Pediatr Gastroenterol Hepatol Nutr.
2018 Jul;21(3):209-213. 10.5223/pghn.2018.21.3.209.
Incidentally Discovered Solitary Gastrointestinal Polyp with Pathological Significance in Children: Four Case Reports
- Affiliations
-
- 1Department of Pediatrics, Hanyang University College of Medicine, Seoul, Korea. kyjoo@hanyang.ac.kr
- 2Department of Pathology, Hanyang University College of Medicine, Seoul, Korea.
- KMID: 2415600
- DOI: http://doi.org/10.5223/pghn.2018.21.3.209
Abstract
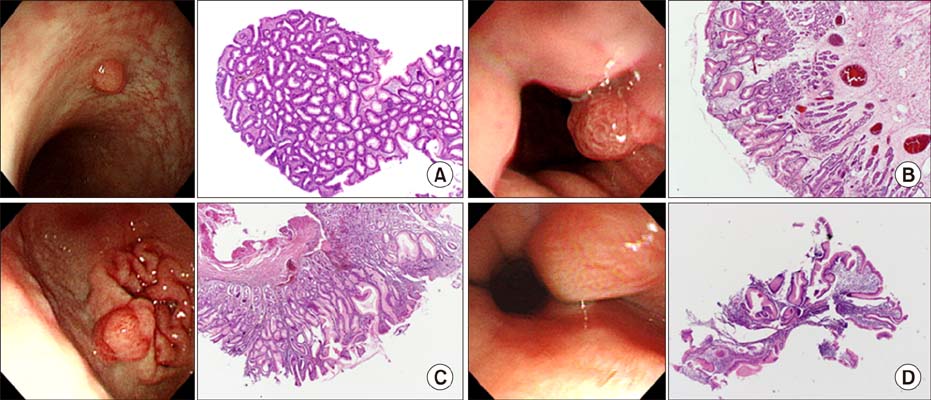
- Most solitary gastrointestinal (GI) polyps in children are either inflammatory or hamartomatous. Solitary hyperplastic polyp, sentinel polyp and solitary adenomatous polyp have been occasionally diagnosed in adults, but very rarely reported in Korean children. We recently came across a case with adenomatous polyp in the colon, a case with hyperplastic polyp beneath the gastroesophageal junction, a case with hyperplastic polyp in the prepyloric area, and a case with sentinel polyp in the distal esophagus, which are unusual pathologic types in children. These mucosal lesions were diagnosed incidentally during elective endoscopic examinations for GI symptoms. Most polyps do not cause significant symptoms, so the diagnosis might be delayed, especially in children, in whom GI endoscopy is not commonly performed for screening purpose as in the adults.
Keyword
MeSH Terms
Figure
Reference
-
1. Horrilleno EG, Eckert C, Ackerman LV. Polyps of the rectum and colon in children. Cancer. 1957; 10:1210–1220.
Article2. Friedman CJ, Fechner RE. A solitary juvenile polyp with hyperplastic and adenomatous glands. Dig Dis Sci. 1982; 27:946–948.
Article3. Goddard AF, Badreldin R, Pritchard DM, Walker MM, Warren B. on behalf of the British Society of Gastroenterology. The management of gastric polyp. Gut. 2010; 59:1270–1276.4. Dirschmid K, Platz-Baudin C, Stolte M. Why is the hyperplastic polyp a marker for the precancerous condition of the gastric mucosa? Virchows Arch. 2006; 448:80–84.
Article5. Lim MS, Seo JK, Ko JS, Yang HR, Kang GH, Kim WS. Clinical, endoscopic and pathologic findings of colonic polyposis in Korean children. Korean J Pediatr Gastroenterol Nutr. 2010; 13:154–163.
Article6. Kim JW, Song JY, Lee HK, Yun HS, Yang I, Shim JW, et al. A case of isolated adenomatous polyp of rectum in a child: tubulovillous adenoma. Korean J Pediatr Gastroenterol Nutr. 1999; 2:250–255.
Article7. Lee KS, Lee SH, Myong NH. Peutz-Jeghers syndrome with adenomatous change in a fifteen-month-old boy. Korean J Gastroenterol. 2015; 66:106–110.
Article8. Hongo M, Fujimoto K. Gastric Polyps Study Group. Incidence and risk factor of fundic gland polyp and hyperplastic polyp in long-term proton pump inhibitor therapy: a prospective study in Japan. J Gastroenterol. 2010; 45:618–624.
Article9. Pashankar DS, Israel DM. Gastric polyps and nodules in children receiving long-term omeprazole therapy. J Pediatr Gastroenterol Nutr. 2002; 35:658–662.
Article10. Ohkusa T, Takashimizu I, Fujiki K, Suzuki S, Shimoi K, Horiuchi T, et al. Disappearance of hyperplastic polyps in the stomach after eradication of Helicobacter pylori. A randomized, clinical trial. Ann Intern Med. 1998; 129:712–715.
Article11. Nakamura T, Nakano G. Histopathological classification and malignant change in gastric polyps. J Clin Pathol. 1985; 38:754–764.
Article12. Park SJ, Kim HG, Yang JH, Song HJ, Jin SY, Ryu CB, et al. A case of adenocarcinoma arising in hyperplastic polyp in the stomach. Korean J Gastrointest Endosc. 2003; 27:153–157.13. Fry LC, Lazenby AJ, Lee DH, Mönkemüller K. Signet-ring-cell adenocarcinoma arising from a hyperplastic polyp in the stomach. Gastrointest Endosc. 2005; 61:493–495.
Article14. Ryu HS, Shin SR, Kim KH, Seo GS, Choi SC. A case of a gastric hyperplastic polyp with a signet ring cell carcinoma. Korean J Gastrointest Endosc. 2008; 36:376–379.15. Han AR, Sung CO, Kim KM, Park CK, Min BH, Lee JH, et al. The clinicopathological features of gastric hyperplastic polyps with neoplastic transformations: a suggestion of indication for endoscopic polypectomy. Gut Liver. 2009; 3:271–275.
Article16. Abraham SC, Singh VK, Yardley JH, Wu TT. Hyperplastic polyps of the esophagus and esophagogastric junction: histologic and clinicopathologic findings. Am J Surg Pathol. 2001; 25:1180–1187.17. Bishop PR, Nowicki MJ, Subramony C, Parker PH. The inflammatory polyp-fold complex in children. J Clin Gastroenterol. 2002; 34:229–232.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of a Solitary Peutz-Jeghers Type Hamartomatous Polyp in the Duodenum with Upper Gastrointestinal Bleeding as the Initial Diagnosis
- Two Cases of a Solitary Peutz-Jeghers Polyp in the Rectum
- Solitary Peutz-Jeghers type harmartomatous polyp in duodenum with gastric foveolar epithelium: a case report
- Solitary Fibrous Tumor of the Adrenal Gland: A Case Report
- Solitary Peutz-Jeghers Polyp of the Colon