Imaging Sci Dent.
2018 Jun;48(2):147-152. 10.5624/isd.2018.48.2.147.
Temporomandibular joint synovial chondromatosis accompanying temporal bone proliferation: A case report
- Affiliations
-
- 1Department of Oral and Maxillofacial Radiology, Dankook University College of Dentistry, Cheonan, Korea. wjhan@dankook.ac.kr
- 2Department of Pathology, Dankook University College of Medicine, Cheonan, Korea.
- KMID: 2413927
- DOI: http://doi.org/10.5624/isd.2018.48.2.147
Abstract
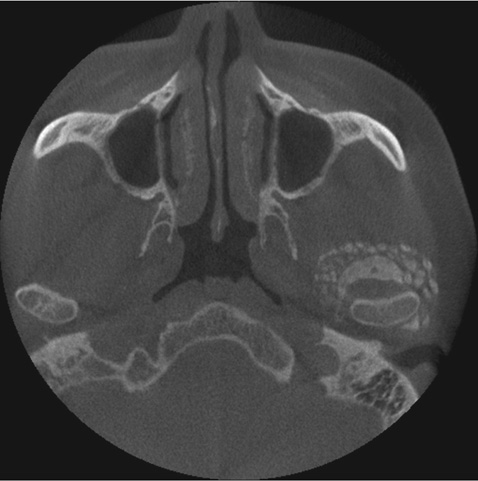
- Synovial chondromatosis is a rare metaplastic disease affecting the joints, including the temporomandibular joint (TMJ). Since its symptoms are similar to those of temporomandibular disorders, a careful differential diagnosis is essential. A 50-year-old male patient was referred with the chief complaint of pain and radiopaque masses around the left TMJ on panoramic radiography. Clinically, pre-auricular swelling and resting pain was found, without limitation of mouth opening. On cone-beam computed tomographic images, multiple calcified nodules adjacent to the TMJ and bone proliferation with sclerosis at the articular fossa and eminence were found. T2-weighted magnetic resonance images showed multiple signal-void nodules with high signal effusion in the superior joint space and thickened cortical bone at the articular fossa and eminence. The calcified nodules were removed by surgical excision, but the hypertrophic articular fossa and eminence remained. A histopathological examination confirmed the diagnosis. The patient was followed up few months later without recurrence.
Keyword
MeSH Terms
Figure
Reference
-
1. Schulte WC, Rhyne RR. Synovial chondromatosis of temporomandibular joint. Report of a case. Oral Surg Oral Med Oral Pathol. 1969; 28:906–913.2. Tamimi D, Hatcher D. Specialty imaging. Temporomandibular joint. Philadelphia, PA: Elsevier;2016. p. 530–533.3. Testaverde L, Perrone A, Caporali L, Ermini A, Izzo L, D'Angeli I, et al. CT and MR findings in synovial chondromatosis of the temporo-mandibular joint: our experience and review of literature. Eur J Radiol. 2011; 78:414–418.
Article4. Ida M, Yoshitake H, Okoch K, Tetsumura A, Ohbayashi N, Amagasa T, et al. An investigation of magnetic resonance imaging features in 14 patients with synovial chondromatosis of the temporomandibular joint. Dentomaxillofac Radiol. 2008; 37:213–219.
Article5. von Lindern JJ, Theuerkauf I, Niederhagen B, Bergé S, Appel T, Reich RH. Synovial chondromatosis of the temporomandibular joint: clinical, diagnostic, and histomorphologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94:31–38.
Article6. Matsumoto K, Sato T, Iwanari S, Kameoka S, Oki H, Komiyama K, et al. The use of arthrography in the diagnosis of temporomandibular joint synovial chondromatosis. Dentomaxillofac Radiol. 2013; 42:15388284.
Article7. Liu X, Huang Z, Zhu W, Liang P, Tao Q. Clinical and imaging findings of temporomandibular joint synovial chondromatosis: an analysis of 10 cases and literature review. J Oral Maxillofac Surg. 2016; 74:2159–2168.
Article8. Meng J, Guo C, Yi B, Zhao Y, Luo H, Ma X. Clinical and radiologic findings of synovial chondromatosis affecting the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:441–448.
Article9. Lim SW, Jeon SJ, Choi SS, Choi KH. Synovial chondromatosis in the temporomandibular joint: a case with typical imaging features and pathological findings. Br J Radiol. 2011; 84:e213–e216.
Article10. Yu Q, Yang J, Wang P, Shi H, Luo J. CT features of synovial chondromatosis in the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 97:524–528.
Article11. Wang P, Tian Z, Yang J, Yu Q. Synovial chondromatosis of the temporomandibular joint: MRI findings with pathological comparison. Dentomaxillofac Radiol. 2012; 41:110–116.
Article12. Villacin AB, Brigham LN, Bullough PG. Primary and secondary synovial chondrometaplasia: histopathologic and clinicoradiologic differences. Hum Pathol. 1979; 10:439–451.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary synovial chondromatosis of the temporomandibular joint with temporal involvement
- CASE REPORT OF SYNOVIAL CHONDROMATOSIS IN THE TEMPOROMANDIBULAR JOINT
- Articular loose body, Synovial Chondromatosis of the Temporomandibular Joint: a Case Report
- Temporomandibular joint synovial chondromatosis extending to the temporal bone: a report of two cases
- A clinical Study of Synovial Chondromatosis