Neonatal Med.
2022 May;29(2):68-75. 10.5385/nm.2022.29.2.68.
The Use of Probiotics in Preterm Infants
- Affiliations
-
- 1Department of Pediatrics, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea
- KMID: 2530609
- DOI: http://doi.org/10.5385/nm.2022.29.2.68
Abstract
- Probiotics are live microorganisms that positively affect host health by altering the composition of the host microbiota. Gastrointestinal dysbiosis refers to adverse alterations of the intestinal flora and is associated with several diseases, including necrotizing enterocolitis, late-onset sepsis in preterm infants as well as atopic disease, colic, diabetes, and diarrhea in term infants. The risk factors for gastrointestinal dysbiosis are preterm birth, cesarean section delivery, and formula feeding, in contrast to term birth infants, vaginal delivery and breast milk feeding. Probiotics have been used to restore synbiosis in infants with gastrointestinal dysbiosis. Probiotics inhibit colonization of pathogenic bacteria in the gastrointestinal tract, thereby improving the barrier function of the gastrointestinal tract, and the immune function. In preterm infants, probiotics reduce mortality as well as rates of necrotizing enterocolitis and late-onset sepsis. The combined use of probiotics such as Lactobacillus and Bifidobacterium and the combination of probiotics with prebiotics yield better outcomes in the prevention of necrotizing enterocolitis than those achieved with a single pro- or prebiotic strain. However, the routine use of probiotics has been hindered by the lack of pharmaceutical-quality products, and a definite effect has yet to be demonstrated in preterm infants with a birth weight <1,000 g. Therefore, to reduce the risk of necrotizing enterocolitis in preterm infants, probiotics should be provided along with breast milk and other strategies aimed at preventing gastrointestinal dysbiosis.
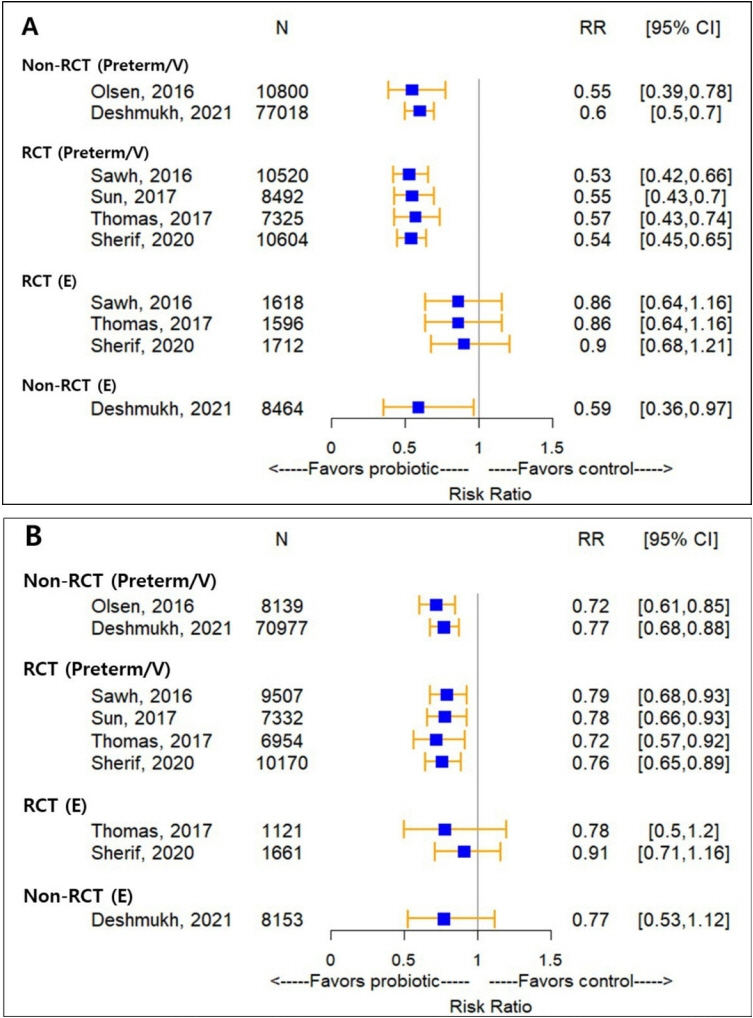
Figure
Reference
-
1. Zbinden A, Zbinden R, Berger C, Arlettaz R. Case series of Bifidobacterium longum bacteremia in three preterm infants on probiotic therapy. Neonatology. 2015; 107:56–9.2. Di Mauro A, Neu J, Riezzo G, Raimondi F, Martinelli D, Francavilla R, et al. Gastrointestinal function development and microbiota. Ital J Pediatr. 2013; 39:15.3. Underwood MA, Sohn K. The microbiota of the extremely preterm infant. Clin Perinatol. 2017; 44:407–27.4. Underwood MA, Mukhopadhyay S, Lakshminrusimha S, Bevins CL. Neonatal intestinal dysbiosis. J Perinatol. 2020; 40:1597–608.5. Poindexter B; Committee on Fetus and Newborn. Use of probiotics in preterm infants. Pediatrics. 2021; 147:e2021051485.6. Patel RM, Pammi M. Probiotics for preterm infants: which one(s) to choose? Pediatrics. 2021; 147:e2020039735.7. Johnson-Henry KC, Abrahamsson TR, Wu RY, Sherman PM. Probiotics, prebiotics, and synbiotics for the prevention of necrotizing enterocolitis. Adv Nutr. 2016; 7:928–37.8. Underwood MA, Salzman NH, Bennett SH, Barman M, Mills DA, Marcobal A, et al. A randomized placebo-controlled com parison of 2 prebiotic/probiotic combinations in preterm infants: impact on weight gain, intestinal microbiota, and fecal short-chain fatty acids. J Pediatr Gastroenterol Nutr. 2009; 48:216–25.9. Buccigrossi V, de Marco G, Bruzzese E, Ombrato L, Bracale I, Polito G, et al. Lactoferrin induces concentration-dependent functional modulation of intestinal proliferation and differentiation. Pediatr Res. 2007; 61:410–4.10. Senn V, Bassler D, Choudhury R, Scholkmann F, Righini-Grunder F, Vuille-Dit-Bile RN, et al. Microbial colonization from the fetus to early childhood: a comprehensive review. Front Cell Infect Microbiol. 