J Korean Assoc Oral Maxillofac Surg.
2017 Oct;43(5):336-342. 10.5125/jkaoms.2017.43.5.336.
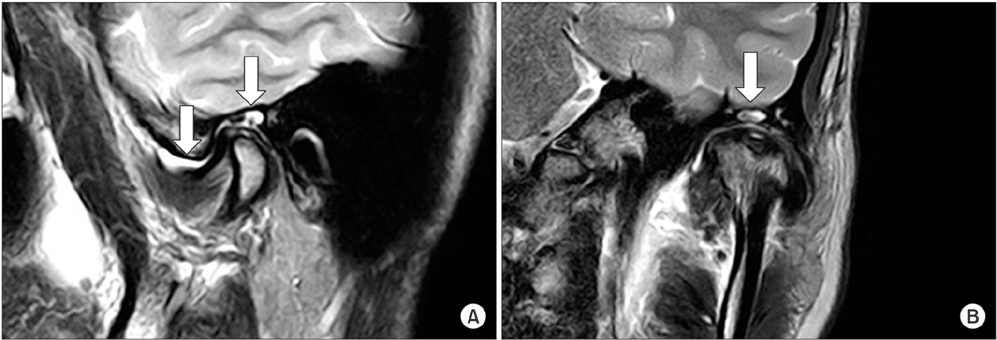
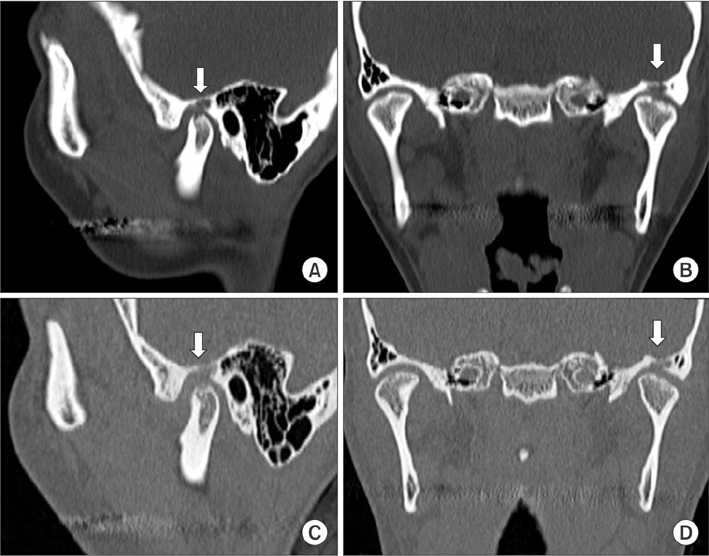
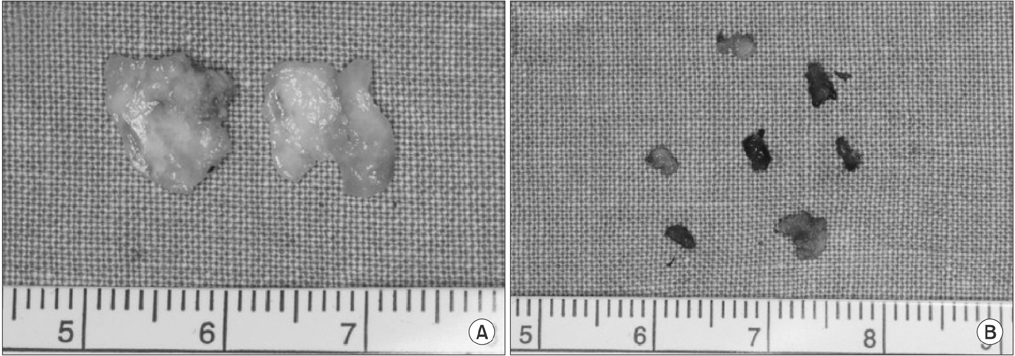
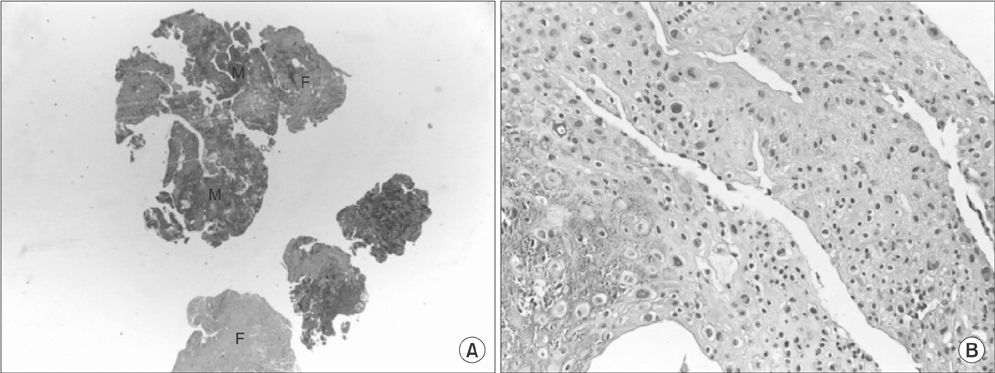
Temporomandibular joint synovial chondromatosis extending to the temporal bone: a report of two cases
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Gangnam Severance Hospital, Yonsei University College of Dentistry, Seoul, Korea. omshuh@yuhs.ac
- 2Department of Oral Pathology, Oral Cancer Research Institute, Yonsei University College of Dentistry, Seoul, Korea.
