J Lipid Atheroscler.
2018 Jun;7(1):12-20. 10.12997/jla.2018.7.1.12.
What Do We Get from Recent Statin and CETP Inhibitors Trials?
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Diabetes & Vascular Center, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. bjjake.kim@samsung.com
- KMID: 2416254
- DOI: http://doi.org/10.12997/jla.2018.7.1.12
Abstract
- Recent clinical trials and meta-analyses have indicated that high-intensive statin treatment lowers low-density lipoprotein cholesterol (LDL-C) levels and reduces the risk of nonfatal cardiovascular (CV) events compared with moderate-intensity statin treatment. However, there are residual risks of CV events and safety concerns associated with high-intensity statin treatment. The Improved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT) study showed that ezetimibe plus moderate-intensity statin therapy after acute coronary syndromes incrementally lowers LDL-C levels and improved CV outcomes compared with moderate-intensity statin therapy. However, despite the LDL-C-lowering effects, a substantial residual CV risk still remains, which includes other lipid abnormalities such as low high-density lipoprotein cholesterol (HDL-C). The most representative agents that primarily increase HDL-C are cholesteryl ester transfer protein (CETP) inhibitors. Until now, 4 CETP inhibitors, including torcetrapib, dalcetrapib, evacetrapib, and anacetrapib, have been introduced and all have significantly raised the HDL-C from 30% to 133%. However, the results for CV outcomes in clinical trials differed, based on the 4 agents. Torcetrapib increased the risk of CV events and total mortality in patients at high CV risk (ILLUMINATE trial). Dalcetrapib and evacetrapib did not result in lower rate of CV events in patients with recent acute coronary syndrome and high risk vascular disease, respectively (dal-OUTCOMES and ACCELERATE trials). However, anacetrapib significantly decreased the incidence of major coronary events in patients with atherosclerotic vascular disease (REVEAL trial). This topic summarizes the major results of recent statin and CETP inhibitor trials and provides framework to interpret and implement the trial results in real clinical practice.
Keyword
MeSH Terms
-
Acute Coronary Syndrome
Cholesterol
Cholesterol Ester Transfer Proteins
Dyslipidemias
Ezetimibe
Ezetimibe, Simvastatin Drug Combination
Humans
Hydroxymethylglutaryl-CoA Reductase Inhibitors*
Incidence
Lipoproteins
Mortality
Vascular Diseases
Cholesterol
Cholesterol Ester Transfer Proteins
Ezetimibe
Ezetimibe, Simvastatin Drug Combination
Lipoproteins
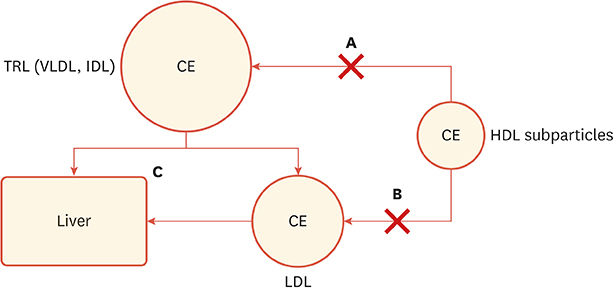
Figure
Cited by 1 articles
-
The Long and Winding Road: To the Proper Understanding of High-density Lipoprotein
Jidong Sung
Korean Circ J. 2020;50(3):248-249. doi: 10.4070/kcj.2020.0020.
Reference
-
1. Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, et al. 2016 ESC/EAS guidelines for the management of dyslipidemias. Eur Heart J. 2016; 37:2999–3058.
Article2. Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:25 Pt B. 2889–2934.
Article3. Cholesterol Treatment Trialists’ (CTT) Collaboration. Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010; 376:1670–1681.
Article4. Preiss D, Seshasai SR, Welsh P, Murphy SA, Ho JE, Waters DD, et al. Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA. 2011; 305:2556–2564.
Article5. Collins R, Reith C, Emberson J, Armitage J, Baigent C, Blackwell L, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet. 2016; 388:2532–2561.
Article6. Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndrome. N Engl J Med. 2015; 372:2387–2397.
Article7. Gordon DJ, Probstfield JL, Garrison RJ, Neaton JD, Castelli WP, Knoke JD, et al. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation. 1989; 79:8–15.
