients with Atrial Fibrillation: Propensity Matching Cohort Analysis
Hyung Ki Jeong, Ki Hong Lee, Hyung Wook Park, Nam Sik Yoon, Min Chul Kim, Nuri Lee, Ji Sung Kim, Youngkeun Ahn, Myung Ho Jeong, Jong Chun Park, Jeong Gwan Cho
Chonnam Med J. 2019;55(1):54-61. doi: 10.4068/cmj.2019.55.1.54.Impact of Non-Vitamin K Antagonist Oral Anticoagulants on the Change of Antithrombotic Regimens in Patients with Atrial Fibrillation Undergoing Percutaneous Coronary Intervention
Soonil Kwon, Jin-Hyung Jung, Eue-Keun Choi, Seung-Woo Lee, Jiesuck Park, So-Ryoung Lee, Jeehoon Kang, Kyungdo Han, Kyung Woo Park, Seil Oh, Gregory Y. H. Lip
Korean Circ J. 2021;51(5):409-422. doi: 10.4070/kcj.2020.0407.
Reference
-
1. Chao TF, Liu CJ, Tuan TC, et al. Lifetime risks, projected numbers, and adverse outcomes in Asian patients with atrial fibrillation: a report from the Taiwan nationwide AF cohort study. Chest. 2018; 153:453–466.2. Lee SR, Choi EK, Han KD, Cha MJ, Oh S. Trends in the incidence and prevalence of atrial fibrillation and estimated thromboembolic risk using the CHA2DS2-VASc score in the entire Korean population. Int J Cardiol. 2017; 236:226–231.3. Chiang CE, Wang KL, Lip GY. Stroke prevention in atrial fibrillation: an Asian perspective. Thromb Haemost. 2014; 111:789–797.
Article4. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991; 22:983–988.
Article5. Gladstone DJ, Bui E, Fang J, et al. Potentially preventable strokes in high-risk patients with atrial fibrillation who are not adequately anticoagulated. Stroke. 2009; 40:235–240.
Article6. Man-Son-Hing M, Laupacis A. Balancing the risks of stroke and upper gastrointestinal tract bleeding in older patients with atrial fibrillation. Arch Intern Med. 2002; 162:541–550.
Article7. Henninger N, Goddeau RP Jr, Karmarkar A, Helenius J, McManus DD. Atrial fibrillation is associated with a worse 90-day outcome than other cardioembolic stroke subtypes. Stroke. 2016; 47:1486–1492.
Article8. Perera KS, Vanassche T, Bosch J, et al. Global survey of the frequency of atrial fibrillation-associated stroke: embolic stroke of undetermined source global registry. Stroke. 2016; 47:2197–2202.9. Tomita H, Hagii J, Metoki N, et al. Impact of sex difference on severity and functional outcome in patients with cardioembolic stroke. J Stroke Cerebrovasc Dis. 2015; 24:2613–2618.
Article10. Kim D, Yang PS, Jang E, et al. Increasing trends in hospital care burden of atrial fibrillation in Korea, 2006 through 2015. Heart. 2018.
Article11. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010; 137:263–272.12. Hart RG, Pearce LA, Aguilar MI. Adjusted-dose warfarin versus aspirin for preventing stroke in patients with atrial fibrillation. Ann Intern Med. 2007; 147:590–592.
Article13. Lip GY, Wang KL, Chiang CE. Non-vitamin K antagonist oral anticoagulants (NOACs) for stroke prevention in Asian patients with atrial fibrillation: time for a reappraisal. Int J Cardiol. 2015; 180:246–254.
Article14. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–992.15. Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013; 369:2093–2104.
Article16. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–891.
Article17. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139–1151.
Article18. Cha MJ, Choi EK, Han KD, et al. Effectiveness and safety of non-vitamin K antagonist oral anticoagulants in Asian patients with atrial fibrillation. Stroke. 2017; 48:3040–3048.
Article19. Hori M, Connolly SJ, Zhu J, et al. Dabigatran versus warfarin: effects on ischemic and hemorrhagic strokes and bleeding in Asians and non-Asians with atrial fibrillation. Stroke. 2013; 44:1891–1896.
