Ann Hepatobiliary Pancreat Surg.
2018 May;22(2):150-155. 10.14701/ahbps.2018.22.2.150.
A huge intraductal papillary neoplasm of the bile duct treated by right trisectionectomy after right portal vein embolization
- Affiliations
-
- 1Division of Hepato-Biliary-Pancreatic and Transplant Surgery, Department of Surgery, Graduate School of Medicine, Kyoto University, Kyoto, Japan. kent@kuhp.kyoto-u.ac.jp
- 2Department of Surgery, Mansoura University, Mansoura, Egypt.
- KMID: 2412430
- DOI: http://doi.org/10.14701/ahbps.2018.22.2.150
Abstract
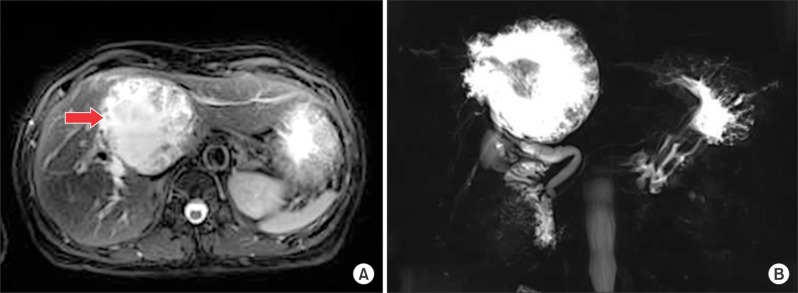
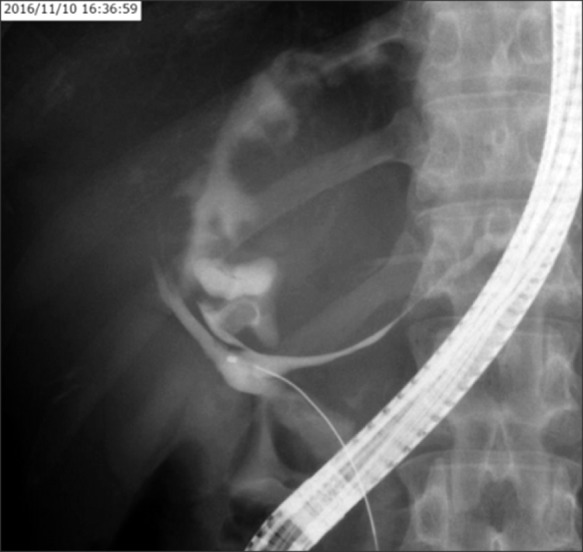
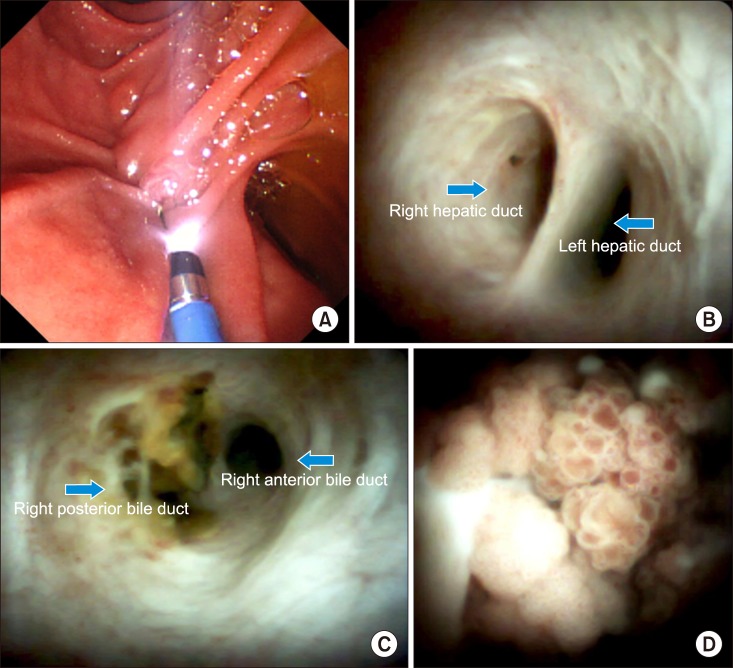
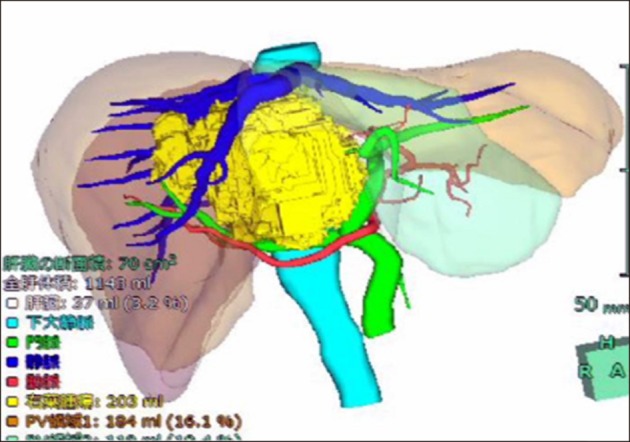
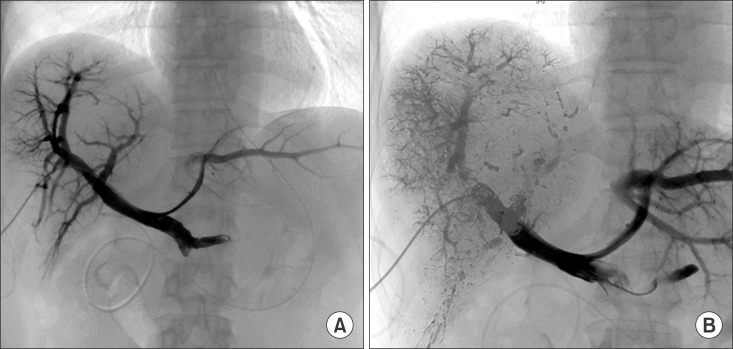
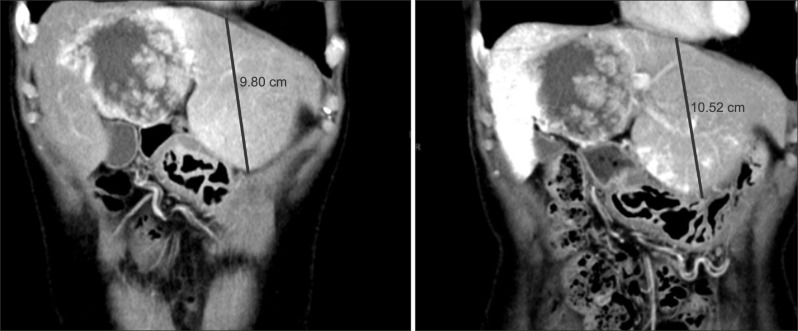
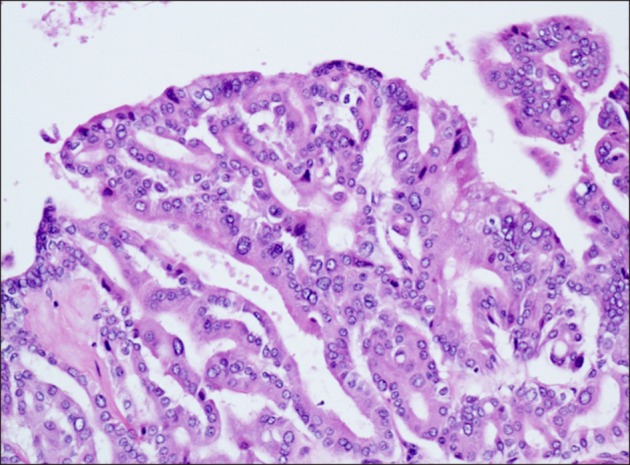
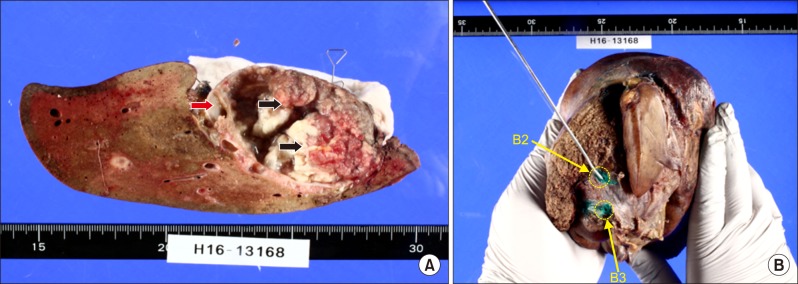
- Intraductal papillary neoplasm of the bile duct (IPNB) is a rare variant of bile duct tumors characterized by papillary growth within the bile duct lumen and recognized precursor of invasive carcinoma. IPNB was detected incidentally in a 60-year-old woman during check up. Radiologic images revealed a huge cystic mass with papillary projection and markedly dilated bile