J Korean Orthop Assoc.
2018 Apr;53(2):159-165. 10.4055/jkoa.2018.53.2.159.
The Results of Hemicortical Resection for Malignant Bone Tumor
- Affiliations
-
- 1Department of Orthopedic Surgery, Korea Cancer Center Hospital, Seoul, Korea. wssongmd@gmail.com
- KMID: 2410064
- DOI: http://doi.org/10.4055/jkoa.2018.53.2.159
Abstract
- PURPOSE
Hemicortical resection may be applied to bone tumors arising at the bone surface or of eccentric location due to minimal medullary involvement. The purpose of this study was to evaluate the results of hemicortical resection for malignant bone tumors.
MATERIALS AND METHODS
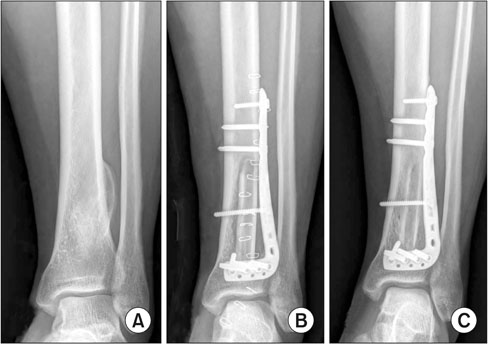
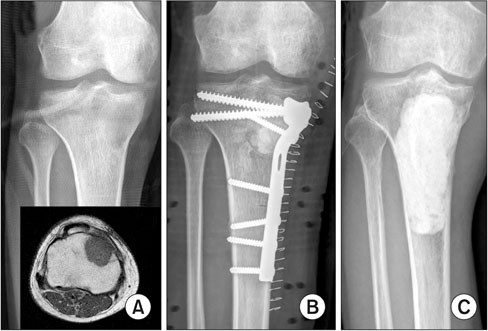
We retrospectively reviewed 18 patients who were treated with hemicortical resection between 2005 and 2014. The study included 10 patients with parosteal osteosarcoma, 5 patients with osteosarcoma, 2 patients with periosteal chondrosarcoma, and 1 patient with chondrosarcoma, who were followed-up for a mean duration of 61 months (24-125 months). We evaluated 1) the oncologic outcome (recurrence, metastasis), 2) the rate of bony union, and 3) complications, such as fracture or infection, after hemicortical resection and reconstruction.
RESULTS
There were local recurrences in 3 parosteal osteosarcoma patients (16.7%). After subsequent re-excision for recurrence, one patient died of metastasis. The defect after hemicortical resection was reconstructed by bone graft in 15 patients and the grafts were removed for infection in 2 patients. Bone grafts were united in 12 (92.3%) out of 13 patients at 8 months (5-13 months) after reconstruction on average. Host bone fractures occurred in 2 patients (11.1%); infection developed in 3 patients (16.7%), who received hemicondylar resection for osteosarcoma in proximal tibia.
CONCLUSION
Hemicortical resection for eccentric tumors or small tumors showed good clinical results. There is relatively a high risk of infection in the lesion of proximal tibia.
MeSH Terms
Figure
Reference
-
1. Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980; 153:106–120.
Article2. Bielack S, Jürgens H, Jundt G, et al. Osteosarcoma: the COSS experience. Cancer Treat Res. 2009; 152:289–308.
Article3. Campanacci M, Capanna R, Stilli S. Posterior hemiresection of the distal femur in parosteal osteosarcoma. Ital J Orthop Traumatol. 1982; 8:23–28.4. Funovics PT, Bucher F, Toma CD, Kotz RI, Dominkus M. Treatment and outcome of parosteal osteosarcoma: biological versus endoprosthetic reconstruction. J Surg Oncol. 2011; 103:782–789.
Article5. Liu T, Liu ZY, Zhang Q, Zhang XS. Hemicortical resection and reconstruction using pasteurised autograft for parosteal osteosarcoma of the distal femur. Bone Joint J. 2013; 95:1275–1279.