- 3Department of Oral and Maxillofacial Radiology, Yonsei University College of Dentistry, Seoul, Korea.
- 4Department of Dentistry, Yongin Severance Hospital, Yongin, Korea.
- KMID: 2393600
- DOI: http://doi.org/10.5125/jkaoms.2017.43.5.336
Abstract
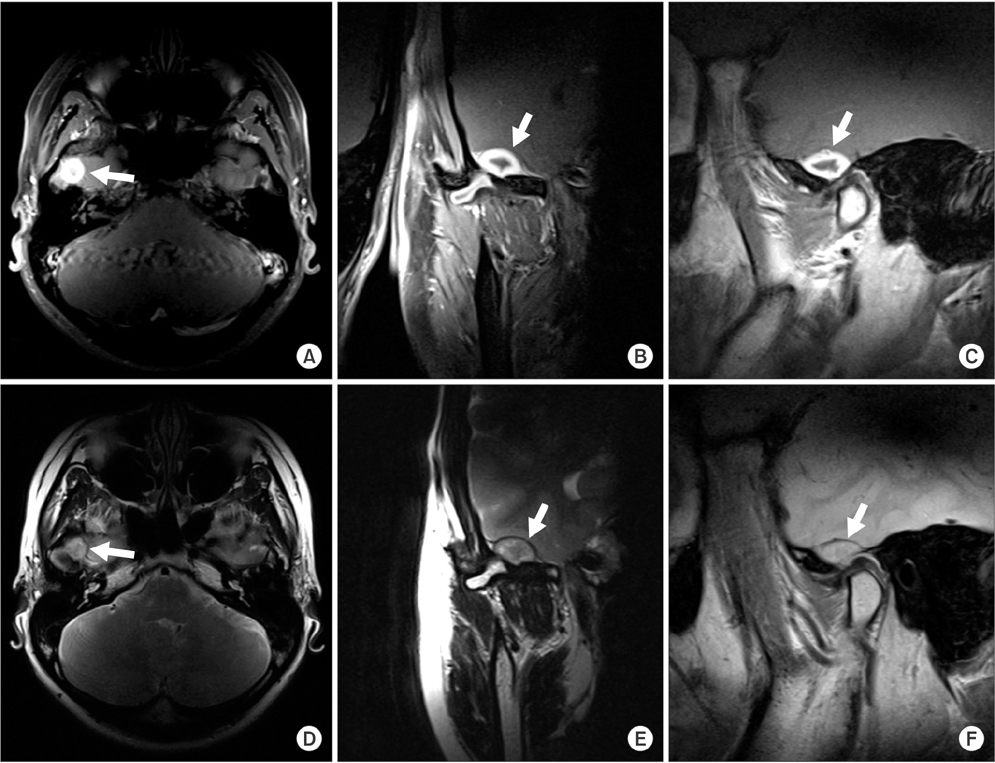
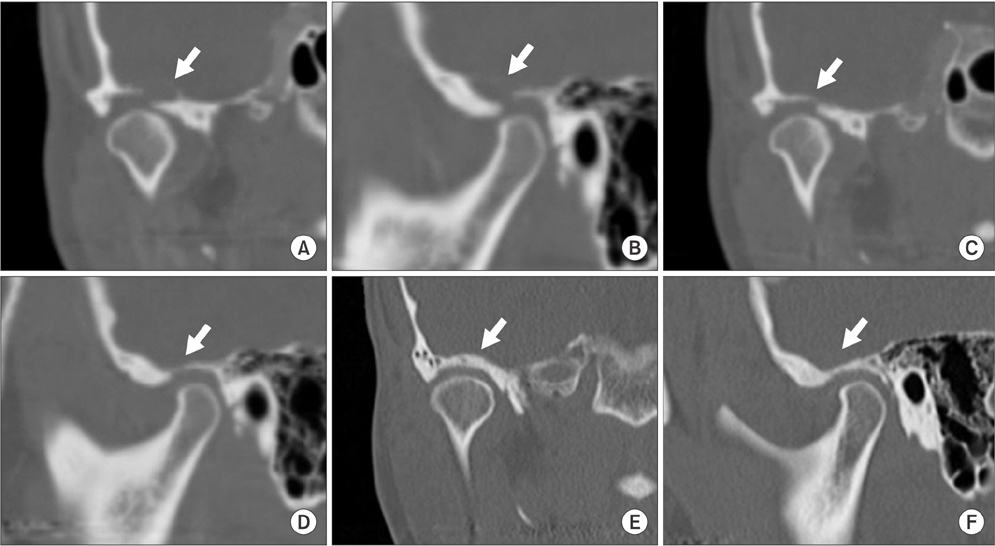
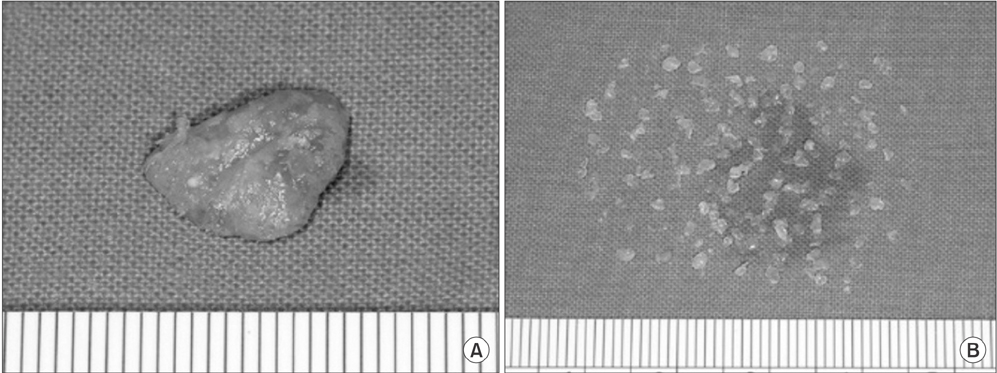
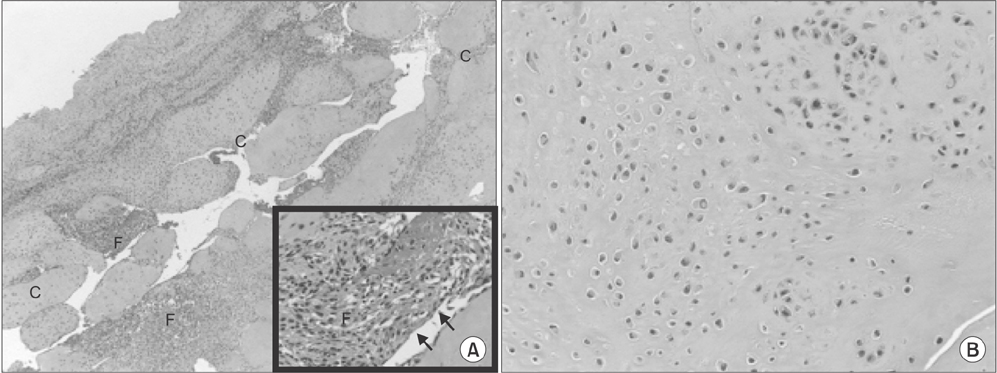
- Synovial chondromatosis is a rare benign lesion originating from the synovial membrane. It presents as adhesive or non-adhesive intra-articular cartilaginous loose bodies. Although the causes of synovial chondromatosis have not been fully elucidated, inflammation, external injury, or excessive use of joints have been suggested as possible causes. Synovial chondromatosis has been reported to occur most frequently at large joints that bear weights, with a rare occurrence at the temporomandibular joint (TMJ). When synovial chondromatosis develops at TMJ, clinical symptoms, including pain, joint sounds, and mouth opening may common. Moreover, synovial chondromatosis rarely spreads to the mandibular condyle, glenoid cavity, or articular eminence of TMJ. The goal of this study was to discuss the methods of surgery and other possible considerations by reviewing cases of patients who underwent surgery for synovial chondromatosis that extended to the temporal bone.
