Prog Med Phys.
2018 Mar;29(1):1-7. 10.14316/pmp.2018.29.1.1.
Impact of the Respiratory Motion and Longitudinal Profile on Helical Tomotherapy
- Affiliations
-
- 1Department of Radiation Oncology, Jeju National University Hospital, Jeju University College of Medicine, Jeju, Korea.
- 2Department of Radiation Oncology, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea. KPARK02@yuhs.ac
- KMID: 2411947
- DOI: http://doi.org/10.14316/pmp.2018.29.1.1
Abstract
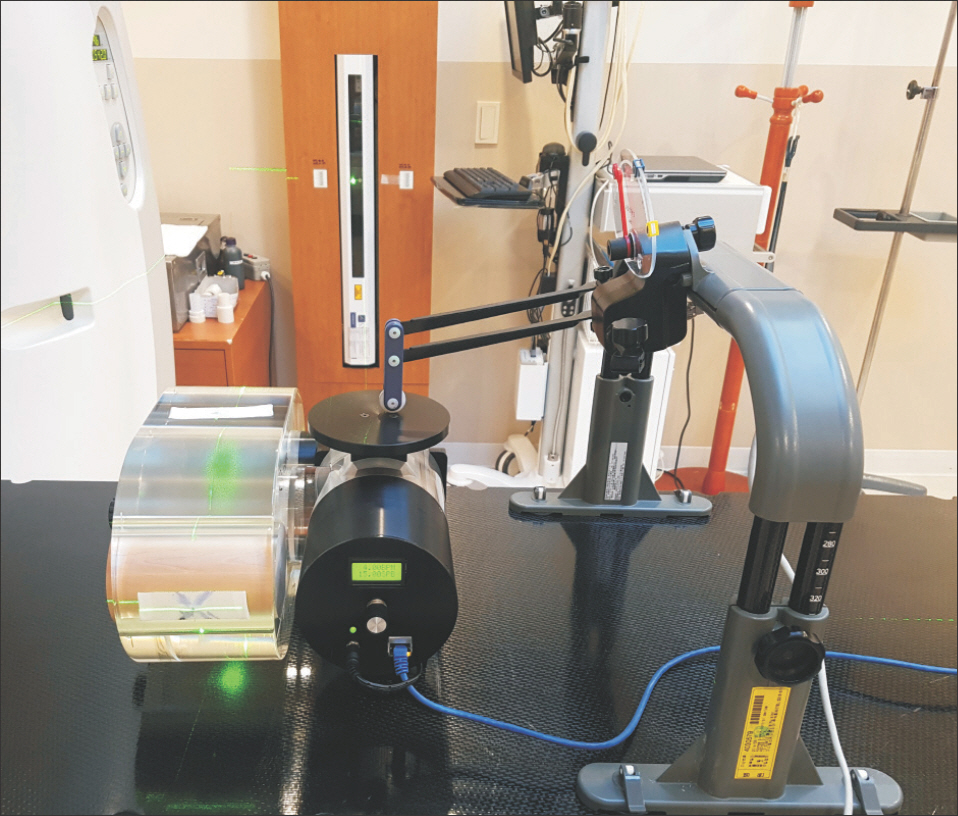
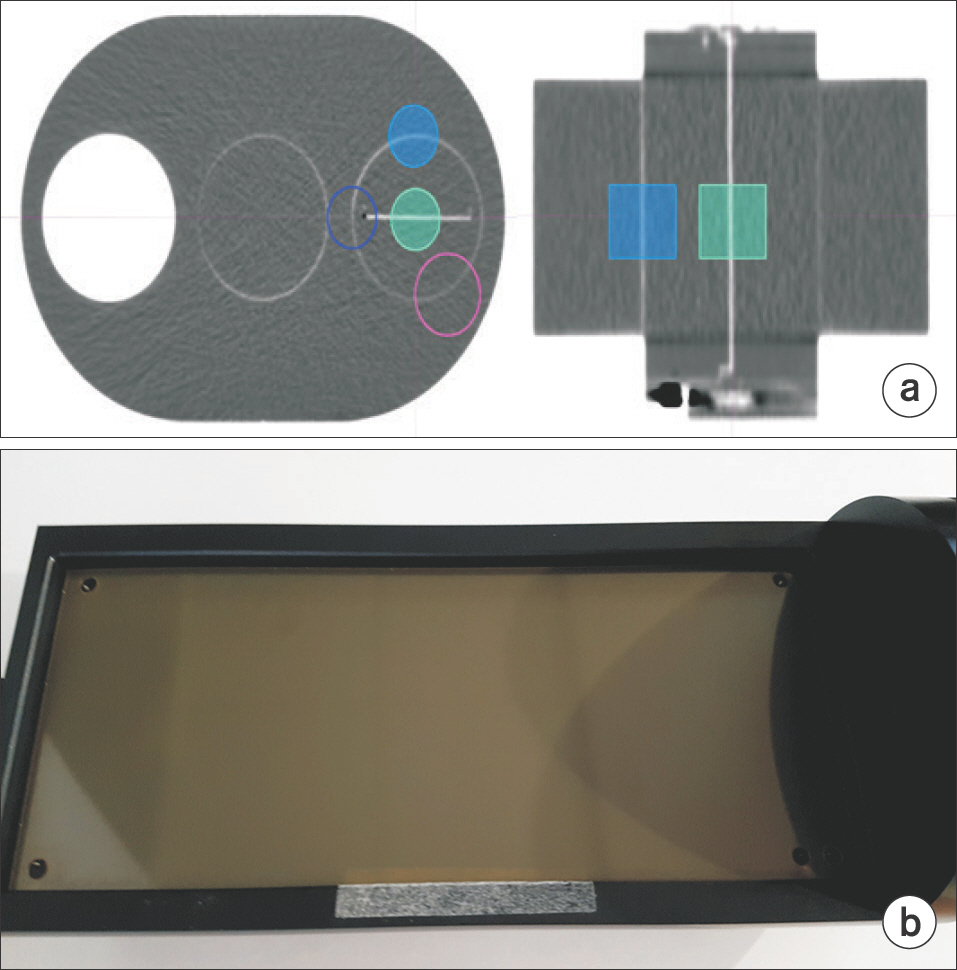
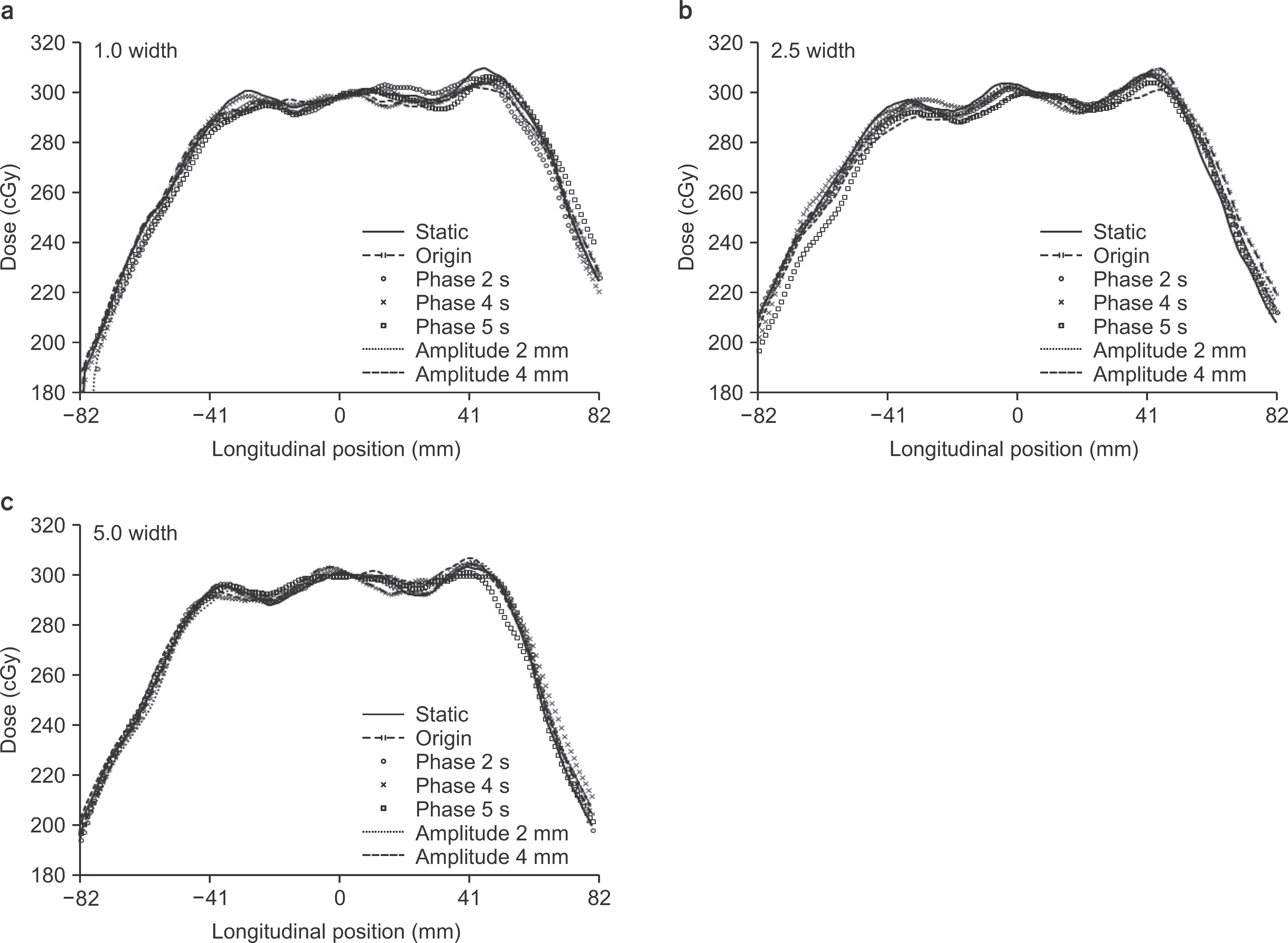
- The TomoTherapy® beam-delivery method creates helical beam-junctioning patterns in the dose distribution within the target. In addition, the dose discrepancy results in the particular region where the resonance by pattern of dose delivery occurs owing to the change in the position and shape of internal organs with a patient's respiration during long treatment times. In this study, we evaluated the dose pattern of the longitudinal profile with the change in respiration. The superior-inferior motion signal of the programmable respiratory motion phantom was obtained using AbChes as a four-dimensional computed tomography (4DCT) original moving signal. We delineated virtual targets in the phantom and planned to deliver the prescription dose of 300 cGy using field widths of 1.0 cm, 2.5 cm, and 5.0 cm. An original moving signal was fitted to reflecting the beam delivery time of the TomoTherapy®. The EBT3 film was inserted