J Clin Neurol.
2018 Jul;14(3):351-358. 10.3988/jcn.2018.14.3.351.
Recurrent Optic Neuritis as the Initial Symptom in Demyelinating Diseases
- Affiliations
-
- 1Department of Neurology and Neurosurgery, Federal University of São Paulo (UNIFESP), São Paulo, SP, Brazil. alebfalcao@gmail.com
- KMID: 2415052
- DOI: http://doi.org/10.3988/jcn.2018.14.3.351
Abstract
- BACKGROUND AND PURPOSE
Optic neuritis (ON) is an inflammation of the optic nerve that can be recurrent, with unilateral or bilateral presentation. Diagnosing recurrent cases may be challenging. We aimed to compare patients with recurrent ON as their initial symptom according to their following final diagnoses: multiple sclerosis (MS), neuromyelitis optica spectrum disorders (NMOSD), or chronic relapsing inflammatory optic neuropathy (CRION).
METHODS
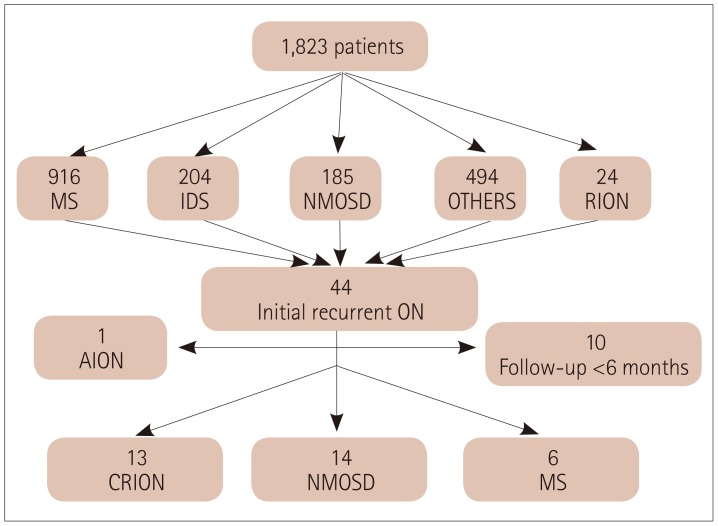
The medical records of patients with initial recurrent ON who were followed at the Neuroimmunology Clinic of the Federal University of São Paulo between 2004 and 2016 were analyzed retrospectively. Patients were classified according to their final diagnosis into MS, NMOSD, or CRION, and the characteristics of these groups were compared to identify predictive factors.
RESULTS
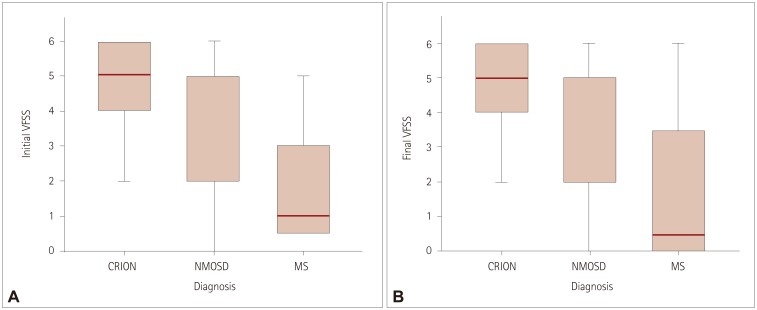
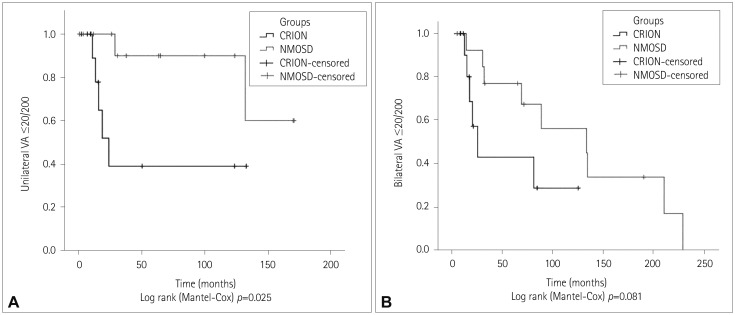
Thirty-three patients with recurrent ON were included, and 6, 14, and 13 had final diagnoses of MS, NMOSD, and CRION, respectively. Most of the patients were female with unilateral and severe ON in their first episode, and the initial Visual Functional System Score (VFSS) was ≥5 in 63.6%, 85.7%, and 16.7% of the patients with CRION, NMOSD, and MS, respectively. Anti-aquaporin-4 antibodies were detected in 9 of 21 (42.8%) tested patients. Seven of nine (77.8%) seropositive NMOSD patients experienced transverse myelitis episodes during the follow-up period. A multivariate regression analysis showed that the VFSS at the last medical appointment predicted the final diagnosis.