Article20. Wong KS, Hu DY, Oomman A, et al. Rivaroxaban for stroke prevention in East Asian patients from the ROCKET AF trial. Stroke. 2014; 45:1739–1747.
Article21. Yamashita T, Koretsune Y, Yang Y, et al. Edoxaban vs. warfarin in East Asian patients with atrial fibrillation - an ENGAGE AF-TIMI 48 subanalysis. Circ J. 2016; 80:860–869.22. Goto S, Zhu J, Liu L, et al. Efficacy and safety of apixaban compared with warfarin for stroke prevention in patients with atrial fibrillation from East Asia: a subanalysis of the Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) Trial. Am Heart J. 2014; 168:303–309.
Article23. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016; 37:2893–2962.24. Chiang CE, Okumura K, Zhang S, et al. 2017 consensus of the Asia Pacific Heart Rhythm Society on stroke prevention in atrial fibrillation. J Arrhythm. 2017; 33:345–367.
Article25. Jones C, Pollit V, Fitzmaurice D, Cowan C; Guideline Development Group. The management of atrial fibrillation: summary of updated NICE guidance. BMJ. 2014; 348:g3655.
Article26. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1–e76.27. Chao TF, Liu CJ, Tuan TC, et al. Comparisons of CHADS2 and CHA2DS2-VASc scores for stroke risk stratification in atrial fibrillation: which scoring system should be used for Asians? Heart Rhythm. 2016; 13:46–53.
Article28. Xiong Q, Chen S, Senoo K, Proietti M, Hong K, Lip GY. The CHADS2 and CHA2DS2-VASc scores for predicting ischemic stroke among East Asian patients with atrial fibrillation: a systemic review and meta-analysis. Int J Cardiol. 2015; 195:237–242.
Article29. Kim TH, Yang PS, Kim D, et al. CHA2DS2-VASc score for identifying truly low-risk atrial fibrillation for stroke: a Korean nationwide cohort study. Stroke. 2017; 48:2984–2990.30. Kang SH, Choi EK, Han KD, et al. Risk of ischemic stroke in patients with non-valvular atrial fibrillation not receiving oral anticoagulants - Korean nationwide population-based study. Circ J. 2017; 81:1158–1164.31. Chao TF, Liu CJ, Wang KL, et al. Using the CHA2DS2-VASc score for refining stroke risk stratification in ‘low-risk’ Asian patients with atrial fibrillation. J Am Coll Cardiol. 2014; 64:1658–1665.32. Chan PH, Lau CP, Tse HF, Chiang CE, Siu CW. CHA2DS2-VASc recalibration with an additional age category (50–64 Years) enhances stroke risk stratification in Chinese patients with atrial fibrillation. Can J Cardiol. 2016; 32:1381–1387.33. Chao TF, Wang KL, Liu CJ, et al. Age threshold for increased stroke risk among patients with atrial fibrillation: a nationwide cohort study from Taiwan. J Am Coll Cardiol. 2015; 66:1339–1347.34. Chao TF, Lip GY, Liu CJ, et al. Validation of a modified CHA2DS2-VASc score for stroke risk stratification in Asian patients with atrial fibrillation: a nationwide cohort study. Stroke. 2016; 47:2462–2469.35. Chao TF, Liu CJ, Wang KL, et al. Should atrial fibrillation patients with 1 additional risk factor of the CHA2DS2-VASc score (beyond sex) receive oral anticoagulation? J Am Coll Cardiol. 2015; 65:635–642.36. Hung Y, Chao TF, Liu CJ, et al. Is an oral anticoagulant necessary for young atrial fibrillation patients with a CHA2DS2-VASc score of 1 (men) or 2 (women)? J Am Heart Assoc. 2016; 5:e003839.