2020; 10:573735.11. D’Argenio V. The prenatal microbiome: a new player for human health. High Throughput. 2018; 7:38.12. Milani C, Duranti S, Bottacini F, Casey E, Turroni F, Mahony J, et al. The first microbial colonizers of the human gut: composition, activities, and health implications of the infant gut microbiota. Microbiol Mol Biol Rev. 2017; 81:e00036–17.13. Gritz EC, Bhandari V. The human neonatal gut microbiome: a brief review. Front Pediatr. 2015; 3:17.14. Westerbeek EA, van den Berg A, Lafeber HN, Knol J, Fetter WP, van Elburg RM. The intestinal bacterial colonisation in preterm infants: a review of the literature. Clin Nutr. 2006; 25:361–8.15. Patel RM, Underwood MA. Probiotics and necrotizing enterocolitis. Semin Pediatr Surg. 2018; 27:39–46.16. Patel RM, Myers LS, Kurundkar AR, Maheshwari A, Nusrat A, Lin PW. Probiotic bacteria induce maturation of intestinal claudin 3 expression and barrier function. Am J Pathol. 2012; 180:626–35.17. Sharif S, Meader N, Oddie SJ, Rojas-Reyes MX, McGuire W. Probiotics to prevent necrotising enterocolitis in very preterm or very low birth weight infants. Cochrane Database Syst Rev. 2020; 10:CD005496.18. Walker WA. Mechanisms of action of probiotics. Clin Infect Dis. 2008; 46 Suppl 2:S87–91.19. Guo S, Gillingham T, Guo Y, Meng D, Zhu W, Walker WA, et al. Secretions of Bifidobacterium infantis and Lactobacillus acidophilus protect intestinal epithelial barrier function. J Pediatr Gastroenterol Nutr. 2017; 64:404–12.20. Vincenzi A, Goettert MI, Volken de Souza CF. An evaluation of the effects of probiotics on tumoral necrosis factor (TNF-α) signaling and gene expression. Cytokine Growth Factor Rev. 2021; 57:27–38.21. Lin PW, Myers LE, Ray L, Song SC, Nasr TR, Berardinelli AJ, et al. Lactobacillus rhamnosus blocks inflammatory signaling in vivo via reactive oxygen species generation. Free Radic Biol Med. 2009; 47:1205–11.22. Litvak Y, Byndloss MX, Tsolis RM, Baumler AJ. Dysbiotic Proteobacteria expansion: a microbial signature of epithelial dysfunction. Curr Opin Microbiol. 2017; 39:1–6.23. Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 2011; 364:255–64.24. Hackam DJ, Sodhi CP. Toll-like receptor-mediated intestinal inflammatory imbalance in the pathogenesis of necrotizing enterocolitis. Cell Mol Gastroenterol Hepatol. 2018; 6:229–38.25. van den Akker CH, van Goudoever JB, Shamir R, Domellof M, Embleton ND, Hojsak I, et al. Probiotics and preterm infants: a position paper by the European Society for Paediatric Gastroenterology Hepatology and Nutrition Committee on Nutrition and the European Society for Paediatric Gastroenterology Hepatology and Nutrition Working Group for Probiotics and Prebiotics. J Pediatr Gastroenterol Nutr. 2020; 70:664–80.26. Olsen R, Greisen G, Schroder M, Brok J. Prophylactic probiotics for preterm infants: a systematic review and meta-analysis of observational studies. Neonatology. 2016; 109:105–12.27. Jacobs SE, Tobin JM, Opie GF, Donath S, Tabrizi SN, Pirotta M, et al. Probiotic effects on late-onset sepsis in very preterm infants: a randomized controlled trial. Pediatrics. 2013; 132:1055–62.28. Costeloe K, Hardy P, Juszczak E, Wilks M, Millar MR; Probiotics in Preterm Infants Study Collaborative Group. Bifidobacterium breve BBG-001 in very preterm infants: a randomised controlled phase 3 trial. Lancet. 2016; 387:649–60.29. Razak A, Patel RM, Gautham KS. Use of probiotics to prevent necrotizing enterocolitis: evidence to clinical practice. JAMA Pediatr. 