Ann Hepatobiliary Pancreat Surg.
2018 Feb;22(1):27-35. 10.14701/ahbps.2018.22.1.27.
Bridging therapies to liver transplantation for hepatocellular carcinoma: A bridge to nowhere?
- Affiliations
-
- 1Division of Hepatobiliary and Pancreatic Surgery and Liver Transplantation, Department of Surgery, University Surgical Cluster, National University Health System, Singapore, Singapore. alfred_kow@nuhs.edu.sg
- 2Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore.
- 3Department of Gastroenterology and Hepatology, National University Health System, Singapore, Singapore.
- 4National University Centre for Organ Transplantation, National University Health System, Singapore, Singapore.
- KMID: 2409077
- DOI: http://doi.org/10.14701/ahbps.2018.22.1.27
Abstract
- BACKGROUNDS/AIMS
Liver Transplantation (LT) is a recognized treatment for Hepatocellular Carcinoma (HCC). The role of Bridging Therapies (BT) remains controversial.
METHODS
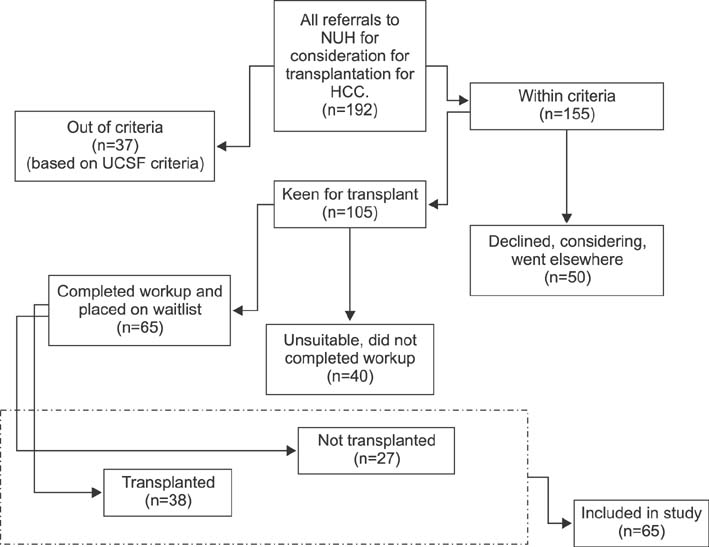
From January 2001 to October 2012, 192 patients were referred to the National University Hospital, Singapore for consideration of LT for HCC. Sixty-five patients (33.8%) were found suitable for transplant and were placed on the waitlist. Analysis was performed in these patients.
RESULTS
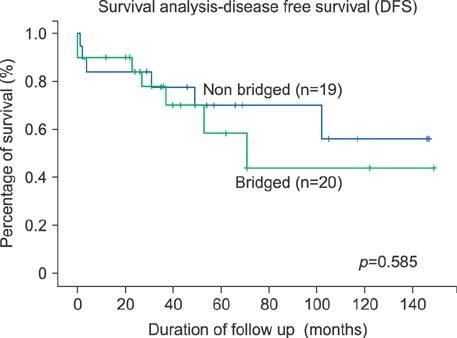
The most common etiology of HCC was Hepatitis B (n=28, 43.1%). Thirty-six patients (55.4%) received BT. Seventeen patients (47.2%) received TACE only, while 10 patients (27.8%) received radiofrequency ablation (RFA) only. The remaining patients received a combination of transarterial chemoembolization (TACE) and RFA. Baseline tumor and patient characteristics were comparable between the two groups. The overall dropout rate was 44.4% and 31.0% in the BT and non-BT groups, respectively (p=0.269). The dropout rate due to disease progression beyond criteria was 6.9% (n=2) in the non-bridged group and 22.2% (n=8) in the bridged group (p=0.089). Thirty-nine patients (60%) underwent LT, of which all patients who underwent Living Donor LT did not receive BT (n=4, 21.1%, p=0.030). The median time to LT was 180 days (range, 20-558 days) in the non-BT group and 291 days (range, 17-844 days) in the BT group (p=0.214). There was no difference in survival or recurrence between the BT and non-BT groups (p=0.862).
CONCLUSIONS
BT does not influence the dropout rate or survival after LT but it should be considered in patients who are on the waitlist for more than 6 months.
MeSH Terms
Figure
Cited by 1 articles
-
The impact of waiting time and delayed treatment on the outcomes of patients with hepatocellular carcinoma: A systematic review and meta-analysis
Feng Yi Cheo, Celeste Hong Fei Lim, Kai Siang Chan, Vishal Girishchandra Shelat
Ann Hepatobiliary Pancreat Surg. 2024;28(1):1-13. doi: 10.14701/ahbps.23-090.
Reference
-
1. Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996; 334:693–699.
Article2. Yao FY, Ferrell L, Bass NM, Watson JJ, Bacchetti P, Venook A, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001; 33:1394–1403.
Article3. Lim SG, Wai CT, Da Costa M, Sutedja DS, Lee YM, Lee KH, et al. Referral patterns and waiting times for liver transplantation in Singapore. Singapore Med J. 2006; 47:599–603.4. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009; 45:228–247.