Article37. Eckman MH, Singer DE, Rosand J, Greenberg SM. Moving the tipping point: the decision to anticoagulate patients with atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2011; 4:14–21.38. JCS Joint Working Group. Guidelines for pharmacotherapy of atrial fibrillation (JCS 2013). Circ J. 2014; 78:1997–2021.39. Chiang CE, Wu TJ, Ueng KC, et al. 2016 guidelines of the Taiwan Heart Rhythm Society and the Taiwan Society of Cardiology for the management of atrial fibrillation. J Formos Med Assoc. 2016; 115:893–952.
Article40. Jung BC, Kim NH, Nam GB, et al. The Korean Heart Rhythm Society's 2014 statement on antithrombotic therapy for patients with nonvalvular atrial fibrillation: Korean Heart Rhythm Society. Korean Circ J. 2015; 45:9–19.
Article41. Lee JM, Joung B, Cha MJ, et al. 2018 KHRS guidelines for stroke prevention therapy in Korean patients with nonvalvular atrial fibrillation. Korean J Med. 2018; 93:87–109.
Article42. Chao TF, Lip GY, Liu CJ, et al. Relationship of aging and incident comorbidities to stroke risk in patients with atrial fibrillation. J Am Coll Cardiol. 2018; 71:122–132.
Article43. Yoon M, Yang PS, Jang E, et al. Dynamic changes of CHA2DS2-VASc score and the risk of ischaemic stroke in Asian patients with atrial fibrillation: a nationwide cohort study. Thromb Haemost. 2018.
Article44. Lip GY, Lane DA. Bleeding risk assessment in atrial fibrillation: observations on the use and misuse of bleeding risk scores. J Thromb Haemost. 2016; 14:1711–1714.
Article45. Wilke T, Bauer S, Mueller S, Kohlmann T, Bauersachs R. Patient preferences for oral anticoagulation therapy in atrial fibrillation: a systematic literature review. Patient. 2017; 10:17–37.
Article46. Guo Y, Zhu H, Chen Y, Lip GY. Comparing bleeding risk assessment focused on modifiable risk factors only versus validated bleeding risk scores in atrial fibrillation. Am J Med. 2018; 131:185–192.
Article47. Esteve-Pastor MA, Rivera-Caravaca JM, Shantsila A, Roldán V, Lip GY, Marín F. Assessing bleeding risk in atrial fibrillation patients: comparing a bleeding risk score based only on modifiable bleeding risk factors against the HAS-BLED score. The AMADEUS trial. Thromb Haemost. 2017; 117:2261–2266.
Article48. Chao TF, Lip GY, Lin YJ, et al. Major bleeding and intracranial hemorrhage risk prediction in patients with atrial fibrillation: attention to modifiable bleeding risk factors or use of a bleeding risk stratification score? A nationwide cohort study. Int J Cardiol. 2018; 254:157–161.
Article49. Hijazi Z, Oldgren J, Lindbäck J, et al. The novel biomarker-based ABC (age, biomarkers, clinical history)-bleeding risk score for patients with atrial fibrillation: a derivation and validation study. Lancet. 2016; 387:2302–2311.
Article50. O'Brien EC, Simon DN, Thomas LE, et al. The ORBIT bleeding score: a simple bedside score to assess bleeding risk in atrial fibrillation. Eur Heart J. 2015; 36:3258–3264.51. Fang MC, Go AS, Chang Y, et al. A new risk scheme to predict warfarin-associated hemorrhage: the ATRIA (anticoagulation and risk factors in atrial fibrillation) study. J Am Coll Cardiol. 2011; 58:395–401.52. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010; 138:1093–1100.53. Guo YT, Zhang Y, Shi XM, et al. Assessing bleeding risk in 4824 Asian patients with atrial fibrillation: the Beijing PLA Hospital Atrial Fibrillation Project. Sci Rep. 2016; 6:31755.
Article54. Chao TF, Lip GY, Lin YJ, et al. Incident risk factors and major bleeding in patients with atrial fibrillation treated with oral anticoagulants: a comparison of baseline, follow-up and delta HAS-BLED scores with an approach focused on modifiable bleeding risk factors. Thromb Haemost. 2018; 118:768–777.
Article55. Park CS, Choi EK, Kim HM, et al. Increased risk of major bleeding in underweight patients with atrial fibrillation who were prescribed non-vitamin K antagonist oral anticoagulants. Heart Rhythm. 2017; 14:501–507.
