J Korean Soc Echocardiogr.
1994 Dec;2(2):143-154. 10.4250/jkse.1994.2.2.143.
Changes in Video Density of the Left Ventricle by Transpulmonary Administration of Sonicated Albumin: Contrast Echocardiographic Study
- Affiliations
-
- 1Department of Medicine, Chosun University Medical College, Kwangju, Korea.
- 2Department of Rehabilitation and Physical Medicine, Kagoshima University, Kagoshima, Japan.
- KMID: 2410442
- DOI: http://doi.org/10.4250/jkse.1994.2.2.143
Abstract
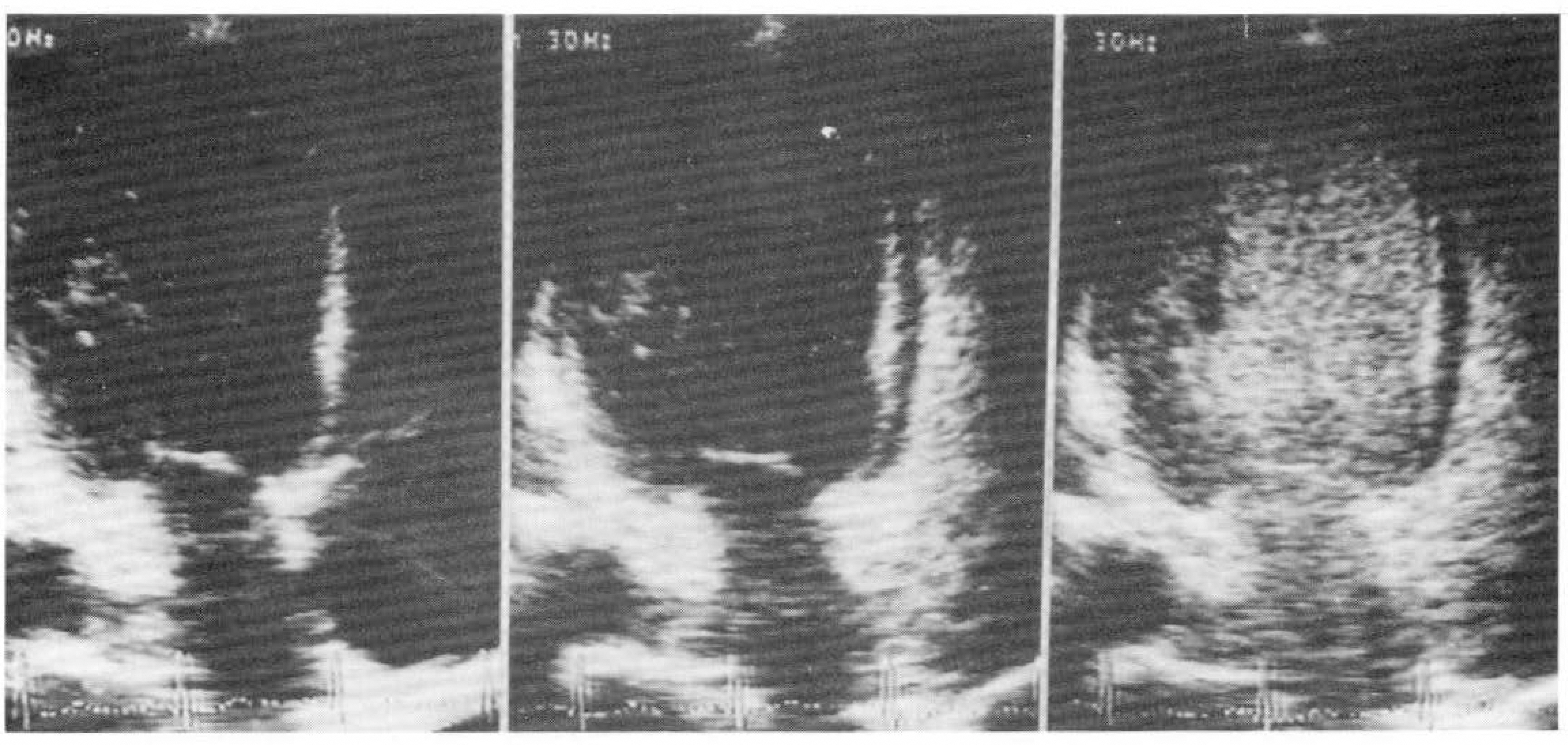