MeSH Terms
Figure
Reference
-
1. Akhtar M, Mahajan S, Kott E. Synovial chondromatosis of the temporomandibular joint. J Bone Joint Surg Am. 1977; 59:266–267.
Article2. von Lindern JJ, Theuerkauf I, Niederhagen B, Bergé S, Appel T, Reich RH. Synovial chondromatosis of the temporomandibular joint: clinical, diagnostic, and histomorphologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94:31–38.
Article3. Karlis V, Glickman RS, Zaslow M. Synovial chondromatosis of the temporomandibular joint with intracranial extension. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998; 86:664–666.
Article4. Ardekian L, Faquin W, Troulis MJ, Kaban LB, August M. Synovial chondromatosis of the temporomandibular joint: report and analysis of eleven cases. J Oral Maxillofac Surg. 2005; 63:941–947.
Article5. Quinn PD, Stanton DC, Foote JW. Synovial chondromatosis with cranial extension. Oral Surg Oral Med Oral Pathol. 1992; 73:398–402.
Article6. Simon GT, Kendrick RW, Whitlock RI. Osteochondroma of the mandibular condyle. Case report and its management. Oral Surg Oral Med Oral Pathol. 1977; 43:18–24.7. Lustmann J, Zeltser R. Synovial chondromatosis of the temporomandibular joint. Review of the literature and case report. Int J Oral Maxillofac Surg. 1989; 18:90–94.8. Hammodeh N, Nasser NA. Synovial chondromatosis of the temporomandibular joint, presenting as parotid mass. J Laryngol Otol. 2006; 120:e40.
Article9. Cannon CR. Osteochondrosis of the temporomandibular joint presenting as an apparent parotid mass. Ann Otol Rhinol Laryngol. 1987; 96:330–332.
Article10. Allias-Montmayeur F, Durroux R, Dodart L, Combelles R. Tumours and pseudotumorous lesions of the temporomandibular joint: a diagnostic challenge. J Laryngol Otol. 1997; 111:776–781.
Article11. Balliu E, Medina V, Vilanova J, Peláez I, Puig J, Trull JM, et al. Synovial chondromatosis of the temporomandibular joint: CT and MRI findings. Dentomaxillofac Radiol. 2007; 36:55–58.
Article12. Wong WC, Cheng PW, Chan FL. MRI appearance of synovial chondromatosis in the temporomandibular joint. Clin Radiol. 2001; 56:773–774.
Article13. Koyama J, Ito J, Hayashi T, Kobayashi F. Synovial chondromatosis in the temporomandibular joint complicated by displacement and calcification of the articular disk: report of two cases. AJNR Am J Neuroradiol. 2001; 22:1203–1206.14. Herzog S, Mafee M. Synovial chondromatosis of the TMJ: MR and CT findings. AJNR Am J Neuroradiol. 1990; 11:742–745.15. Kim HG, Park KH, Huh JK, Song YB, Choi HS. Magnetic resonance imaging characteristics of synovial chondromatosis of the temporomandibular joint. J Orofac Pain. 2002; 16:148–153.16. Milgram JW. Synovial osteochondromatosis: a histopathological study of thirty cases. J Bone Joint Surg Am. 1977; 59:792–801.17. Hallam P, Ashwood N, Cobb J, Fazal A, Heatley W. Malignant transformation in synovial chondromatosis of the knee? Knee. 2001; 8:239–242.
Article18. Lieger O, Zix J, Stauffer-Brauch EJ, Iizuka T. Synovial chondromatosis of the temporomandibular joint with cranial extension: a case report and literature review. J Oral Maxillofac Surg. 2007; 65:2073–2080.
Article19. Huh JK, Park JY, Lee S, Lee SH, Choi SW. Synovial chondromatosis of the temporomandibular joint with condylar extension. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:e83–e88.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary synovial chondromatosis of the temporomandibular joint with temporal involvement
- CASE REPORT OF SYNOVIAL CHONDROMATOSIS IN THE TEMPOROMANDIBULAR JOINT
- Articular loose body, Synovial Chondromatosis of the Temporomandibular Joint: a Case Report
- A clinical Study of Synovial Chondromatosis
- Synovial Chondromatosis