Investig Clin Urol.
2017 Jul;58(4):281-288. 10.4111/icu.2017.58.4.281.
Prevalence and management status of urologic disease in geriatric hospitals in South Korea: A population-based analysis
- Affiliations
-
- 1Department of Urology, Seoul National University College of Medicine, Seoul, Korea. drboss@gmail.com
- 2Department of Urology, Gachon University Gil Medical Center, Incheon, Korea.
- 3Department of Urology, Dongguk University Ilsan Medical Center, Goyang, Korea.
- 4Community Nursing Science, Seoul National University College of Nursing, Seoul, Korea.
- KMID: 2410296
- DOI: http://doi.org/10.4111/icu.2017.58.4.281
Abstract
- PURPOSE
This study aimed to investigate the prevalence and management status of urologic disease in geriatric hospitals in Korea.
MATERIALS AND METHODS
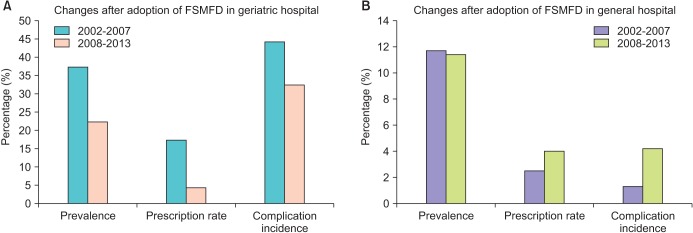
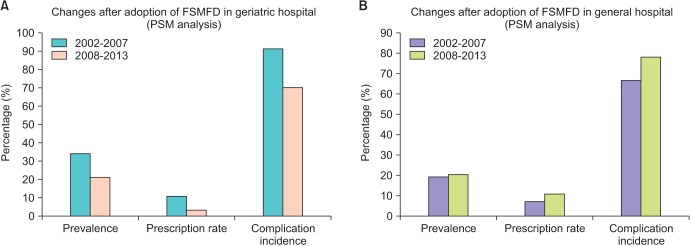
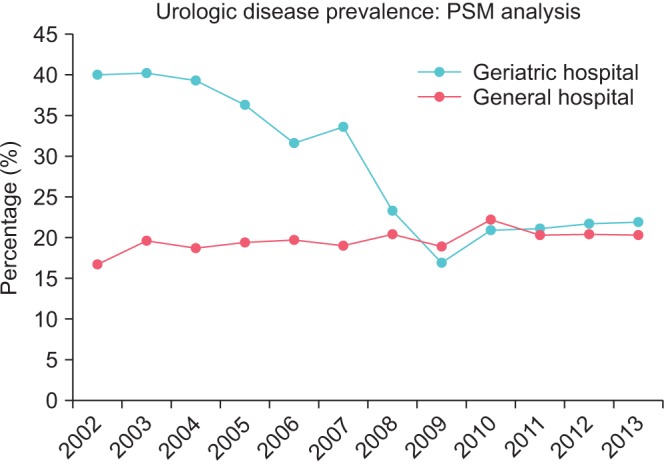
We conducted population-based analyzed using cohort established by the National Health Insurance Service of Korea, which contains the medical insurance data of 1 million people from 2002 to 2013. The prevalence, prescription rate, and complication incidence of urologic disease in geriatric hospitals were compared with similar-sized general hospitals. We analyzed the changes that followed the adoption of the fixed sum medical fee per day for geriatric hospitals, which began in January 2008. Subgroup analysis was conducted in an elderly group and a propensity score matching (PSM) group.
RESULTS
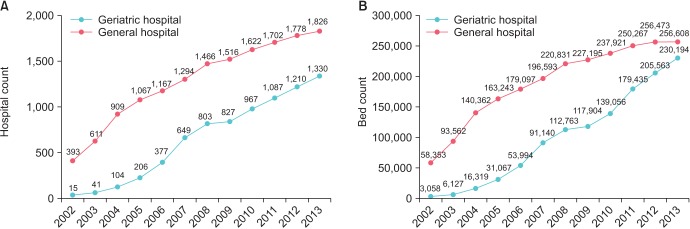
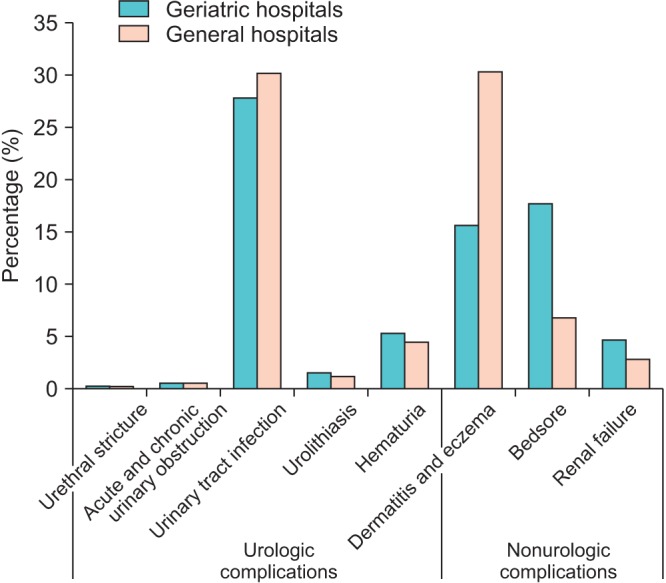
During this time, the number of geriatric hospitals exponentially increased over general hospitals (675.5%/y vs. 30.9%/y). The prevalence, prescription rate, and complication incidence of urologic disease was higher in geriatric hospitals than in general hospitals (2.1, 1.8, and 1.4 times higher). In the elderly group, the prevalence of urologic disorders was higher in geriatric hospitals than in general hospitals, but the prescription rate was lower (26.5% vs. 19.9% and 6.8% vs. 10.0%). This tendency also founded in the PSM analysis. After the medical fee system changed, diagnosis and prescription rates decreased in geriatric hospitals but increased in general hospitals.