ducts. Biopsies revealed high-grade IPNB. Cholangioscopy detected a connection between the right posterior bile duct and cyst lumen with epithelial dysplasia of the bile duct. Right posterior sectional duct opened in the left hepatic duct. Consequently, right trisectionectomy and extrahepatic bile duct resection were conducted. Histological studies revealed intraductal papillary neoplasm with high-grade intraepithelial neoplasia (carcinoma in situ). IPNB patients without distant metastases are candidates for surgery and complete resection should be conducted to achieve long-term survival.
Keyword
MeSH Terms
Figure
Reference
-
1. Shibahara H, Tamada S, Goto M, Oda K, Nagino M, Nagasaka T, et al. Pathologic features of mucin-producing bile duct tumors: two histopathologic categories as counterparts of pancreatic intraductal papillary-mucinous neoplasms. Am J Surg Pathol. 2004; 28:327–338. PMID: 15104295.2. Nakanuma Y, Curabo MP, Franceschi S, Gores G, Paradis V, Sripa B. WHO classification of tumours of the digestive system. Lyon: IARC;2010. p. 217–224.3. Ohtsuka M, Shimizu H, Kato A, Yoshitomi H, Furukawa K, Tsuyuguchi T, et al. Intraductal papillary neoplasms of the bile duct. Int J Hepatol. 2014; 2014:459091. PMID: 24949206.