Article5. OPTN. Organ Procurement and Transplantation Network Policies. Richmond: OPTN;2016. cited 2016 Mar 26. Available from: https://optn.transplant.hrsa.gov/media/1200/optn_policies.pdf#nameddest=Policy_09.6. Terzi E, Ray Kim W, Sanchez W, Charlton MR, Schmeltzer P, Gores GJ, et al. Impact of multiple transarterial chemoembolization treatments on hepatocellular carcinoma for patients awaiting liver transplantation. Liver Transpl. 2015; 21:248–257.
Article7. Lesurtel M, Müllhaupt B, Pestalozzi BC, Pfammatter T, Clavien PA. Transarterial chemoembolization as a bridge to liver transplantation for hepatocellular carcinoma: an evidence-based analysis. Am J Transplant. 2006; 6:2644–2650.
Article8. Fujiki M, Aucejo F, Choi M, Kim R. Neo-adjuvant therapy for hepatocellular carcinoma before liver transplantation: where do we stand? World J Gastroenterol. 2014; 20:5308–5319.
Article9. Alba E, Valls C, Dominguez J, Martinez L, Escalante E, Lladó L, et al. Transcatheter arterial chemoembolization in patients with hepatocellular carcinoma on the waiting list for orthotopic liver transplantation. AJR Am J Roentgenol. 2008; 190:1341–1348.
Article10. Mazzaferro V, Battiston C, Perrone S, Pulvirenti A, Regalia E, Romito R, et al. Radiofrequency ablation of small hepatocellular carcinoma in cirrhotic patients awaiting liver transplantation: a prospective study. Ann Surg. 2004; 240:900–909.11. Lu DS, Yu NC, Raman SS, Lassman C, Tong MJ, Britten C, et al. Percutaneous radiofrequency ablation of hepatocellular carcinoma as a bridge to liver transplantation. Hepatology. 2005; 41:1130–1137.
Article12. Tsochatzis E, Garcovich M, Marelli L, Papastergiou V, Fatourou E, Rodriguez-Peralvarez ML, et al. Transarterial embolization as neo-adjuvant therapy pretransplantation in patients with hepatocellular carcinoma. Liver Int. 2013; 33:944–949.
Article13. Freeman RB Jr, Steffick DE, Guidinger MK, Farmer DG, Berg CL, Merion RM. Liver and intestine transplantation in the United States, 1997-2006. Am J Transplant. 2008; 8:958–976.
Article14. Majno PE, Adam R, Bismuth H, Castaing D, Ariche A, Krissat J, et al. Influence of preoperative transarterial lipiodol chemoembolization on resection and transplantation for hepatocellular carcinoma in patients with cirrhosis. Ann Surg. 1997; 226:688–701. discussion 701-703.
Article15. Lai Q, Avolio AW, Graziadei I, Otto G, Rossi M, Tisone G, et al. Alpha-fetoprotein and modified response evaluation criteria in solid tumors progression after locoregional therapy as predictors of hepatocellular cancer recurrence and death after transplantation. Liver Transpl. 2013; 19:1108–1118.
Article16. Yao FY, Kerlan RK Jr, Hirose R, Davern TJ 3rd, Bass NM, Feng S, et al. Excellent outcome following down-staging of hepatocellular carcinoma prior to liver transplantation: an intention-to-treat analysis. Hepatology. 2008; 48:819–827.
Article17. De Carlis L, Di Sandro S, Giacomoni A, Slim A, Lauterio A, Mangoni I, et al. Beyond the Milan criteria: what risks for patients with hepatocellular carcinoma progression before liver transplantation? J Clin Gastroenterol. 2012; 46:78–86.18. Otto G, Herber S, Heise M, Lohse AW, Mönch C, Bittinger F, et al. Response to transarterial chemoembolization as a biological selection criterion for liver transplantation in hepatocellular carcinoma. Liver Transpl. 2006; 12:1260–1267.
Article19. Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology. 1999; 30:1434–1440.
Article20. Ashoori N, Bamberg F, Paprottka P, Rentsch M, Kolligs FT, Siegert S, et al. Multimodality treatment for early-stage hepatocellular carcinoma: a bridging therapy for liver transplantation. Digestion. 2012; 86:338–348.
Article21. Llovet JM, Mas X, Aponte JJ, Fuster J, Navasa M, Christensen E, et al. Cost effectiveness of adjuvant therapy for hepatocellular carcinoma during the waiting list for liver transplantation. Gut. 2002; 50:123–128.
Article22. Majno P, Lencioni R, Mornex F, Girard N, Poon RT, Cherqui D. Is the treatment of hepatocellular carcinoma on the waiting list necessary? Liver Transpl. 2011; 17:Suppl 2. S98–S108.
Article23. Yao FY, Bass NM, Nikolai B, Merriman R, Davern TJ, Kerlan R, et al. A follow-up analysis of the pattern and predictors of dropout from the waiting list for liver transplantation in patients with hepatocellular carcinoma: implications for the current organ allocation policy. Liver Transpl. 2003; 9:684–692.