Article56. Zoppellaro G, Granziera S, Bertozzo G, et al. Consequences of warfarin suspension after major bleeding in very elderly patients with non valvular atrial fibrillation. Thromb Haemost. 2017; 117:1828–1830.
Article57. Rivera-Caravaca JM, Roldán V, Esteve-Pastor MA, et al. Cessation of oral anticoagulation is an important risk factor for stroke and mortality in atrial fibrillation patients. Thromb Haemost. 2017; 117:1448–1454.
Article58. Wu S, Yang YM, Zhu J, et al. Meta-analysis of efficacy and safety of new oral anticoagulants compared with uninterrupted vitamin K antagonists in patients undergoing catheter ablation for atrial fibrillation. Am J Cardiol. 2016; 117:926–934.
Article59. Cardoso R, Knijnik L, Bhonsale A, et al. An updated meta-analysis of novel oral anticoagulants versus vitamin K antagonists for uninterrupted anticoagulation in atrial fibrillation catheter ablation. Heart Rhythm. 2018; 15:107–115.
Article60. Ntaios G, Papavasileiou V, Makaritsis K, Vemmos K, Michel P, Lip GY. Real-world setting comparison of nonvitamin-K antagonist oral anticoagulants versus vitamin-K antagonists for stroke prevention in atrial fibrillation: a systematic review and meta-analysis. Stroke. 2017; 48:2494–2503.61. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014; 383:955–962.
Article62. Li YG, Pastori D, Lip GY. Fitting the right non-vitamin K antagonist oral anticoagulant to the right patient with non-valvular atrial fibrillation: an evidence-based choice. Ann Med. 2018; 50:288–302.
Article63. Shimada YJ, Yamashita T, Koretsune Y, et al. Effects of regional differences in Asia on efficacy and safety of edoxaban compared with warfarin--insights from the ENGAGE AF-TIMI 48 trial. Circ J. 2015; 79:2560–2567.64. Hori M, Matsumoto M, Tanahashi N, et al. Rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation - the J-ROCKET AF study. Circ J. 2012; 76:2104–2111.65. Wang KL, Lip GY, Lin SJ, Chiang CE. Non-vitamin K antagonist oral anticoagulants for stroke prevention in Asian patients with nonvalvular atrial fibrillation: meta-analysis. Stroke. 2015; 46:2555–2561.66. Kohsaka S, Katada J, Saito K, Terayama Y. Safety and effectiveness of apixaban in comparison to warfarin in patients with nonvalvular atrial fibrillation: a propensity-matched analysis from Japanese administrative claims data. Curr Med Res Opin. 2018; 1–8.
Article67. Lee KH, Park HW, Lee N, et al. Optimal dose of dabigatran for the prevention of thromboembolism with minimal bleeding risk in Korean patients with atrial fibrillation. Europace. 2017; 19:iv1–9.
Article68. Hong KS, Kwon SU, Lee SH, et al. Rivaroxaban vs warfarin sodium in the ultra-early period after atrial fibrillation-related mild ischemic stroke: a randomized clinical trial. JAMA Neurol. 2017; 74:1206–1215.69. Dillinger JG, Aleil B, Cheggour S, et al. Dosing issues with non-vitamin K antagonist oral anticoagulants for the treatment of non-valvular atrial fibrillation: Why we should not underdose our patients. Arch Cardiovasc Dis. 2018; 111:85–94.
Article70. Okumura Y, Yokoyama K, Matsumoto N, et al. Current use of direct oral anticoagulants for atrial fibrillation in Japan: Findings from the SAKURA AF Registry. J Arrhythm. 2017; 33:289–296.
Article71. Wang KL, Giugliano RP, Goto S, et al. Standard dose versus low dose non-vitamin K antagonist oral anticoagulants in Asian patients with atrial fibrillation: a meta-analysis of contemporary randomized controlled trials. Heart Rhythm. 2016; 13:2340–2347.
Article72. Holmes DR, Reddy VY, Turi ZG, PROTECT AF Investigators, et al. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet. 2009; 374:534–542.
