J Dent Anesth Pain Med.
2018 Jun;18(3):189-193. 10.17245/jdapm.2018.18.3.189.
Recurrent ST segment elevations in a patient with asymptomatic early repolarization during head and neck surgery: implications of vasospastic angina
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, University of Ulsan College of Medicine, Seoul, Korea. shkimans@amc.seoul.kr
- 2Department of Cardiology, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Dental Anesthesiology, Seoul National University Dental Hospital, Seoul, Korea.
- KMID: 2415184
- DOI: http://doi.org/10.17245/jdapm.2018.18.3.189
Abstract
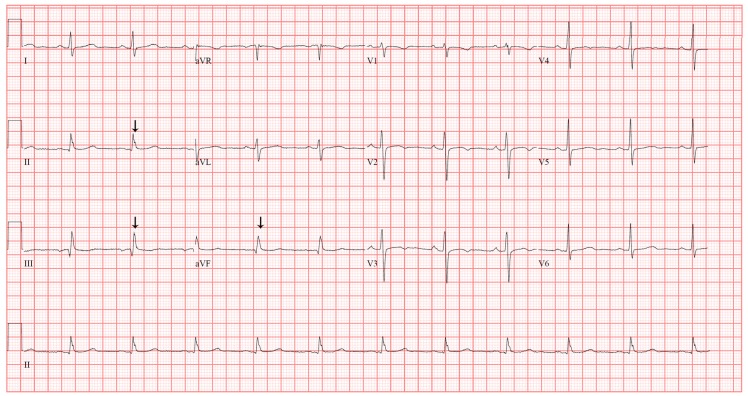
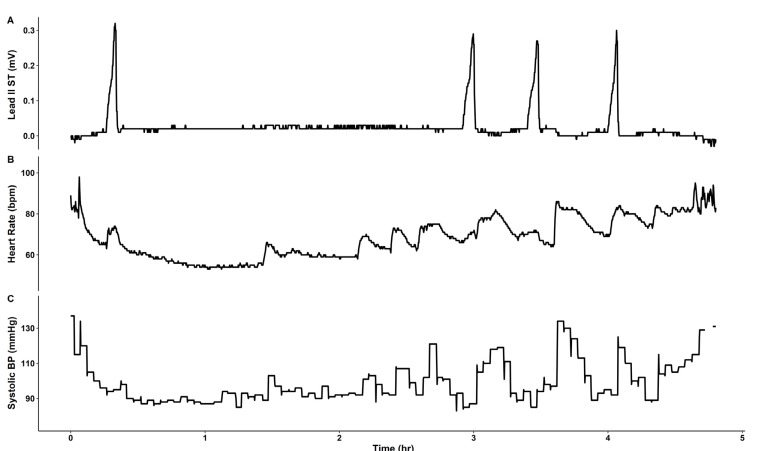
- A 57-year-old woman scheduled for cochlear implant removal exhibited preoperative electrocardiographic findings of early repolarization (ER). Four episodes of transient ST segment elevations during surgery raised suspicion for vasospastic angina (VA). In the post-anesthetic care unit, the patient complained of chest discomfort and received sublingual nitroglycerin with uncertain effect. The patient refused to proceed with postoperative invasive coronary angiography, resulting in inconclusive diagnosis. Intraoperative circumstances limit the diagnosis of VA, which emphasizes the need for further testing to confirm the diagnosis. When VA is suspected in patients with underlying ER, it is reasonable to consider invasive examination to establish the diagnosis and prevent recurrence of VA. If ST changes are observed during surgery in patients with preoperative ER, careful monitoring is recommended. Due to general anesthesia, the absence of patient symptoms limits the definitive diagnosis of those with suspected VA. Therefore, additional postoperative surveillance is recommended.
MeSH Terms
Figure
Reference
-
1. Macfarlane PW, Antzelevitch C, Haissaguerre M, Huikuri HV, Potse M, Rosso R, et al. The Early Repolarization Pattern: A Consensus Paper. J Am Coll Cardiol. 2015; 66:470–477. PMID: 26205599.2. Benito B, Guasch E, Rivard L, Nattel S. Clinical and mechanistic issues in early repolarization of normal variants and lethal arrhythmia syndromes. J Am Coll Cardiol. 2010; 56:1177–1186. PMID: 20883924.3. Rosso R, Kogan E, Belhassen B, Rozovski U, Scheinman MM, Zeltser D, et al. J-point elevation in survivors of primary ventricular fibrillation and matched control subjects: incidence and clinical significance. J Am Coll Cardiol. 2008; 52:1231–1238. PMID: 18926326.4. Sinner MF, Reinhard W, Muller M, Beckmann BM, Martens E, Perz S, et al. Association of early repolarization pattern on ECG with risk of cardiac and all-cause mortality: a population-based prospective cohort study (MONICA/KORA). PLoS Med. 2010; 7:e1000314. PMID: 20668657.
Article5. Tikkanen JT, Junttila MJ, Anttonen O, Aro AL, Luttinen S, Kerola T, et al. Early repolarization: electrocardiographic phenotypes associated with favorable long-term outcome. Circulation. 2011; 123:2666–2673. PMID: 21632493.6. Inamura Y, Nishizaki M, Shimizu M, Fujii H, Yamawake N, Suzuki M, et al. Early repolarization and positive T-wave alternans as risk markers for life-threatening arrhythmias in patients with vasospastic angina. Int J Cardiol. 2015; 196:7–13. PMID: 26070177.
Article7. Ota C, Shiono SN, Fujino Y, Kamibayashi T, Hayashi Y. Prevalence and Prognostic Value of Early Repolarization in Low Risk Surgical Patients. Biomed Res Int. 2015; 2015:309260. PMID: 26266254.
Article8. Oh CM, Oh J, Shin DH, Hwang HJ, Kim BK, Pak HN, et al. Early repolarization pattern predicts cardiac death and fatal arrhythmia in patients with vasospastic angina. Int J Cardiol. 2013; 167:1181–1187. PMID: 22483625.
Article9. Beltrame JF, Crea F, Kaski JC, Ogawa H, Ong P, Sechtem U, et al. International standardization of diagnostic criteria for vasospastic angina. Eur Heart J. 2017; 38:2565–2568. PMID: 26245334.
Article10. Rajiv A, Manjunath CN. Refractory vasospastic angina. J Cardiovasc Dis Res. 2015; 6:189–191.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Vasomotor Tone In Vasospastic Angina
- Exercise-Induced Vasospastic Angina With Prominent Regional Wall Motion Abnormality
- Diagnostic Significance of ECG Ergonovine Provocation Test in Patients with Vasospastic Angina
- ST segment
- Precordial ST-Segment Elevation in Acute Right Ventricular Myocardial Infarction