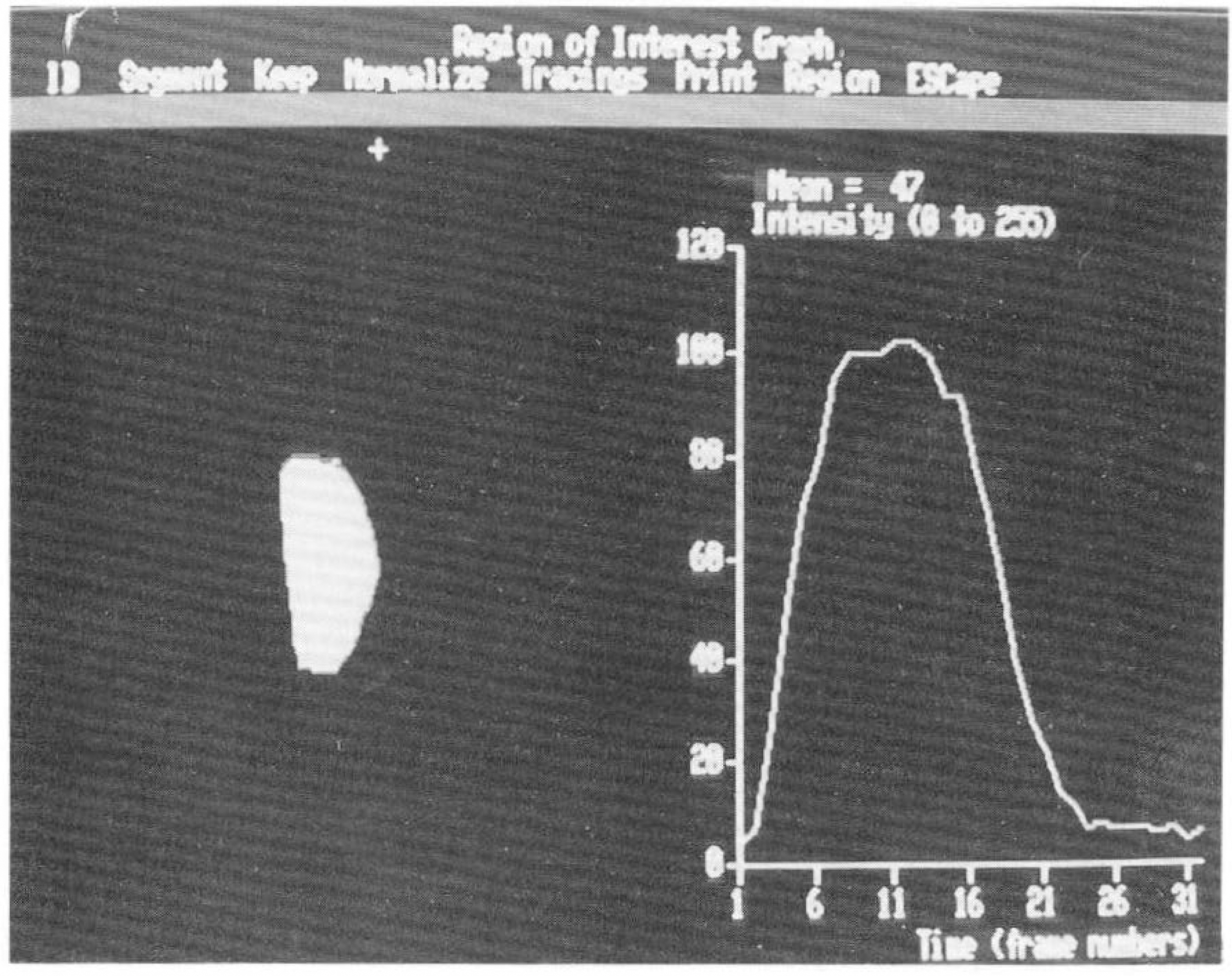
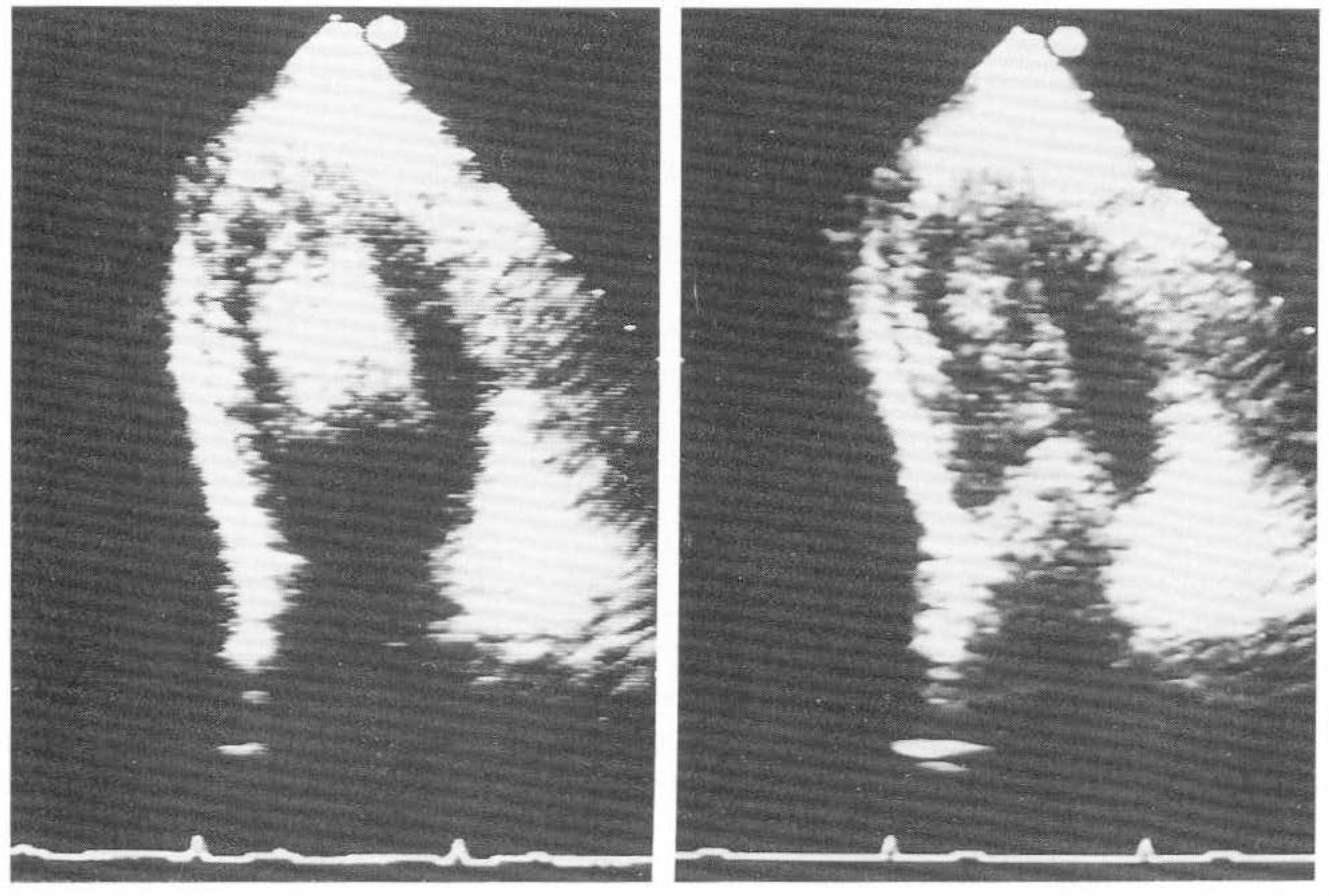
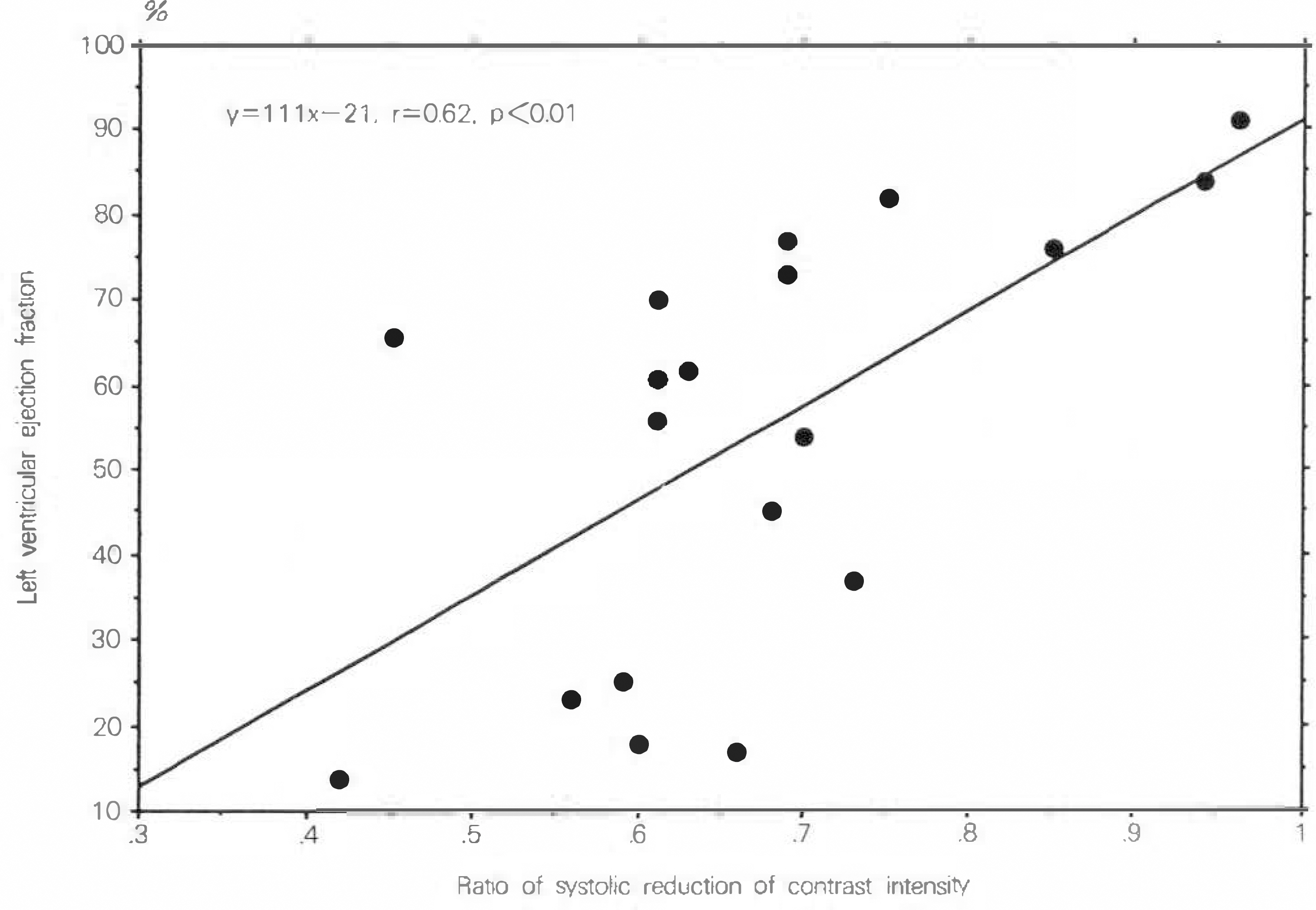
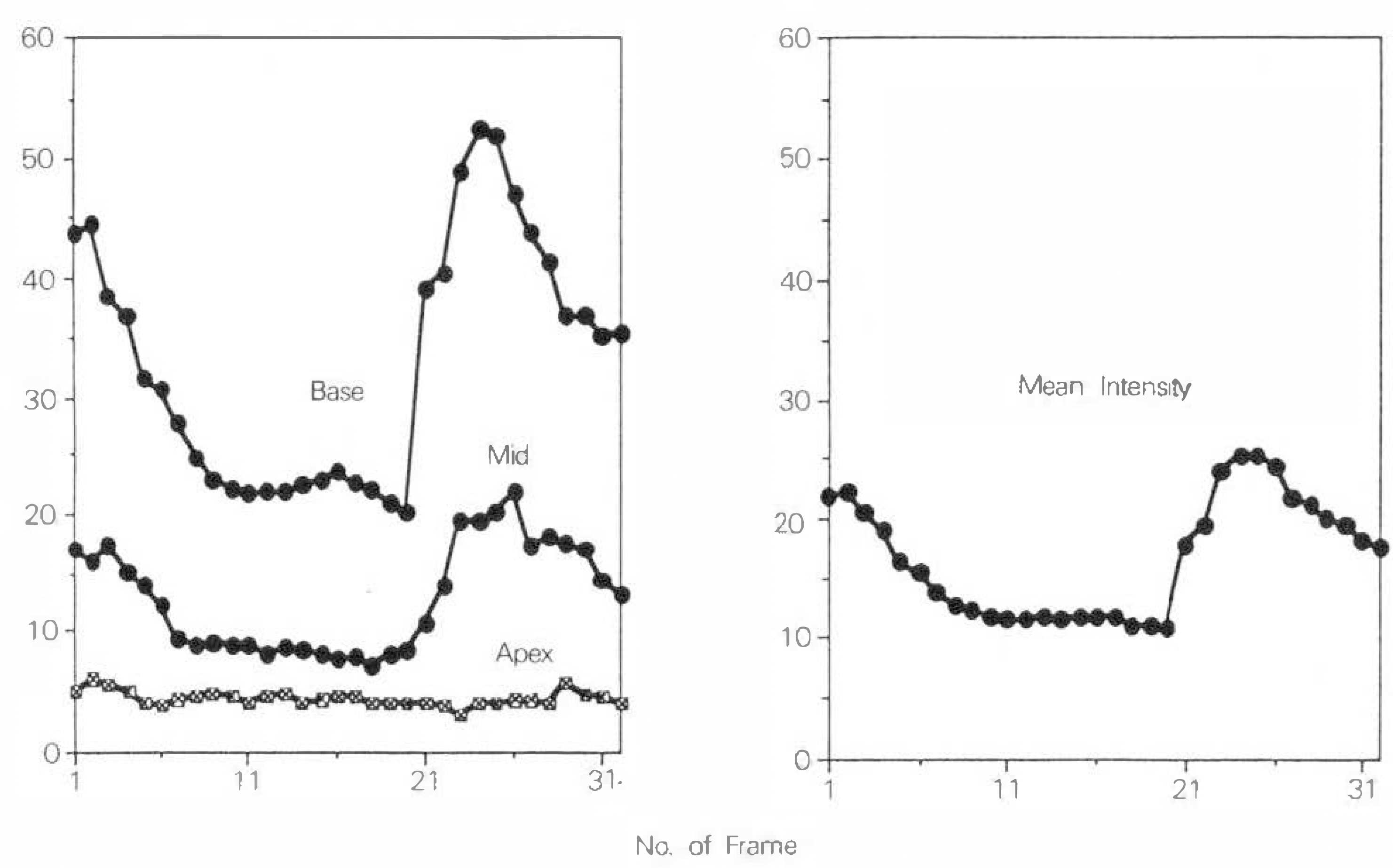
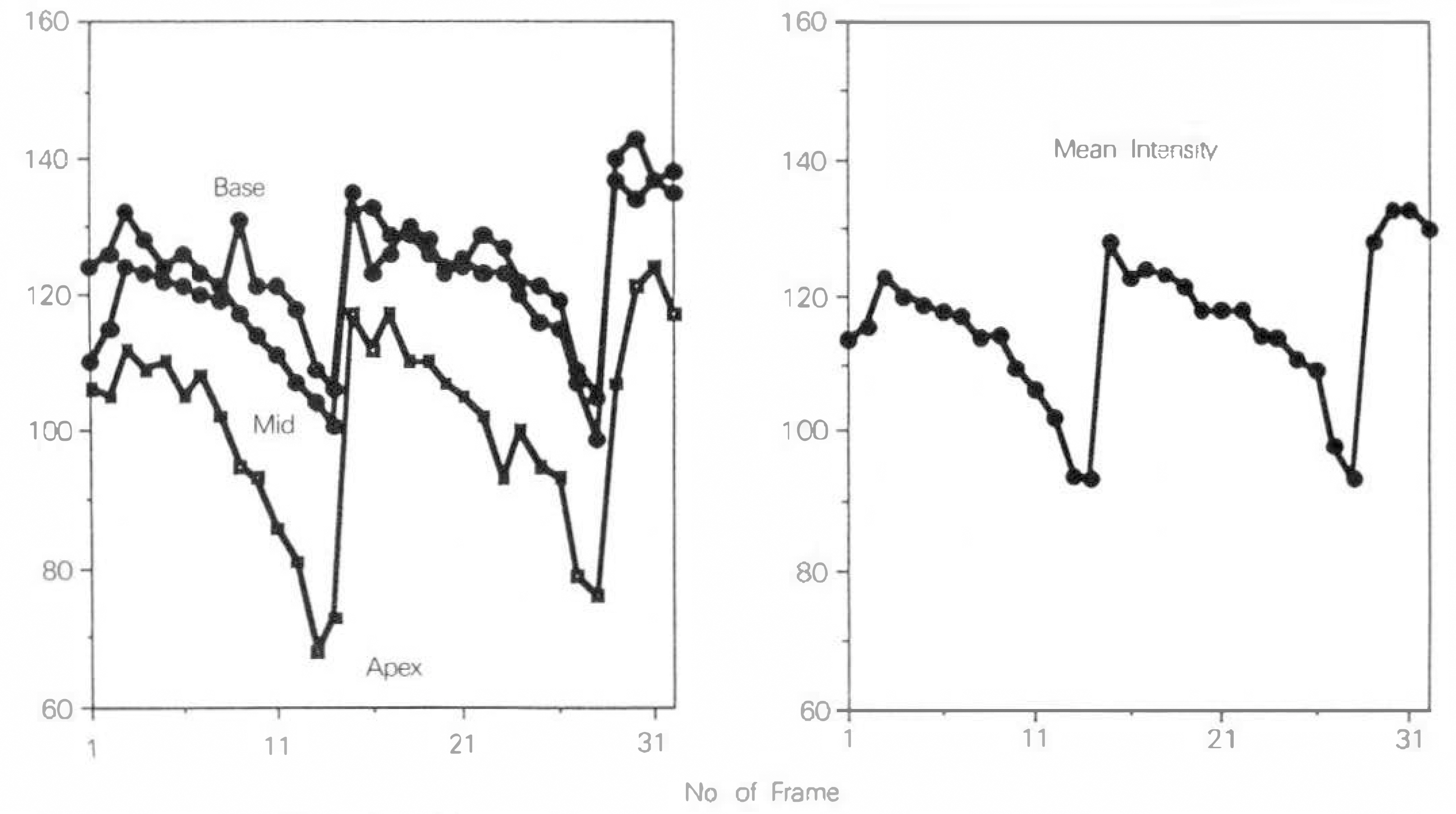
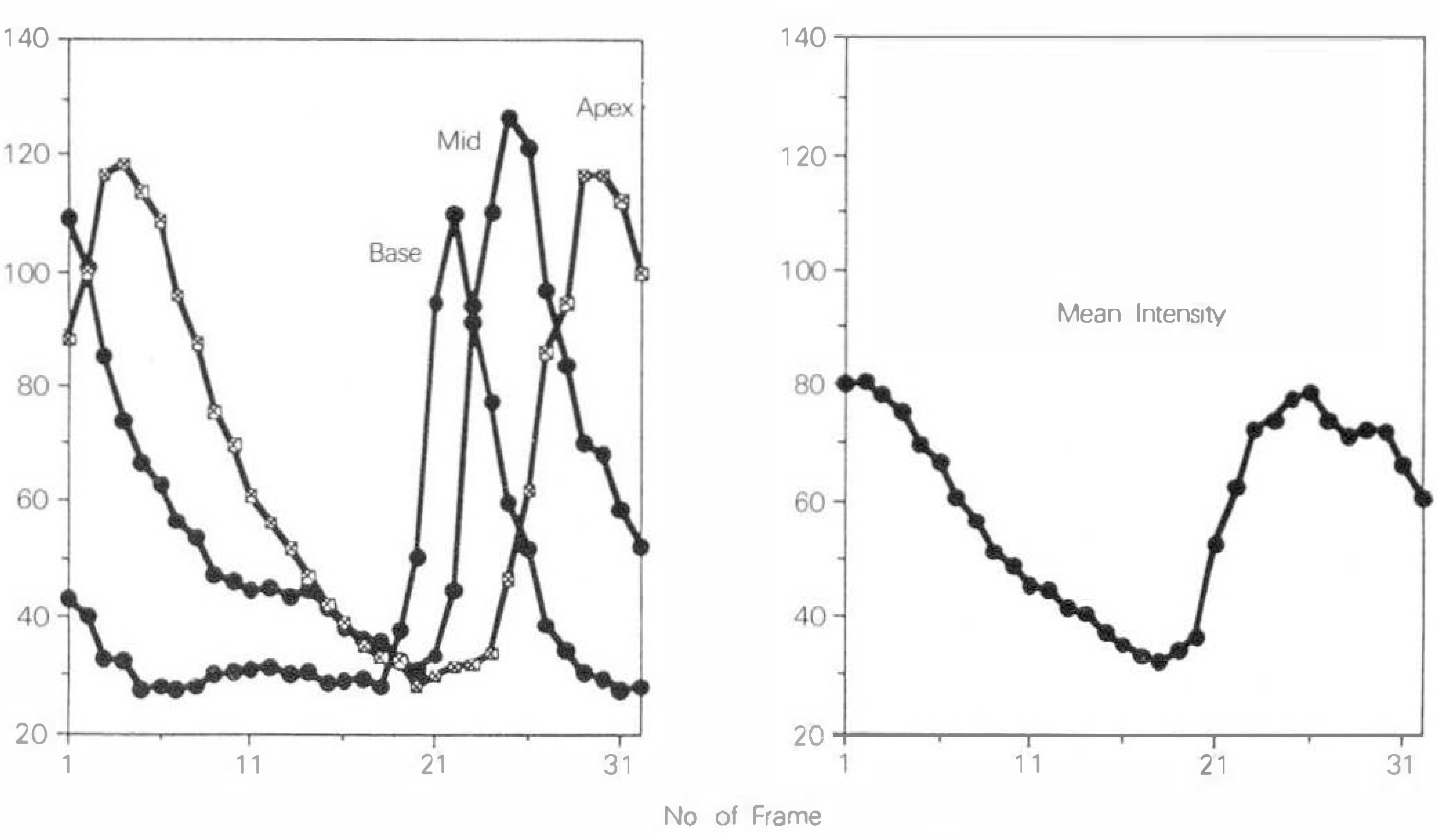
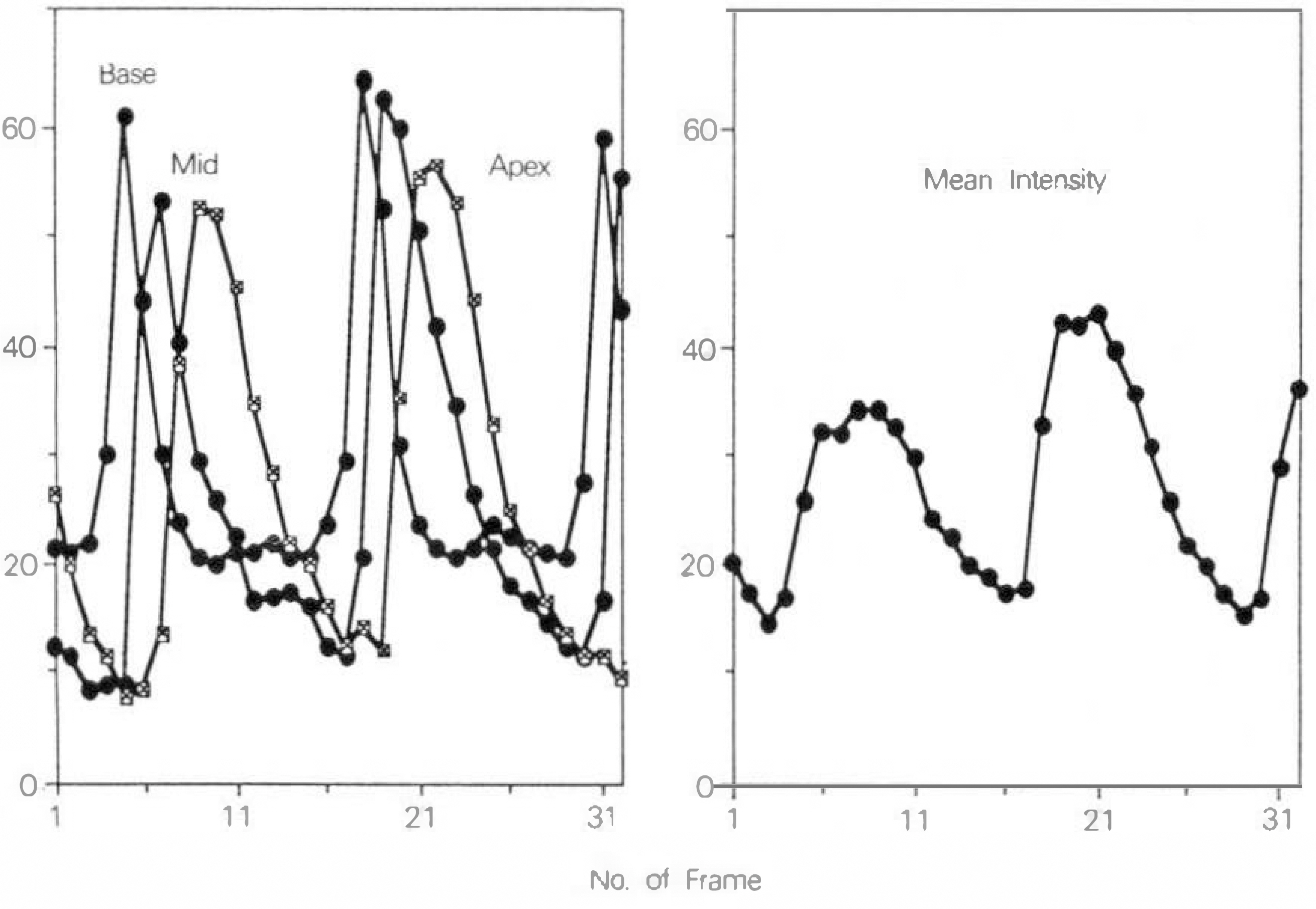
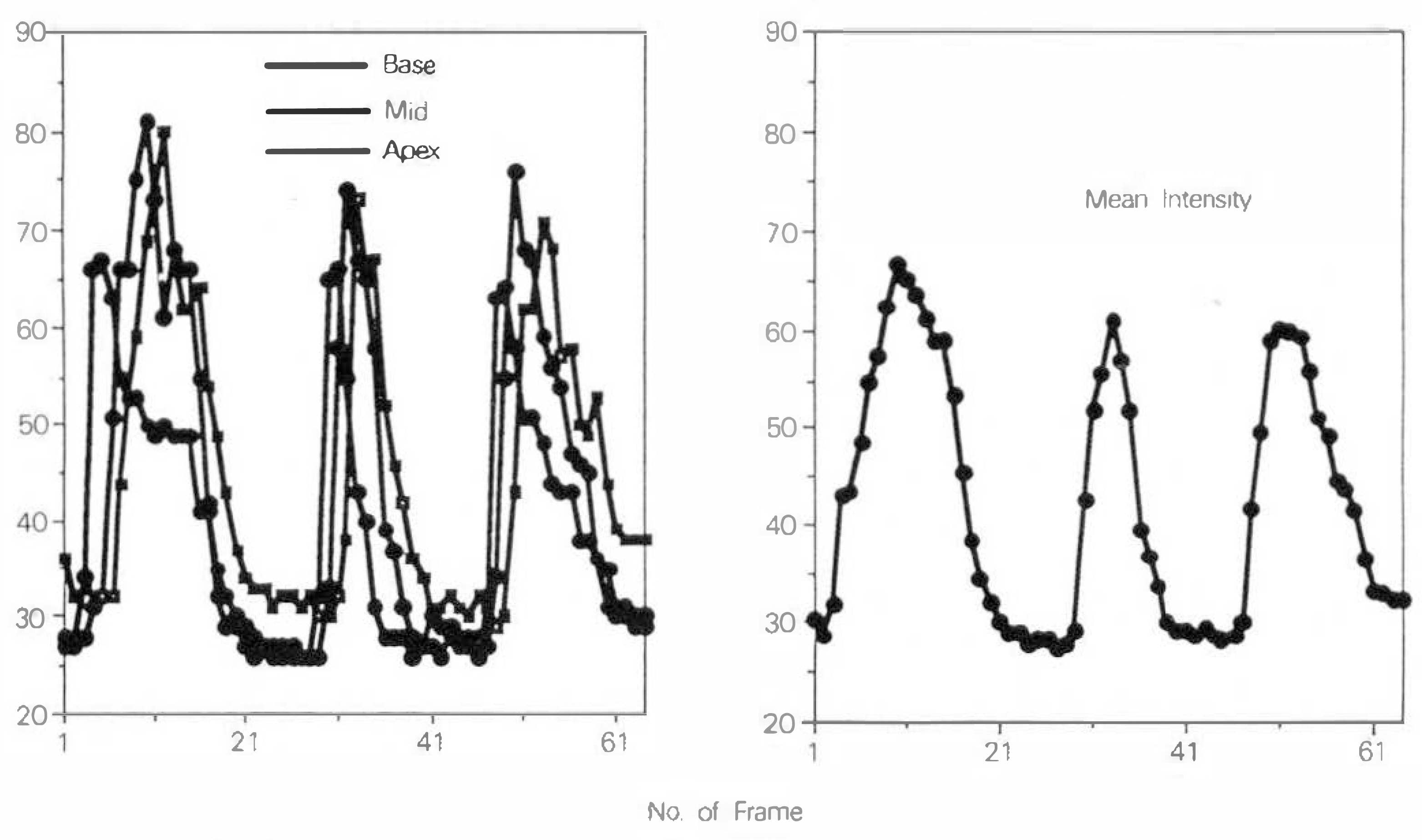
- With the advance of color-Doppler echocardiography, there has been many studies on the hemodynamics of the left ventricle. Doppler echocardiography, however, has many limitations, and the recently developed contrast echocardiography