CONCLUSIONS
A lower VFSS at the last medical appointment was predictive of MS. Patients with NMOSD and CRION have similar clinical characteristics, whereas NMOSD patients tend to have worse visual acuity.
MeSH Terms
Figure
Reference
-
1. Optic Neuritis Study Group. Visual function 15 years after optic neuritis: a final follow-up report from the optic neuritis treatment trial. Ophthalmology. 2008; 115:1079–1082.e5. PMID: 17976727.2. Jarius S, Frederikson J, Waters P, Paul F, Akman-Demir G, Marignier R, et al. Frequency and prognostic impact of antibodies to aquaporin-4 in patients with optic neuritis. J Neurol Sci. 2010; 298:158–162. PMID: 20850793.
Article3. Hickman SJ, Dalton CM, Miller DH, Plant GT. Management of acute optic neuritis. Lancet. 2002; 360:1953–1962. PMID: 12493277.
Article4. Beck RW, Cleary PA, Anderson MM Jr, Keltner JL, Shults WT, Kaufman DI, et al. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. The Optic Neuritis Study Group. N Engl J Med. 1992; 326:581–588. PMID: 1734247.5. Abou Zeid N, Bhatti MT. Acute inflammatory demyelinating optic neuritis: evidence-based visual and neurological considerations. Neurologist. 2008; 14:207–223. PMID: 18617847.6. Benoilid A, Tilikete C, Collongues N, Arndt C, Vighetto A, Vignal C, et al. Relapsing optic neuritis: a multicentre study of 62 patients. Mult Scler. 2014; 20:848–853. PMID: 24177207.
Article7. Kidd D, Burton B, Plant GT, Graham EM. Chronic relapsing inflammatory optic neuropathy (CRION). Brain. 2003; 126:276–284. PMID: 12538397.
Article8. Matiello M, Lennon VA, Jacob A, Pittock SJ, Lucchinetti CF, Wingerchuk DM, et al. NMO-IgG predicts the outcome of recurrent optic neuritis. Neurology. 2008; 70:2197–2200. PMID: 18434643.
Article9. de Seze J, Arndt C, Jeanjean L, Zephir H, Blanc F, Labauge P, et al. Relapsing inflammatory optic neuritis: is it neuromyelitis optica? Neurology. 2008; 70:2075–2076. PMID: 18505981.10. Marignier R, De Sèze J, Vukusic S, Durand-Dubief F, Zéphir H, Vermersch P, et al. NMO-IgG and Devic's neuromyelitis optica: a French experience. Mult Scler. 2008; 14:440–445. PMID: 18208892.
Article11. Petzold A, Pittock S, Lennon V, Maggiore C, Weinshenker BG, Plant GT. Neuromyelitis optica-IgG (aquaporin-4) autoantibodies in immune mediated optic neuritis. J Neurol Neurosurg Psychiatry. 2010; 81:109–111. PMID: 20019228.
Article12. Petzold A, Plant GT. Chronic relapsing inflammatory optic neuropathy: a systematic review of 122 cases reported. J Neurol. 2014; 261:17–26. PMID: 23700317.
Article13. Collongues N, Marignier R, Zéphir H, Blanc F, Vukusic S, Outteryck O, et al. High-risk syndrome for neuromyelitis optica: a descriptive and comparative study. Mult Scler. 2011; 17:720–724. PMID: 21239412.
Article14. Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011; 69:292–302. PMID: 21387374.
Article15. Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015; 85:177–189. PMID: 26092914.
Article16. Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983; 33:1444–1452. PMID: 6685237.
Article17. Papais-Alvarenga RM, Carellos SC, Alvarenga MP, Holander C, Bichara RP, Thuler LC. Clinical course of optic neuritis in patients with relapsing neuromyelitis optica. Arch Ophthalmol. 2008; 126:12–16. PMID: 18195212.
Article18. Swanton JK, Fernando KT, Dalton CM, Miszkiel KA, Altmann DR, Plant GT, et al. Early MRI in optic neuritis: the risk for clinically definite multiple sclerosis. Mult Scler. 2010; 16:156–165. PMID: 20086028.
Article19. Biotti D, Bonneville F, Tournaire E, Ayrignac X, Dallière CC, Mahieu L, et al. Optic neuritis in patients with anti-MOG antibodies spectrum disorder: MRI and clinical features from a large multicentric cohort in France. J Neurol. 2017; 264:2173–2175. PMID: 28914353.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Optic neuritis and multiple cranial neuropathies in patient with chronic inflammatory demyelinating polyneuropathy
- Clinical Characteristics of Optic Neuritis according to the Presence of Abnormal MRI Lesions
- Subacute Inflammatory Demyelinating Polyneuropathy Combined with Optic Neuritis
- Reversible Bilateral Optic Neuritis with No Light Perception
- Transocular Ultrasonography in Central Nervous System (CNS) Demyelinating Disease: A Narrative Review of the Clinical Utility in Optic Neuritis and CNS Demyelinating Disease