Perinatology.
2018 Mar;29(1):20-26. 10.14734/PN.2018.29.1.20.
Risk Factors Associated with Hypothermia Immediately after Birth among Preterm Infants
- Affiliations
-
- 1Department of Pediatrics, CHA Bundang Medical Center, CHA University, Seongnam, Korea. joneona@cha.ac.kr
- 2Department of Pediatrics, CHA Gumi Medical Center, CHA University, Gumi, Korea.
- KMID: 2409108
- DOI: http://doi.org/10.14734/PN.2018.29.1.20
Abstract
OBJECTIVE
The purpose of this study was to investigate the distribution of initial body temperature in premature infants admitted to the neonatal intensive care unit and to reveal the perinatal risk factors that may affect the incidence of hypothermia immediately after birth.
METHODS
The subjects were 402 preterm infants born in CHA Bundang Medical Center at less than 32 weeks of gestation between January 2008 and December 2015. They were divided into two groups, the hypothermic group (body temperature < 36℃) and the normothermic group (body temperature 36-37.5℃), and compared to investigate the distribution of body temperature. We also investigated perinatal characteristics associated with hypothermia at admission and 2 hours after admission.
RESULTS
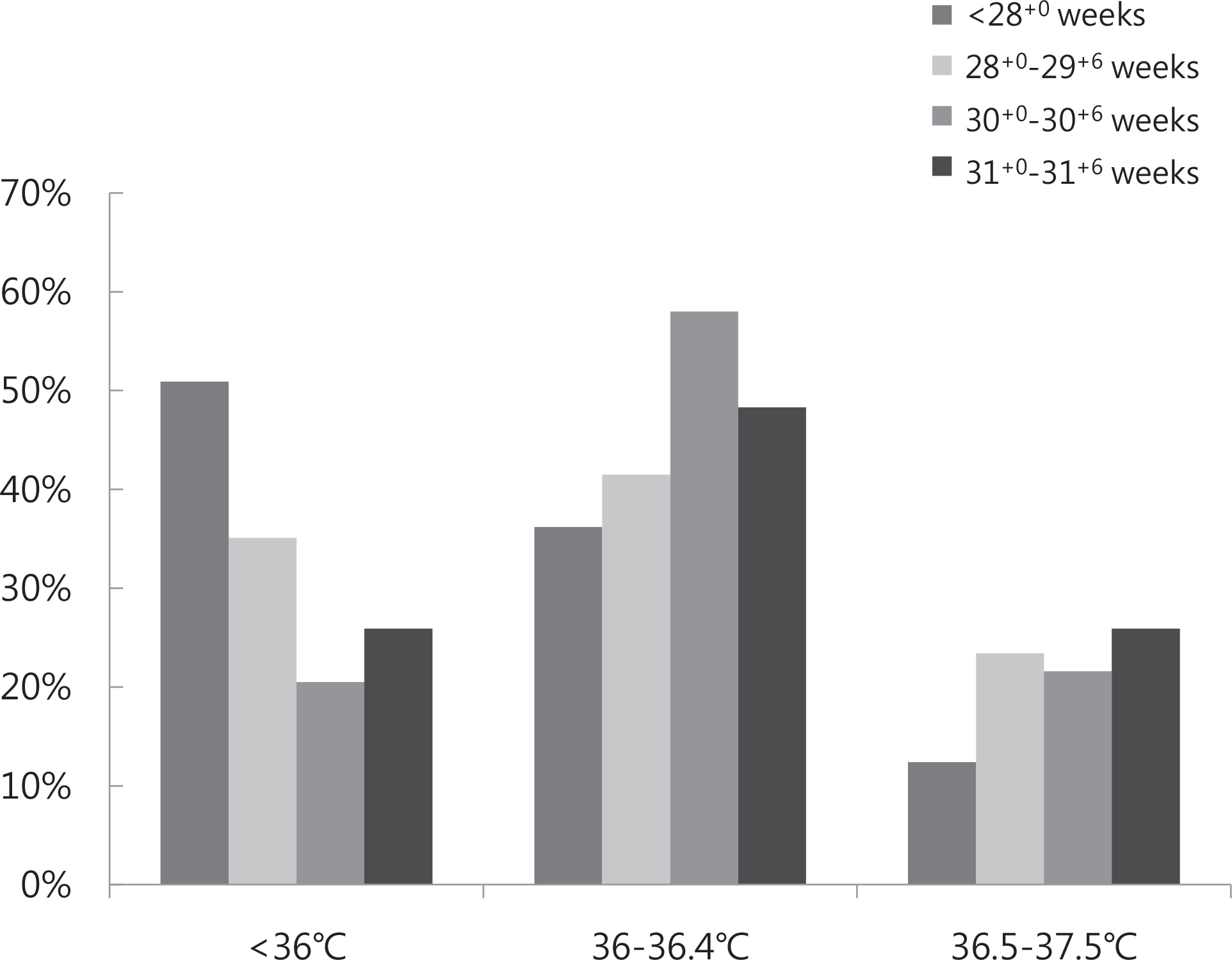
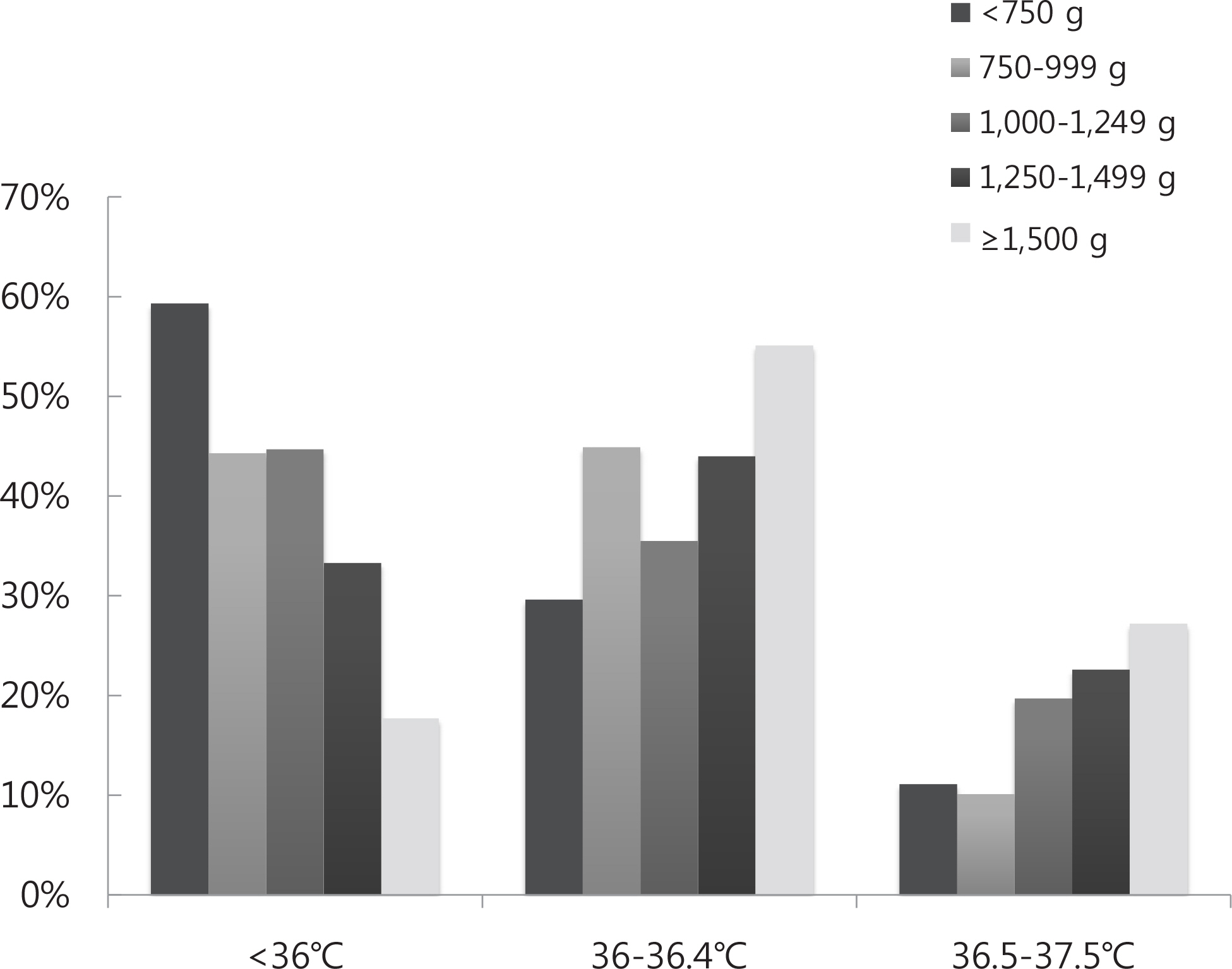
The incidence of hypothermia at admission was 33.5% in all patients, 50.9% of gestational age below 28 weeks and 48.4% of birth weight less than 1,000 g. Twenty-five (6.2%) infants did not gain appropriate body temperature within two hours after birth. Logistic regression analysis results showed that low birth weight, 1 minute Apgar score of < 7 and gestational diabetes were hypothermic risk factors immediately after admission.
CONCLUSION
To prevent hypothermia at the time of admission in premature infants, more active treatment is needed to maintain body temperature from the place of delivery when gestational diabetes mellitus or Apgar score of < 7 is present, in addition to low birth weight.
Keyword
MeSH Terms
Figure
Reference
-
1). Day RL., Caliguiri L., Kamenski C., Ehrlich F. Body temperature and survival of premature infants. Pediatrics. 1964. 34:171–81.
Article2). Li S., Guo P., Zou Q., He F., Xu F., Tan L. Efficacy and safety of plastic wrap for prevention of hypothermia after birth and during NICU in preterm infants: a systematic review and meta-analysis. PLoS One. 2016. 11:e0156960.