Article4. Barton JG, Barrett DA, Maricevich MA, Schnelldorfer T, Wood CM, Smyrk TC, et al. Intraductal papillary mucinous neoplasm of the biliary tract: a real disease? HPB (Oxford). 2009; 11:684–691. PMID: 20495637.
Article5. Kim KM, Lee JK, Shin JU, Lee KH, Lee KT, Sung JY, et al. Clinicopathologic features of intraductal papillary neoplasm of the bile duct according to histologic subtype. Am J Gastroenterol. 2012; 107:118–125. PMID: 21946282.
Article6. Aoki S, Okayama Y, Kitajima Y, Hayashi K, Imai H, Okamoto T, et al. Intrahepatic biliary papilloma morphologically similar to biliary cystadenoma. J Gastroenterol Hepatol. 2005; 20:321–324. PMID: 15683443.
Article7. Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. Lyon: IARC;2010. p. 3–8.8. Zen Y, Fujii T, Itatsu K, Nakamura K, Minato H, Kasashima S, et al. Biliary papillary tumors share pathological features with intraductal papillary mucinous neoplasm of the pancreas. Hepatology. 2006; 44:1333–1343. PMID: 17058219.
Article9. Wan XS, Xu YY, Qian JY, Yang XB, Wang AQ, He L, et al. Intraductal papillary neoplasm of the bile duct. World J Gastroenterol. 2013; 19:8595–8604. PMID: 24379576.
Article10. Ohtsuka M, Kimura F, Shimizu H, Yoshidome H, Kato A, Yoshitomi H, et al. Similarities and differences between intraductal papillary tumors of the bile duct with and without macroscopically visible mucin secretion. Am J Surg Pathol. 2011; 35:512–521. PMID: 21412069.
Article11. Tan Y, Milikowski C, Toribio Y, Singer A, Rojas CP, Garcia-Buitrago MT. Intraductal papillary neoplasm of the bile ducts: a case report and literature review. World J Gastroenterol. 2015; 21:12498–12504. PMID: 26604656.
Article12. Lee SS, Kim MH, Lee SK, Jang SJ, Song MH, Kim KP, et al. Clinicopathologic review of 58 patients with biliary papillomatosis. Cancer. 2004; 100:783–793. PMID: 14770435.
Article13. Yoon KH, Ha HK, Kim CG, Roh BS, Yun KJ, Chae KM, et al. Malignant papillary neoplasms of the intrahepatic bile ducts: CT and histopathologic features. AJR Am J Roentgenol. 2000; 175:1135–1139. PMID: 11000178.14. Sakai Y, Tsuyuguchi T, Ishihara T, Sugiyama H, Miyakawa K, Yasui S, et al. Usefulness of peroral cholangioscopy in preoperative diagnosis of intraductal papillary neoplasm of the bile duct. Hepatogastroenterology. 2010; 57:691–693. PMID: 21033211.15. Schlitter AM, Born D, Bettstetter M, Specht K, Kim-Fuchs C, Riener MO, et al. Intraductal papillary neoplasms of the bile duct: stepwise progression to carcinoma involves common molecular pathways. Mod Pathol. 2014; 27:73–86. PMID: 23828315.
Article16. Paik KY, Heo JS, Choi SH, Choi DW. Intraductal papillary neoplasm of the bile ducts: the clinical features and surgical outcome of 25 cases. J Surg Oncol. 2008; 97:508–512. PMID: 18314868.
Article17. Hokuto D, Nomi T, Yasuda S, Yoshikawa T, Ishioka K, Yamada T, et al. Long-term observation and treatment of a widespread intraductal papillary neoplasm of the bile duct extending from the intrapancreatic bile duct to the bilateral intrahepatic bile duct: A case report. Int J Surg Case Rep. 2017; 38:166–171. PMID: 28763696.
Article18. Kubota K, Nakanuma Y, Kondo F, Hachiya H, Miyazaki M, Nagino M, et al. Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: a multi-institutional study by the Japan Biliary Association. J Hepatobiliary Pancreat Sci. 2014; 21:176–185. PMID: 23908126.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intrahepatic and extrahepatic intraductal papillary neoplasms of bile duct
- Extrahepatic Bile Duct Duplication with Intraductal Papillary Neoplasm: A Case Report
- Right trisectionectomy with en bloc portal vein resection for perihilar cholangiocarcinoma after preoperative left portal vein stenting and sequential right portal and hepatic vein embolization
- Photodynamic Therapy Followed by Left Hepatectomy Used to Treat an Intraductal Papillary Mucinous Neoplasm of the Bile Duct
- Caroli's disease misdiagnosed as intraductal papillary neoplasm of the bile duct