into the phantom movement cassette, and static, without the movement and with the original movement, was measured with signal changes of 2.0 s, 4.0 s, and 5.0 s periods, and 2.0 mm and 4.0 mm amplitudes. It was found that a dose fluctuation within ±4.0% occurred in all longitudinal profiles. Compared with the original movement, the region of the gamma index above 1 partially appeared within the target and the border of the target when the period and amplitude were changed. Gamma passing rates were 95.00% or more. However, cases for a 5.0 s period and 4.0 mm amplitude at a field width of 2.5 cm and for 2.0 s and 5.0 s periods at a field width of 5.0 cm have gamma passing rates of 92.73%, 90.31%, 90.31%, and 93.60%. TomoTherapy® shows a small difference in dose distribution according to the changes of period and amplitude of respiration. Therefore, to treat a variable respiratory motion region, a margin reflecting the degree of change of respiration signal is required.
Keyword
MeSH Terms
Figure
Reference
-
References
1. T.Rock M, Timothy H, Stuart S, Paul R, Joseph OD, James Y, Bhudatt P, Timothy K. Tomotherapy: A new concept for the delivery of dynamic conformal radiotherapy. Med. Phys. 1993; 20:1709–1719.
Article2. Robert T, Krisha O, Brian DJ, Lacy ET, Daniel GM, Michael SA, Elizabeth GM, David TM. Comparison of radiation treatment delivery for pancreatic cancer: Linac intensitymodulated radiotherapy versus helical tomotherapy. Radiation Oncology. 