Article73. Holmes DR Jr, Kar S, Price MJ, et al. Prospective randomized evaluation of the Watchman Left Atrial Appendage Closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. J Am Coll Cardiol. 2014; 64:1–12.74. Reddy VY, Doshi SK, Kar S, et al. 5-Year Outcomes After Left Atrial Appendage Closure: From the PREVAIL and PROTECT AF Trials. J Am Coll Cardiol. 2017; 70:2964–2975.75. Lam YY, Yip GW, Yu CM, et al. Left atrial appendage closure with AMPLATZER cardiac plug for stroke prevention in atrial fibrillation: initial Asia-Pacific experience. Catheter Cardiovasc Interv. 2012; 79:794–800.
Article76. Lee OH, Kim JS, Pak HN, et al. Feasibility of left atrial appendage occlusion for left atrial appendage thrombus in patients with persistent atrial fibrillation. Am J Cardiol. 2018; 121:1534–1539.
Article77. Kim JS, Lee H, Suh Y, et al. Left atrial appendage occlusion in non-valvular atrial fibrillation in a Korean Multi-Center Registry. Circ J. 2016; 80:1123–1130.
Article78. Chen Y, Zhang Y, Huang W, Huang K, Xu B, Su XI. Primary and secondary stroke prevention using left atrial appendage closure with Watchman devices in atrial fibrillation patients: a single center experience from Mainland China. Pacing Clin Electrophysiol. 2017; 40:607–614.79. Landmesser U, Schmidt B, Nielsen-Kudsk JE, et al. Left atrial appendage occlusion with the AMPLATZER Amulet device: periprocedural and early clinical/echocardiographic data from a global prospective observational study. EuroIntervention. 2017; 13:867–876.
Article80. Phan QT, Shin SY, Cho IS, et al. Impact of left atrial appendage closure on cardiac functional and structural remodeling: a Difference-in-Difference analysis of propensity score matched samples. Cardiol J. 2018.
Article81. Siu CW, Tse HF. Net clinical benefit of warfarin therapy in elderly Chinese patients with atrial fibrillation. Circ Arrhythm Electrophysiol. 2014; 7:300–306.
Article82. Huisman MV, Rothman KJ, Paquette M, et al. Antithrombotic treatment patterns in patients with newly diagnosed nonvalvular atrial fibrillation: the GLORIA-AF Registry, Phase II. Am J Med. 2015; 128:1306–1313.e1.
Article83. Bassand JP, Accetta G, Camm AJ, et al. Two-year outcomes of patients with newly diagnosed atrial fibrillation: results from GARFIELD-AF. Eur Heart J. 2016; 37:2882–2889.
Article84. Guo Y, Wang H, Tian Y, Wang Y, Lip GY. Time trends of aspirin and warfarin use on stroke and bleeding events in Chinese patients with new-onset atrial fibrillation. Chest. 2015; 148:62–72.
Article85. Chang SS, Dong JZ, Ma CS, et al. Current status and time trends of oral anticoagulation use among Chinese patients with nonvalvular atrial fibrillation: the Chinese atrial fibrillation registry study. Stroke. 2016; 47:1803–1810.86. Siu CW, Lip GY, Lam KF, et al. Risk of stroke and intracranial hemorrhage in 9727 Chinese with atrial fibrillation in Hong Kong. Heart Rhythm. 2014; 11:1401–1408.
Article87. Son MK, Lim NK, Park HY. Trend of prevalence of atrial fibrillation and use of oral anticoagulation therapy in patients with atrial fibrillation in South Korea (2002–2013). J Epidemiol. 2018; 28:81–87.
Article88. Lee SR, Choi EK, Han KD, Cha MJ, Oh S, Lip GY. Temporal trends of antithrombotic therapy for stroke prevention in Korean patients with non-valvular atrial fibrillation in the era of non-vitamin K antagonist oral anticoagulants: a nationwide population-based study. PLoS One. 2017; 12:e0189495.