Article3). Harms K., Herting E., Kron M., Schill M., Schiffmann H. Importance of pre-and perinatal risk factors in respiratory distress syndrome of premature infants. A logical regression analysis of 1100 cases. Z Geburtshilfe Neonatol. 1997. 201:258–62.4). Yu VY., Joseph R., Bajuk B., Orgill A., Astbury J. Perinatal risk factors for necrotizing enterocolitis. Arch Dis Child. 1984. 59:430–4.
Article5). Herting E., Speer CP., Harms K., Robertson B., Curstedt T., Halliday HL, et al. Factors influencing morbidity and mortality in infants with severe respiratory distress syndrome treated with single or multiple doses of a natural porcine surfactant. Biol Neonate. 1992. 61(Suppl 1):26–30.
Article6). Kim JK., Seong SI., Shin JH., Jeong JM., Ahn SY., Kim ES, et al. Effect of clinical strategy for preventing heat loss between 23 and 24 weeks of gestation. J Korean Soc Neonatol. 2012. 19:26–31.
Article7). Meyer MP., Payton MJ., Salmon A., Hutchinson C., de Klerk A. A clinical comparison of radiant warmer and incubator care for preterm infants from birth to 1800 grams. Pediatrics. 2001. 108:395–401.
Article8). Knobel RB., Holditch-Davis D., Schwartz TA. Optimal body temperature in transitional extremely low birth weight infants using heart rate and temperature as indicators. J Obstet Gynecol Neonatal Nurs. 2010. 39:3–14.
Article9). Costeloe K., Hennessy E., Gibson AT., Marlow N., Wilkinson AR. The EPICure study: outcomes to discharge from hospital for infants born at the threshold of viability. Pediatrics. 2000. 106:659–71.
Article10). Knobel RB., Wimmer JE Jr., Holbert D. Heat loss prevention for preterm infants in the delivery room. J Perinatol. 2005. 25:304–8.
Article11). Thomas KA. Preterm infant thermal responses to caregiving differ by incubator control mode. J Perinatol. 2003. 23:640–5.
Article12). World Health Organization. Maternal and Newborn Health/Safe Motherhood. Thermal protection of the newborn: a practical guide. Geneva: World Health Organization. 1997. 64.13). Committee on Obstetric Practice. Committee Opinion No. 713: antenatal corticosteroid therapy for fetal maturation. Obstet Gynecol. 2017. 130:e102–9.14). Laptook AR., Salhab W., Bhaskar B. Neonatal Research Network. Admission temperature of low birth weight infants: predictors and associated morbidities. Pediatrics. 2007. 119:e643–9.
Article15). de Almeida MF., Guinsburg R., Sancho GA., Rosa IR., Lamy ZC., Martinez FE, et al. Hypothermia and early neonatal mortality in preterm infants. J Pediatr. 2014. 164:271–5. .e1.
Article16). Lyu Y., Shah PS., Ye XY., Warre R., Piedboeuf B., Deshpandey A, et al. Association between admission temperature and mortality and major morbidity in preterm infants born at fewer than 33 weeks' gestation. JAMA Pediatr. 2015. 169:e150277.
Article17). Wyllie J., Perlman JM., Kattwinkel J., Wyckoff MH., Aziz K., Guinsburg R, et al. Part 7: neonatal resuscitation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2015. 95:e169–201.18). Bissinger RL., Annibale DJ. Thermoregulation in very low-birth-weight infants during the golden hour: results and implications. Adv Neonatal Care. 2010. 10:230–8.19). Lee JA. Delivery room management: first step to the best neonatal outcome. Korean J Perinatol. 2015. 26:12–20.
Article20). Rohana J., Khairina W., Boo NY., Shareena I. Reducing hypothermia in preterm infants with polyethylene wrap. Pediatr Int. 2011. 53:468–74.
Article21). McCall EM., Alderdice F., Halliday HL., Jenkins JG., Vohra S. Interventions to prevent hypothermia at birth in preterm and/or low birthweight infants. Cochrane Database Syst Rev. 2010. 3:CD004210.
Article22). Jang JH., Shin SH., Woo HK., Choi EK., Song IG., Shin SH, et al. The association between admission hypothermia and neonatal outcomes in very low birth weight infants. Neonatal Med. 2016. 23:183–9.
Article23). Wilson E., Maier RF., Norman M., Misselwitz B., Howell EA., Zeitlin J, et al. Admission hypothermia in very preterm infants and neonatal mortality and morbidity. J Pediatr. 2016. 175:61–7. .e4.
Article24). Chung JH. Obstetrical management of late preterm pregnancy. Perinatology. 2016. 27:195–204.
Article25). Jo HS. Initial optimal body temperature in preterm infants. Neonatal Med. 2014. 21:85–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Initial Optimal Body Temperature in Preterm Infants
- The impact of a quality improvement effort in reducing admission hypothermia in preterm infants following delivery
- The Risk of Repeated Preterm Birth
- Risk factors of preterm delivery and survival rate of preterm infants in Bucheon
- The Use of Probiotics in Preterm Infants