Ultrasonographic Echogenicity and Histopathologic Correlation of Thyroid Nodules in Core Needle Biopsy Specimens
- Affiliations
-
- 1Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul 03080, Korea.
- 2Department of Radiology, GangNeung Asan Hospital, University of Ulsan College of Medicine, Gangneung 25440, Korea. nndgna@gmail.com
- 3Department of Radiology, Human Medical Imaging and Intervention Center, Seoul 06524, Korea.
- 4Department of Pathology, Ewha Clinical Laboratory, Seoul 06312, Korea.
- KMID: 2413696
- DOI: http://doi.org/10.3348/kjr.2018.19.4.673
Abstract
OBJECTIVE
To determine the histopathologic features associated with ultrasonographic echogenicity of thyroid nodules.
MATERIALS AND METHODS
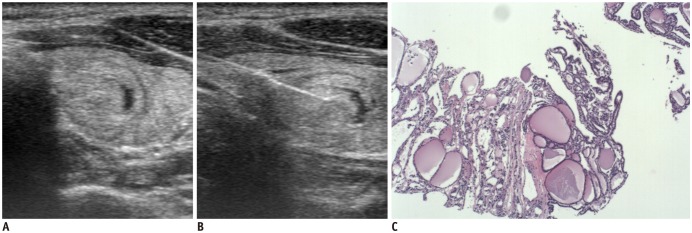
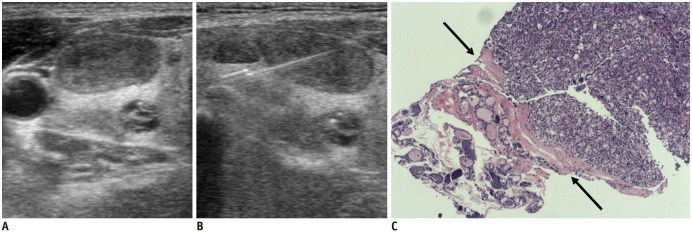
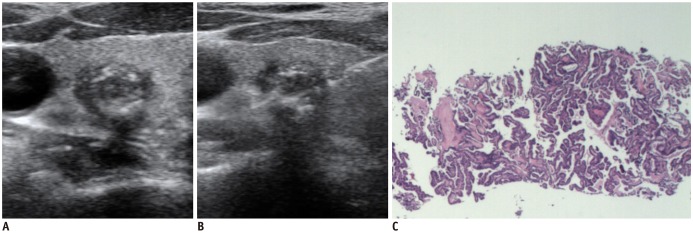
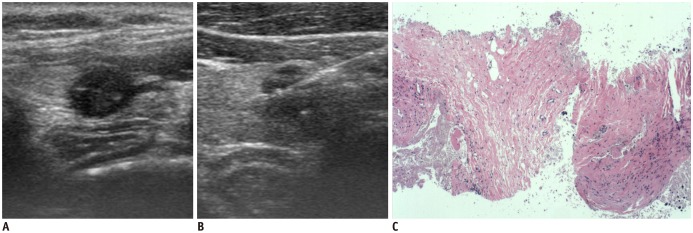
This study included 95 nodules of 95 patients (76 women, 19 men; mean age 47.5 ± 12.9 years) with homogeneous echogenicity in which core needle biopsy was performed during a one year period. The nodule echogenicity was categorized into 4 grades (hyperechogenicity, isoechogenicity, mild hypoechogenicity, and marked hypoechogenicity). The biopsy specimens were evaluated by a pathologist regarding the histopathologic features of fibrosis, lymphoid infiltration, microfollicular pattern, uniform follicular pattern, and hypercellularity in nodules. We evaluated the association of each histopathologic feature among 3 categories of nodule echogenicity by multinomial regression analysis.
RESULTS
The nodule echogenicity was isoechoic in 28 (29.5%), mildly hypoechoic in 37 (38.9%), and markedly hypoechoic in 30 (31.6%), and there was no hyperechoic nodule. There was a trend of increasing frequency of fibrosis (> 30%) as nodule echogenicity decreased (isoechogenicity, 10.7%; mild hypoechogenicity, 32.4%; and marked hypoechogenicity, 80%; p < 0.001). The microfollicular pattern, uniform follicular pattern, and hypercellularity were frequently found in mildly hypoechoic nodules than in isoechoic nodules (p ≤ 0.018). The fibrosis (> 30%) and hypercellularity were independently associated with mild or marked hypoechogenicity as compared to isoechogenicity (fibrosis; p ≤ 0.004 and hypercellularity; p ≤ 0.036), and only fibrosis (> 30%) was independently associated with marked hypoechogenicity as compared to mild hypoechogenicity (p = 0.004).
CONCLUSION
The fibrosis (> 30%) and high cellularity are independently associated with mild or marked hypoechogenicity of nodules. The knowledge of the relationship of echogenicity and histopathology of thyroid nodules could improve management of patients with thyroid nodules.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Ultrasound-Guided Core Needle Biopsy Techniques for Intermediate or Low Suspicion Thyroid Nodules: Which Method is Effective for Diagnosis?