2021; 175:773–4.30. Chi C, Li C, Buys N, Wang W, Yin C, Sun J. Effects of probiotics in preterm infants: a network meta-analysis. Pediatrics. 2021; 147:e20200706.31. Morgan RL, Preidis GA, Kashyap PC, Weizman AV, Sadeghirad B; McMaster Probiotic, Prebiotic, and Synbiotic Work Group. Probiotics reduce mortality and morbidity in preterm, lowbirth-weight infants: a systematic review and network metaanalysis of randomized trials. Gastroenterology. 2020; 159:467–80.32. Thomas DW, Greer FR; American Academy of Pediatrics Committee on Nutrition; American Academy of Pediatrics Section on Gastroenterology, Hepatology, and Nutrition. Probiotics and prebiotics in pediatrics. Pediatrics. 2010; 126:1217–31.33. Marchand V. Using probiotics in the paediatric population. Paediatr Child Health. 2012; 17:575–6.34. Su GL, Ko CW, Bercik P, Falck-Ytter Y, Sultan S, Weizman AV, et al. AGA clinical practice guidelines on the role of probiotics in the management of gastrointestinal disorders. Gastroenterology. 2020; 159:697–705.35. Qiao LX, Zhu WY, Zhang HY, Wang H. Effect of early administration of probiotics on gut microflora and feeding in pre-term infants: a randomized controlled trial. J Matern Fetal Neonatal Med. 2017; 30:13–6.36. Bertelli C, Pillonel T, Torregrossa A, Prod’hom G, Fischer CJ, Greub G, et al. Bifidobacterium longum bacteremia in preterm infants receiving probiotics. Clin Infect Dis. 2015; 60:924–7.37. Esaiassen E, Cavanagh P, Hjerde E, Simonsen GS, Stoen R, Klingenberg C. Bifidobacterium longum subspecies infantis bacteremia in 3 extremely preterm infants receiving probiotics. Emerg Infect Dis. 2016; 22:1664–6.38. Jenke A, Ruf EM, Hoppe T, Heldmann M, Wirth S. Bifidobacterium septicaemia in an extremely low-birthweight infant under probiotic therapy. Arch Dis Child Fetal Neonatal Ed. 2012; 97:F217–8.39. Vallabhaneni S, Walker TA, Lockhart SR, Ng D, Chiller T, Melchreit R, et al. Notes from the field: fatal gastrointestinal mucormycosis in a premature infant associated with a contaminated dietary supplement: Connecticut, 2014. MMWR Morb Mortal Wkly Rep. 2015; 64:155–6.40. Salminen MK, Tynkkynen S, Rautelin H, Saxelin M, Vaara M, Ruutu P, et al. Lactobacillus bacteremia during a rapid increase in probiotic use of Lactobacillus rhamnosus GG in Finland. Clin Infect Dis. 2002; 35:1155–60.41. Kane AF, Bhatia AD, Denning PW, Shane AL, Patel RM. Routine supplementation of Lactobacillus rhamnosus GG and risk of necrotizing enterocolitis in very low birth weight infants. J Pediatr. 2018; 195:73–9.42. Kim SN, Lee HY, Kim S, Lee BK, Jung YH, Huh J, et al. A case of Lactobacillus bacteremia during probiotic supplementation in a very preterm infant with short bowel syndrome. Neonatal Med. 2015; 22:173–6.43. Jacobs SE, Hickey L, Donath S, Opie GF, Anderson PJ, Garland SM, et al. Probiotics, prematurity and neurodevelopment: follow-up of a randomised trial. BMJ Paediatr Open. 2017; 1:e000176.44. Upadhyay RP, Taneja S, Chowdhury R, Strand TA, Bhandari N. Effect of prebiotic and probiotic supplementation on neurodevelopment in preterm very low birth weight infants: findings from a meta-analysis. Pediatr Res. 2020; 87:811–22.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intestinal Microbiota in Preterm Infants and Probiotics Use for Disease Prevention
- Probiotics and Necrotizing Enterocolitis
- The Optimal Time for Initiating Probiotics for Preterm and VeryLow-Birth-Weight Infants: A 10-Year Experience in a Single Neonatal Intensive Care Unit
- A Case of Lactobacillus Bacteremia during Probiotic Supplementation in a Very Preterm Infant with Short Bowel Syndrome
- Neurodevelopmental outcomes of preterm infants