Article89. Lee SR, Han K, Cha MJ, et al. Prevalence of non-valvular atrial fibrillation based on geographical distribution and socioeconomic status in the entire Korean population. Korean Circ J. 2018; 48:e58.
Article90. Kim H, Kim TH, Cha MJ, et al. A prospective survey of atrial fibrillation management for real-world guideline adherence: COmparison study of Drugs for symptom control and complication prEvention of Atrial Fibrillation (CODE-AF) Registry. Korean Circ J. 2017; 47:877–887.
Article91. Suzuki S, Otsuka T, Sagara K, et al. Nine-year trend of anticoagulation use, thromboembolic events, and major bleeding in patients with non-valvular atrial fibrillation - Shinken Database analysis. Circ J. 2016; 80:639–649.92. Miyazaki S, Miyauchi K, Hayashi H, et al. Registry of Japanese patients with atrial fibrillation focused on anticoagulant therapy in the new era: The RAFFINE registry study design and baseline characteristics. J Cardiol. 2018; 71:590–596.
Article93. Apostolakis S, Sullivan RM, Olshansky B, Lip GY. Factors affecting quality of anticoagulation control among patients with atrial fibrillation on warfarin: the SAMe-TT2R2 score. Chest. 2013; 144:1555–1563.94. Singer DE, Hellkamp AS, Piccini JP, et al. Impact of global geographic region on time in therapeutic range on warfarin anticoagulant therapy: data from the ROCKET AF clinical trial. J Am Heart Assoc. 2013; 2:e000067.
Article95. Wallentin L, Yusuf S, Ezekowitz MD, et al. Efficacy and safety of dabigatran compared with warfarin at different levels of international normalised ratio control for stroke prevention in atrial fibrillation: an analysis of the RE-LY trial. Lancet. 2010; 376:975–983.
Article96. Oh S, Goto S, Accetta G, et al. Vitamin K antagonist control in patients with atrial fibrillation in Asia compared with other regions of the world: Real-world data from the GARFIELD-AF registry. Int J Cardiol. 2016; 223:543–547.
Article97. Bernaitis N, Ching CK, Chen L, et al. The sex, age, medical history, treatment, tobacco use, race risk (SAMe TT2R2) score predicts warfarin control in a Singaporean population. J Stroke Cerebrovasc Dis. 2017; 26:64–69.98. Hong KS, Kim YK, Bae HJ, et al. Quality of anticoagulation with warfarin in Korean patients with atrial fibrillation and prior stroke: a multicenter retrospective observational study. J Clin Neurol. 2017; 13:273–280.
Article99. Saokaew S, Sapoo U, Nathisuwan S, Chaiyakunapruk N, Permsuwan U. Anticoagulation control of pharmacist-managed collaborative care versus usual care in Thailand. Int J Clin Pharm. 2012; 34:105–112.
Article100. Thanimalai S, Shafie AA, Hassali MA, Sinnadurai J. Comparing effectiveness of two anticoagulation management models in a Malaysian tertiary hospital. Int J Clin Pharm. 2013; 35:736–743.
Article101. Bernaitis N, Ching CK, Teo SC, et al. Factors influencing warfarin control in Australia and Singapore. Thromb Res. 2017; 157:120–125.
Article102. Yang QD, Niu Q, Zhou YH, et al. Incidence of cerebral hemorrhage in the Changsha community. A prospective study from 1986 to 2000. Cerebrovasc Dis. 2004; 17:303–313.103. Guo Y, Pisters R, Apostolakis S, et al. Stroke risk and suboptimal thromboprophylaxis in Chinese patients with atrial fibrillation: would the novel oral anticoagulants have an impact? Int J Cardiol. 2013; 168:515–522.
Article104. Gamra H, Murin J, Chiang CE, et al. Use of antithrombotics in atrial fibrillation in Africa, Europe, Asia and South America: insights from the International RealiseAF Survey. Arch Cardiovasc Dis. 2014; 107:77–87.
Article105. Huisman MV, Ma CS, Diener HC, et al. Antithrombotic therapy use in patients with atrial fibrillation before the era of non-vitamin K antagonist oral anticoagulants: the Global Registry on Long-Term Oral Antithrombotic Treatment in Patients with Atrial Fibrillation (GLORIA-AF) Phase I cohort. Europace. 2016; 18:1308–1318.