has overcome those limitations. The purpose of this study is to analyze of the blood flow hemodynamics of the left ventricle by transpulmonary contrast echocardiography. Subjects were fifteen healthy volunteers(group I), fifteen patients of various heart diseases(group 2), and thirteen patients with dilated cardiomyopathy(group 3). We used sonicated albumin, and a videodensitometer for the analysis of the base, midventricle and apex of the left ventricle. Among the total 43 subjects, left ventricular opacifications were obtained in 28 subjects(65.1%). Tehre were systolic decreases in group 1(68.5±1.7%), and group 2(67.0±1.4%), and the systolic decrease correlated with the mean blood pressure(r=0.46, p < 0.05), and ejection fraction(r=0.62, p < 0.01) of the subject, while it showed no correlation with the systolic blood pressure. There were three definitive diastolic filling patterns, type A : early diastolic peak and late diastolic peak, thpe B : only early diastolic peak with a slow decrease, type C : three different peak times of base, midventricle and apex of left ventricle. The difference between the peak times of the base and midventricle and between the midventricle and apex of the left ventricle of group 3(dilated cardiomyopathy) were 4.1±1.4, 4.7±1.8, different from those of group 1 and 2 significantly(p < 0.001, respectively) According to the above results, contrast echocardiography with sonicated albumin is useful for the analysis of blood flow patterns of the left ventricle.
MeSH Terms
Figure
Reference
-
References