Article8. Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, et al. HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med. 2007; 357:1301–1310.
Article9. Kaur N, Pandey A, Negi H, Shafiq N, Reddy S, Kaur H, et al. Effect of HDL-raising drugs on cardiovascular outcomes: a systematic review and meta-regression. PLoS One. 2014; 9:e94585.
Article10. Tall AR, Rader DJ. Trials and tribulations of CETP inhibitors. Circ Res. 2018; 122:106–112.
Article11. Ferri N, Corsini A, Sirtori CR, Ruscica M. Present therapeutic role of cholesteryl ester transfer protein inhibitors. Pharmacol Res. 2018; 128:29–41.
Article12. Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, et al. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007; 357:2109–2122.
Article13. Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012; 367:2089–2099.
Article14. Lincoff AM, Nicholls SJ, Riesmeyer JS, Barter PJ, Brewer HB, Fox KA, et al. Evacetrapib and caradiovascular outcomes in high-risk vascular disease. N Engl J Med. 2017; 376:1933–1942.
Article15. HPS3/TIMI55–REVEAL Collaborative Group. Bowman L, Hopewell JC, Chen F, Wallendszus K, Stevens W, et al. Effects of anacetrapib in patients with atherosclerotic vascular disease. N Engl J Med. 2017; 377:1217–1227.
Article16. Tardif JC, Rhéaume E, Lemieux Perreault LP, Grégoire JC, Feroz Zada Y, Asselin G, et al. Pharmacogenomic determinants of the cardiovascular effects of dalcetrapib. Circ Cardiovasc Genet. 2015; 8:372–382.
Article17. Giugliano RP, Cannon CP, Blazing MA, Nicolau JC, Corbalán R, Špinar J, et al. Benefit of adding ezetimibe to statin therapy on cardiovascular outcomes and safety in patients with versus without diabetes mellitus: results from IMPROVE-IT. Circulation. 2018; 137:1571–1582.
Article18. Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm-2017 executive summary. Endocr Pract. 2017; 23:207–238.
Article19. Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm-2018 executive summary. Endocr Pract. 2018; 24:91–120.20. AIM-HIGH Investigators. Boden WE, Probstfield JL, Anderson T, Chaitman BR, Desvignes-Nickens P, et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011; 365:2255–2267.
Article21. Nicholls SJ, Ray KK, Ballantyne CM, Beacham LA, Miller DL, Ruotolo G, et al. Comparative effects of cholesteryl ester transfer protein inhibition, statin or ezetimibe on lipid factors: the ACCENTUATE trial. Atherosclerosis. 2017; 261:12–18.
Article22. Luo M, Liu A, Wang S, Wang T, Hu D, Wu S, et al. ApoCIII enrichment in HDL impairs HDL-mediated cholesterol efflux capacity. Sci Rep. 2017; 7:2312.
Article23. Lewis CE. Defining the safety of anacetrapib, a CETP inhibitor, in patients at high risk for coronary heart disease: the DEFINE study. Curr Cardiovasc Risk Rep. 2011; 5:109–112.
Article24. Khera AV, Cuchel M, de la Llera-Moya M, Rodrigues A, Burke MF, Jafri K, et al. Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N Engl J Med. 2011; 364:127–135.
Article25. Rohatgi A, Khera A, Berry JD, Givens EG, Ayers CR, Wedin KE, et al. HDL cholesterol efflux capacity and incident cardiovascular events. N Engl J Med. 2014; 371:2383–2393.
Article26. Simic B, Mocharla P, Crucet M, Osto E, Kratzer A, Stivala S, et al. Anacetrapib, but not evacetrapib, impairs endothelial function in CETP-transgenic mice in spite of marked HDL-C increase. Atherosclerosis. 2017; 257:186–194.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combination pharmacotherapy in lipid management
- Cholesterol Lowering Therapy in Coronary Artery Disease: With Particular Reference to Statins
- CETP(Cholesteryl Ester Transfer Protein) Deficiency Caused by Genetic Mutation in the CETP Gene in Normal Korean Population
- In the Shadow of the "Statin Festival"
- Statin Use and the Risk of All-cause Mortality