Soo Yeon Hahn, Jung Hee Shin, Young Lyun Oh, Ko Woon Park
Korean J Radiol. 2019;20(10):1454-1461. doi: 10.3348/kjr.2018.0841.Degenerating Thyroid Nodules: Ultrasound Diagnosis, Clinical Significance, and Management
Jie Ren, Jung Hwan Baek, Sae Rom Chung, Young Jun Choi, Chan Kwon Jung, Jeong Hyun Lee
Korean J Radiol. 2019;20(6):947-955. doi: 10.3348/kjr.2018.0599.Usage and Diagnostic Yield of Fine-Needle Aspiration Cytology and Core Needle Biopsy in Thyroid Nodules: A Systematic Review and Meta-Analysis of Literature Published by Korean Authors
Soon-Hyun Ahn
Clin Exp Otorhinolaryngol. 2021;14(1):116-130. doi: 10.21053/ceo.2020.00199.
Reference
-
1. Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, et al. Thyroid Study Group, Korean Society of Neuro- and Head and Neck Radiology. Benign and malignant thyroid nodules: US differentiation--multicenter retrospective study. Radiology. 2008; 247:762–777. PMID: 18403624.
Article2. Na DG, Baek JH, Sung JY, Kim JH, Kim JK, Choi YJ, et al. Thyroid imaging reporting and data system risk stratification of thyroid nodules: categorization based on solidity and echogenicity. Thyroid. 2016; 26:562–572. PMID: 26756476.
Article3. Ha EJ, Moon WJ, Na DG, Lee YH, Choi N, Kim SJ, et al. A multicenter prospective validation study for the Korean thyroid imaging reporting and data system in patients with thyroid nodules. Korean J Radiol. 2016; 17:811–821. PMID: 27587972.
Article4. Middleton WD, Teefey SA, Reading CC, Langer JE, Beland MD, Szabunio MM, et al. Multiinstitutional analysis of thyroid nodule risk stratification using the American College of radiology thyroid imaging reporting and data system. AJR Am J Roentgenol. 2017; 208:1331–1341. PMID: 28402167.
Article5. Russ G, Bonnema SJ, Erdogan MF, Durante C, Ngu R, Leenhardt L. European Thyroid Association Guidelines for ultrasound malignancy risk stratification of thyroid nodules in adults: the EU-TIRADS. Eur Thyroid J. 2017; 6:225–237. PMID: 29167761.
Article6. Chen SJ, Yu SN, Tzeng JE, Chen YT, Chang KY, Cheng KS, et al. Characterization of the major histopathological components of thyroid nodules using sonographic textural features for clinical diagnosis and management. Ultrasound Med Biol. 2009; 35:201–208. PMID: 19010588.
Article7. Jung SL, Jung CK, Kim SH, Kang BJ, Ahn KJ, Kim BS, et al. Histopathologic findings related to the indeterminate or inadequate results of fine-needle aspiration biopsy and correlation with ultrasonographic findings in papillary thyroid carcinomas. Korean J Radiol. 2010; 11:141–148. PMID: 20191060.
Article8. Na DG, Min HS, Lee H, Won JK, Seo HB, Kim JH. Role of core needle biopsy in the management of atypia/follicular lesion of undetermined significance thyroid nodules: comparison with repeat fine-needle aspiration in subcategory nodules. Eur Thyroid J. 2015; 4:189–196. PMID: 26558236.
Article9. Na DG, Baek JH, Jung SL, Kim JH, Sung JY, Kim KS, et al. Core needle biopsy of the thyroid: 2016 Consensus Statement and Recommendations from Korean Society of Thyroid Radiology. Korean J Radiol. 2017; 18:217–237. PMID: 28096731.
Article10. Baek JH. Current status of core needle biopsy of the thyroid. Ultrasonography. 2017; 36:83–85. PMID: 28301922.
Article11. Jung CK, Min HS, Park HJ, Song DE, Kim JH, Park SY, et al. Korean Endocrine Pathology Thyroid Core Needle Biopsy Study Group. Pathology reporting of thyroid core needle biopsy: a proposal of the Korean Endocrine Pathology Thyroid Core Needle Biopsy Study Group. J Pathol Transl Med. 2015; 49:288–299. PMID: 26081825.
Article12. Rosai J, Carcangiu ML, DeLelli RA. Atlas of tumor pathology: tumors of the thyroid gland. Washington, DC: Armed Forces Institute of Pathology;1992. p. 21–63.13. Rumack CM, Wilson SR, Charboneau JW, Johnson JM. Diagnostic ultrasound. 3rd ed. St Louis, MO: Mosby;2005. p. 3–34.14. Jung CK, Baek JH. Recent advances in core needle biopsy for thyroid nodules. Endocrinol Metab (Seoul). 2017; 32:407–441. PMID: 29271614.
Article15. Isarangkul W. Dense fibrosis. Another diagnostic criterion for papillary thyroid carcinoma. Arch Pathol Lab Med. 1993; 117:645–664. PMID: 8503738.16. Ko MS, Jeong KS, Shong YK, Gong GY, Baek JH, Lee JH. Collapsing benign cystic nodules of the thyroid gland: sonographic differentiation from papillary thyroid carcinoma. AJNR Am J Neuroradiol. 2012; 33:124–127. PMID: 22158923.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thyroid Nodules with Nondiagnostic FNA Results: Role of Core Needle Biopsy
- Effectiveness and Limitations of Core Needle Biopsy in the Diagnosis of Thyroid Nodules: Review of Current Literature
- Thyroid nodules with discordant results of ultrasonographic and fine-needle aspiration findings
- Surgical Management of Bleeding from the Superior Thyroid Artery after Core Needle Biopsy
- Malignant-looking thyroid nodules with size reduction: core needle biopsy results