CONCLUSIONS
Urologic diseases are more prevalent yet management has some problem in geriatric hospitals. Lack of institutional urologists and changes in the medical payment system should be associated with this problem. Additional study and political support are needed to overcome this issue.
Keyword
MeSH Terms
Figure
Reference
-
1. United Nations. World population aging 2015 [Internet]. New York: United Nations, Department of Economic and Social Affairs Population Division;2015. cited 2016 May 5. Available from: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf.2. Statistics Korea. Population projections for Korea: 2010-2016 (Based on the 2010 Census) [Internet]. Daejeon: Statistics Korea;c2017. cited 2015 Oct 12. Available from: http://kosis.kr/ups3/service/ch_file_down.jsp?PUBCODE=PJ&FILE_NAME=/ups3/upload/101/PJ/PJ2011.pdf&SEQ=15.3. Korea Institute for Health and Social Affairs. 2014 Elderly reports [Internet]. Sejong: Korea Institute for Health and Social Affairs;c2017. cited 2017 May 1. Available from: http://repository.kihasa.re.kr:8080/handle/201002/13710.4. Bo M, Fonte G, Pivaro F, Bonetto M, Comi C, Giorgis V, et al. Prevalence of and factors associated with prolonged length of stay in older hospitalized medical patients. Geriatr Gerontol Int. 2016; 16:314–321. PMID: 25752922.
Article5. Batista-Miranda JE, Molinuevo B, Pardo Y. Impact of lower urinary tract symptoms on quality of life using Functional Assessment Cancer Therapy scale. Urology. 2007; 69:285–288. PMID: 17320665.
Article6. Lawhorne LW, Ouslander JG, Parmelee PA, Resnick B, Calabrese B. Urinary incontinence: a neglected geriatric syndrome in nursing facilities. J Am Med Dir Assoc. 2008; 9:29–35. PMID: 18187110.
Article7. Robertson C, Link CL, Onel E, Mazzetta C, Keech M, Hobbs R, et al. The impact of lower urinary tract symptoms and comorbidities on quality of life: the BACH and UREPIK studies. BJU Int. 2007; 99:347–354. PMID: 17313423.
Article8. Korea Statistical Information Service. Number of specialists [Internet]. Daejeon: Statistics Korea;c2017. cited 2016 May 5. Available from: http://kosis.kr/statHtml/statHtml.do?orgId=354&tblId=DT_HIRA4K&vw_cd=&list_id=&scrId=&seqNo=&lang_mode=ko&obj_var_id=&itm_id=&conn_path=K1&path=#.9. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15. PMID: 26822938.
Article10. Jewett MA, Fernie GR, Holliday PJ, Pim ME. Urinary dysfunction in a geriatric long-term care population: prevalence and patterns. J Am Geriatr Soc. 1981; 29:211–214. PMID: 6785337.
Article11. Lee YS, Lee KS, Jung JH, Han DH, Oh SJ, Seo JT, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011; 29:185–190. PMID: 19898824.
Article12. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984; 132:474–479. PMID: 6206240.
Article13. Garraway WM, Collins GN, Lee RJ. High prevalence of benign prostatic hypertrophy in the community. Lancet. 1991; 338:469–471. PMID: 1714529.
Article14. Chung JS, Byun SS, Han BK, Jeong SJ, Hong SK, Lee SE. Changes in prostate-specific antigen levels and prostate volume in octogenarian men: community-based study. Urology. 2009; 73:1270–1273. PMID: 19371943.
Article15. Lee YJ, Jeong SJ, Byun SS, Lee JJ, Han JW, Kim KW. Prevalence and correlates of nocturia in community-dwelling older men: results from the korean longitudinal study on health and aging. Korean J Urol. 2012; 53:263–267. PMID: 22536470.
Article16. Lee E, Yoo KY, Kim Y, Shin Y, Lee C. Prevalence of lower urinary tract symptoms in Korean men in a community-based study. Eur Urol. 1998; 33:17–21. PMID: 9471036.
Article17. Offermans MP, Du Moulin MF, Hamers JP, Dassen T, Halfens RJ. Prevalence of urinary incontinence and associated risk factors in nursing home residents: a systematic review. Neurourol Urodyn. 2009; 28:288–294. PMID: 19191259.
Article18. Shin CW, Kim SD, Cho WY. The prevalence and management of urinary incontinence in elderly patients at sanatorium in Busan area. Korean J Urol. 2009; 50:450–456.
Article19. Lee SH, Kang JS, Kim JW, Lee SJ. Incontinence pad usage in medical welfare facilities in Korea. Int Neurourol J. 2013; 17:186–190. PMID: 24466466.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corrigendum: Correction of the Acknowledgments. Prevalence and management status of urologic disease in geriatric hospitals in South Korea: A population-based analysis
- Urology and Geriatrics in Korea: Present Status and Future Directions
- Prevalence and management status of urologic diseases in geriatric hospitals in South Korea: A field research
- Management of urinary incontinence in geriatric hospitals
- Factors Influencing Nurses' Implementation of Evidence-based Fall Management in Geriatric Hospitals