1). Miyatake K, Omoto M, Kinoshita N, Izumi S, Owa M, Takao S, Sakakibara H, Nimura Y. Clinical application of a new type of real-time two-dimensional Doppler flow imaging system. Am J Cardiol. 54:857–868. 1984.2). Jacobs LE, Kotler MN, Parry WR. Flow patterns in dilated cardiomyopathy: a pulsed-wave and color flow Doppler study. J Am Soc Echocardiogr. 3:294–302. 1990.3). Garrahy PJ, Kwan OL, Booth DC, DeMaria AN. Assessment of abnormal systolic intraventricular flow patterns by Doppler imaging in patients with left ventricular dyssynergy. Circulation. 82:95–104. 1990.
Article4). Beppu S, Izumi S, Miyatake K, Nagata S, Park YD, Sakakibara H, Nimura Y. Abnormal blood pathways in left ventricular cavity in acute myocardial infarction: experimental observations with special reference tio regional wall motion abnormality and hemostasis. Circulation. 78:157–164. 1988.5). Feinstein SB, Ten Cate FJ, Zwehl W, Ong K, Maurer G, Tei C, Shah PM, Meerbaum S, Corday E. Two-dimensional contrast echocardiography: I in vitro development and quantitative analysis of echo contrast agents. J Am Coll Cardiol. 3:14–20. 1984.