Article106. Amerena J, Chen SA, Sriratanasathavorn C, et al. Insights into management of atrial fibrillation in Asia Pacific gained from baseline data from REgistry on cardiac rhythm disORDers (RecordAF-Asia Pacific [AP]) registry. Am J Cardiol. 2012; 109:378–382.
Article107. Chang CH, Yang YH, Chen JH, Lin LJ. Cost-effectiveness of dabigatran etexilate for the prevention of stroke and systemic embolism in atrial fibrillation in Taiwan. Thromb Res. 2014; 133:782–789.
Article108. Chan EW, Lau WC, Siu CW, et al. Effect of suboptimal anticoagulation treatment with antiplatelet therapy and warfarin on clinical outcomes in patients with nonvalvular atrial fibrillation: a population-wide cohort study. Heart Rhythm. 2016; 13:1581–1588.
Article109. Chao TF, Liu CJ, Lin YJ, et al. Oral anticoagulation in very elderly patients with atrial fibrillation - a nationwide cohort study. Circulation. 2018.110. Bai Y, Guo SD, Deng H, et al. Effectiveness and safety of oral anticoagulants in older patients with atrial fibrillation: a systematic review and meta-regression analysis. Age Ageing. 2018; 47:9–17.
Article111. Sato H, Ishikawa K, Kitabatake A, et al. Low-dose aspirin for prevention of stroke in low-risk patients with atrial fibrillation: Japan Atrial Fibrillation Stroke Trial. Stroke. 2006; 37:447–451.112. Yasaka M, Lip GY. Impact of non-vitamin k antagonist oral anticoagulants on intracranial bleeding in Asian patients with non-valvular atrial fibrillation. Circ J. 2014; 78:2367–2372.
Article113. Martinez C, Katholing A, Wallenhorst C, Freedman SB. Therapy persistence in newly diagnosed non-valvular atrial fibrillation treated with warfarin or NOAC. A cohort study. Thromb Haemost. 2016; 115:31–39.114. Yao X, Abraham NS, Alexander GC, et al. Effect of adherence to oral anticoagulants on risk of stroke and major bleeding among patients with atrial fibrillation. J Am Heart Assoc. 2016; 5:e003074.
Article115. Bai Y, Wang YL, Shantsila A, Lip GY. The global burden of atrial fibrillation and stroke: a systematic review of the clinical epidemiology of atrial fibrillation in Asia. Chest. 2017; 152:810–820.116. Bai Y, Guo SD, Shantsila A, Lip GY. Modelling projections for the risks related with atrial fibrillation in East Asia: a focus on ischaemic stroke and death. Europace. 2017.
Article117. Lip GY. The ABC pathway: an integrated approach to improve AF management. Nat Rev Cardiol. 2017; 14:627–628.
Article118. Lip G, Freedman B, De Caterina R, Potpara TS. Stroke prevention in atrial fibrillation: Past, present and future. Comparing the guidelines and practical decision-making. Thromb Haemost. 2017; 117:1230–1239.119. Fauchier L, Villejoubert O, Clementy N, et al. Causes of death and influencing factors in patients with atrial fibrillation. Am J Med. 2016; 129:1278–1287.
Article120. Pokorney SD, Piccini JP, Stevens SR, et al. Cause of death and predictors of all-cause mortality in anticoagulated patients with nonvalvular atrial fibrillation: data from ROCKET AF. J Am Heart Assoc. 2016; 5:e002197.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Mechanism of and Preventive Therapy for Stroke in Patients with Atrial Fibrillation
- Prevention of stroke in atrial fibrillation
- Practical Issues to Prevent Stroke Associated with Non-valvular Atrial Fibrillation
- How and When to Screen for Atrial Fibrillation after Stroke: Insights from Insertable Cardiac Monitoring Devices
- The Primary Goal of Anticoagulation in Atrial Fibrillation to Prevent Stroke and Not to Offer the Apparently Cheapest Treatment