2012; 56:332–337.3. Mathieu S, Simon JT, G . Samuel JT, Jean B, Francois B, Raphael M. Implementation of TomoEDGE in the independent dose calculator CheckTomo. J Appl Clin Med Phys. 2017; 18:92–99.4. Michael WK, Sarah AB, Robert J, T.Rockwell M. Confirmation, refinement, and extension of a study in intrafraction motion interplay with sliding jaw motion. Med. Phys. 2005; 32:2346–2350.
Article5. Cedric XY, David AJ, John WW. The effects of intrafraction organ motion on the delivery of dynamic intensity modulation. Phys.Med.Biol. 1998; 43:91–104.6. Bryan K, Jeff Ch, Tomas K, Jerry B. Motion-induced dose artifacts in helical tomotherapy. Phys.Med.Biol. 2009; 54:5707–5734.7. Brain K, Paul WR, Janelle AM, James ML, Ke Sh. A motion phantom study on helical tomotherapy: the dosimetric impacts of delivery technique and motion. Phys. Med. Biol. 2007; 52:243–255.8. Michael WK, Fenwick J, James JA, Jeraj R, Kapatoes JM, Keller H, Mackie TR, Olivera G, Soisson ET. The helical tomotherapy thread effect. Med. Phys. 2005; 32:1414–1423.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study of Motion-induced Dose Error Caused by Irregular Tumor Motion in Helical Tomotherapy
- Dosimetric Analysis on the Effect of Target Motion in the Delivery of Conventional IMRT, RapidArc and Tomotherapy
- Helical Tomotherapy: Image-guided Intensity Modulated Radiation Therapy
- Comparison of survival rates between patients treated with conventional radiotherapy and helical tomotherapy for head and neck cancer
- Superficial Dosimetry for Helical Tomotherapy