Article6). Keller MW, Feinstein SB, Watson DD. Successful left ventricular opacification following a peripheral injection of a sonicated contrast agent: an experimental evaluation. Am Heart J. 114:570–575. 1987.7). Keller MW, Glasheen WP, Teja K, Gear A, Kaul S. Myocardial contrast echocardiography without significant effects or reactive hyperemia: a major advantage in the imaging of regional myocardial perfusion. J Am Coll Cardiol. 12:1039–1047. 1988.8). Feinstein SB, Cheirif J, Ten Cate FJ, Silverman PR, Heidenreich PA, Dick C, Desir RM, Armstrong WF, Quinones MA, Shah PM. Safety and efficacy of a new transpulmonary ultrasound contrast agent: initial multicenter clinical results. J Am Coll Cardiol. 16:316–324. 1990.
Article9). Smith MD, Kwan OL, Reiser HJ, DeMaria AN, Evans J, Fritzsch TH. Superior intensity and reproducibility of SHU-454, a new right heart contrast agent. J Am Coll Cardiol. 3:992–998. 1984.
Article10). Smith MD, Elion JL, McClure RR, Kwan OL, DeMaria AN, Evans J, Fritzsch TH. Left heart opacification with peripheral venous injection of a new saccharide echo contrast agent in dogs. J Am Coll Cardiol. 13:1622–1628. 1989.
Article11). Shapiro JR, Reisner SA, Lichtenberg GS, Meltzer RS. Intravanous contrast echocardiography with use of sonicated albumin in humans: systolic disappearance of left ventricular contrast after transpulmonary transmission. J Am Coll Cardiol. 6:1607–1617. 1990.12). Voci P, Bilotta F, Scibilia G, Mercanti C, Caretta Q, Marino B, Reale A. In vitro development and clinical applications of sonicated echo contrast agents. Am J Cardiac lmag. 5:192–199. 1991.13). Gramiak R, Shah PM, Kramer DH. Ultrasound cardiography. Contrast studies in antomy and function. Radiology. 92:939. 1968.14). Tei C, Shah PM, Ormiston JA. The assessment of tricuspid regurgitation by directional analysis of right atrial systolic linear reflux echoes with contrast M-mode echocardiograms. Am Heart J. 103:1025–1030. 1982.15). Crouse LJ. Sonicated serum albumin in contrast echocardiography: improved segmental wall motion detection and implications for stress echocardiography. Am J Cardiol. 69:42H–45H. 1992.16). Falcone RA, Marcovitz PA, Rasmussen C, Dittrich HC, Armstrong WF. Albunex increases identification of left ventricular endocardial borders during dobutamine stress echocardiography. J Am Soc Echocardiogr. 7:S29. 1994.17). Tei C, Sakamaki T, Shah PM, Meerbaum S, Shimoura K, Kondo S, Corday E. Myocardial contrast echocardiography: a reproducible technique of myocardial opacification for identifying regional perfusion deficts. Circulation. 67:585–593. 1983.18). Kabas JS, Kisslo J, Flick CL, Johnson SH, Craig DM, Stanley TE, Smith PK. Intraoperative perfusion contrast echocardiography. Initial experience during coronary artery bypass grafting. J Thorac Cardiovasc Surg. 99:536–542. 1990.19). Voci P, Bilotta F, Merialdo P, Eng C, Agati L. Myocardial contrast enhancement after intravenous injection of sonicated albumin microbubbles: a trasesophageal echocardiography dipyridamol study. J Am Soc Echocardiogr. 7:337–46. 1994.20). Vandenberg BF. Myocardial perfusion and contrast echocardiography: review and new perspectives. Echocardiography. 8:65–75. 1991.
Article21). Lim YJ, Nanto S, Masuyama T, Kodama K, Kohama A, Kitabatake A, Kamada T. Coronary collaterals assessed with myocardial contrast echocardiography in healed myocardial infarction. Am J Cardiol. 66:556–561. 1990.
Article22). Heger JJ, Weyman AE, Qann LS, Togers EW, Dillon JC, Ferigenbaum H. Cross-sectional echocardiographic analysis of the extent of left ventricular asynergy in acute myocardial infaction. Circulation. 61:1113–1118. 1980.23). Demaria AN, Bommer W, Kwan OL, Riggs K, Smith M, Waters J. In vivo correlation fo thermodilution cardiac output and videodensitometric indicator-dilution curves obtained from contrast two-dimensional echocardiograms. J Am Coll Cardiol. 3:999–1004. 1984.24). Meerbaum S. Principles of echo contrast. Nanda N, Schlief R, editors. Advances in echo imaging using contrast enhancement. Kluwer Academic Publishers;The Nethelands: 1993. p. 9–42.
Article25). Vuille C, Nidorf M, Morrissey RL, Newell JB, Weyman AE, Picard MH. Effect of static pressure on the disappearance rate of specific echocardiographic contrast agents. J Am Soc Echocardiogr. 7:347–354. 1994.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left Ventricular Opacification and Hemodynamic Effect of Intravenous Injection of Fluorocarbon Based Echocardiographic Contrast Agent
- Development of Microbubble Contrast Agents for High Frequency Ultrasound Microscopy
- Myocardial Contrast Echocardiography for the Assessment of Coronary Blood Flow Reserve
- Common Atrioventricular Canal Diagnosed by Contrast Echocardiography Report of Two Cases
- Two-dimensional Echocardiographic Assessment of Myocardial Strain: Important Echocardiographic Parameter Readily Useful in Clinical Field