Article6. Bus MP, Dijkstra PD, van de, et al. Intercalary allograft reconstructions following resection of primary bone tumors: a nationwide multicenter study. J Bone Joint Surg Am. 2014; 96:e26.7. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993; 286:241–246.
Article8. Lewis VO, Gebhardt MC, Springfield DS. Parosteal osteosarcoma of the posterior aspect of the distal part of the femur. Oncological and functional results following a new resection technique. J Bone Joint Surg Am. 2000; 82:1083–1088.9. Deijkers RL, Bloem RM, Hogendoorn PC, Verlaan JJ, Kroon HM, Taminiau AH. Hemicortical allograft reconstruction after resection of low-grade malignant bone tumours. J Bone Joint Surg Br. 2002; 84:1009–1014.
Article10. Agarwal M, Puri A, Anchan C, Shah M, Jambhekar N. Hemicortical excision for low-grade selected surface sarcomas of bone. Clin Orthop Relat Res. 2007; 459:161–166.
Article11. Chen WM, Wu PK, Chen CF, Chung LH, Liu CL, Chen TH. High-grade osteosarcoma treated with hemicortical resection and biological reconstruction. J Surg Oncol. 2012; 105:825–829.
Article12. Bus MP, Bramer JA, Schaap GR, et al. Hemicortical resection and inlay allograft reconstruction for primary bone tumors: a retrospective evaluation in the Netherlands and review of the literature. J Bone Joint Surg Am. 2015; 97:738–750.13. Hoffer FA, Nikanorov AY, Reddick WE, et al. Accuracy of MR imaging for detecting epiphyseal extension of osteosarcoma. Pediatr Radiol. 2000; 30:289–298.
Article14. Avedian RS, Haydon RC, Peabody TD. Multiplanar osteotomy with limited wide margins: a tissue preserving surgical technique for high-grade bone sarcomas. Clin Orthop Relat Res. 2010; 468:2754–2764.
Article15. Aponte-Tinao L, Ayerza MA, Muscolo DL, Farfalli GL. Survival, recurrence, and function after epiphyseal preservation and allograft reconstruction in osteosarcoma of the knee. Clin Orthop Relat Res. 2015; 473:1789–1796.
Article16. Li J, Wang Z, Guo Z, Chen GJ, Yang M, Pei GX. Precise resection and biological reconstruction under navigation guidance for young patients with juxta-articular bone sarcoma in lower extremity: preliminary report. J Pediatr Orthop. 2014; 34:101–108.17. Frisoni T, Cevolani L, Giorgini A, Dozza B, Donati DM. Factors affecting outcome of massive intercalary bone allografts in the treatment of tumours of the femur. J Bone Joint Surg Br. 2012; 94:836–841.
Article18. Ortiz-Cruz E, Gebhardt MC, Jennings LC, Springfield DS, Mankin HJ. The results of transplantation of intercalary allografts after resection of tumors. A long-term follow-up study. J Bone Joint Surg Am. 1997; 79:97–106.
Article19. Aponte-Tinao L, Farfalli GL, Ritacco LE, Ayerza MA, Muscolo DL. Intercalary femur allografts are an acceptable alternative after tumor resection. Clin Orthop Relat Res. 2012; 470:728–734.
Article20. Muscolo DL, Ayerza MA, Aponte-Tinao L, Ranalletta M, Abalo E. Intercalary femur and tibia segmental allografts provide an acceptable alternative in reconstructing tumor resections. Clin Orthop Relat Res. 2004; 426:97–102.
Article21. Donati D, Di Liddo M, Zavatta M, et al. Massive bone allograft reconstruction in high-grade osteosarcoma. Clin Orthop Relat Res. 2000; 377:186–194.
Article22. Gerrand CH, Griffin AM, Davis AM, Gross AE, Bell RS, Wunder JS. Large segment allograft survival is improved with intramedullary cement. J Surg Oncol. 2003; 84:198–208.
Article