Article24. Graziadei IW, Sandmueller H, Waldenberger P, Koenigsrainer A, Nachbaur K, Jaschke W, et al. Chemoembolization followed by liver transplantation for hepatocellular carcinoma impedes tumor progression while on the waiting list and leads to excellent outcome. Liver Transpl. 2003; 9:557–563.
Article25. Decaens T, Roudot-Thoraval F, Bresson-Hadni S, Meyer C, Gugenheim J, Durand F, et al. Impact of pretransplantation transarterial chemoembolization on survival and recurrence after liver transplantation for hepatocellular carcinoma. Liver Transpl. 2005; 11:767–775.
Article26. Han K, Tzimas GN, Barkun JS, Metrakos P, Tchervenkov JL, Hilzenrat N, et al. Preoperative alpha-fetoprotein slope is predictive of hepatocellular carcinoma recurrence after liver transplantation. Can J Gastroenterol. 2007; 21:39–45.
Article27. Soriano A, Varona A, Gianchandani R, Moneva ME, Arranz J, Gonzalez A, et al. Selection of patients with hepatocellular carcinoma for liver transplantation: Past and future. World J Hepatol. 2016; 8:58–68.
Article28. Clavien PA, Lesurtel M, Bossuyt PM, Gores GJ, Langer B, Perrier A. Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. Lancet Oncol. 2012; 13:e11–e22.
Article29. Lu DS, Yu NC, Raman SS, Limanond P, Lassman C, Murray K, et al. Radiofrequency ablation of hepatocellular carcinoma: treatment success as defined by histologic examination of the explanted liver. Radiology. 2005; 234:954–960.
Article30. Agopian VG, Morshedi MM, McWilliams J, Harlander-Locke MP, Markovic D, Zarrinpar A, et al. Complete pathologic response to pretransplant locoregional therapy for hepatocellular carcinoma defines cancer cure after liver transplantation: analysis of 501 consecutively treated patients. Ann Surg. 2015; 262:536–545. discussion 543-545.31. Kornberg A, Witt U, Matevossian E, Küpper B, Assfalg V, Drzezga A, et al. Extended postinterventional tumor necrosis-implication for outcome in liver transplant patients with advanced HCC. PLoS One. 2013; 8:e53960.
Article32. Cescon M, Cucchetti A, Ravaioli M, Pinna AD. Hepatocellular carcinoma locoregional therapies for patients in the waiting list. Impact on transplantability and recurrence rate. J Hepatol. 2013; 58:609–618.
Article33. Garwood ER, Fidelman N, Hoch SE, Kerlan RK Jr, Yao FY. Morbidity and mortality following transarterial liver chemoembolization in patients with hepatocellular carcinoma and synthetic hepatic dysfunction. Liver Transpl. 2013; 19:164–173.
Article34. Hsin IF, Hsu CY, Huang HC, Huang YH, Lin HC, Lee RC, et al. Liver failure after transarterial chemoembolization for patients with hepatocellular carcinoma and ascites: incidence, risk factors, and prognostic prediction. J Clin Gastroenterol. 2011; 45:556–562.35. Kothary N, Weintraub JL, Susman J, Rundback JH. Transarterial chemoembolization for primary hepatocellular carcinoma in patients at high risk. J Vasc Interv Radiol. 2007; 18:1517–1526. quiz 1527.
Article36. Park MS, Lee KW, Suh SW, You T, Choi Y, Kim H, et al. Living-donor liver transplantation associated with higher incidence of hepatocellular carcinoma recurrence than deceased-donor liver transplantation. Transplantation. 2014; 97:71–77.
Article37. Fisher RA, Kulik LM, Freise CE, Lok AS, Shearon TH, Brown RS Jr, et al. Hepatocellular carcinoma recurrence and death following living and deceased donor liver transplantation. Am J Transplant. 2007; 7:1601–1608.
Article38. Lo CM, Fan ST, Liu CL, Chan SC, Ng IO, Wong J. Living donor versus deceased donor liver transplantation for early irresectable hepatocellular carcinoma. Br J Surg. 2007; 94:78–86.
Article39. Kulik LM, Fisher RA, Rodrigo DR, Brown RS Jr, Freise CE, Shaked A, et al. Outcomes of living and deceased donor liver transplant recipients with hepatocellular carcinoma: results of the A2ALL cohort. Am J Transplant. 2012; 12:2997–3007.
Article40. Chan SC. Section 2. Small-for-size liver graft and hepatocellular carcinoma recurrence. Transplantation. 2014; 97:Suppl 8. S7–S10.
Article41. Ninomiya M, Shirabe K, Facciuto ME, Schwartz ME, Florman SS, Yoshizumi T, et al. Comparative study of living and deceased donor liver transplantation as a treatment for hepatocellular carcinoma. J Am Coll Surg. 2015; 220:297–304.e3.
Article42. Liang W, Wu L, Ling X, Schroder PM, Ju W, Wang D, et al. Living donor liver transplantation versus deceased donor liver transplantation for hepatocellular carcinoma: a meta-analysis. Liver Transpl. 2012; 18:1226–1236.
Article43. Grant RC, Sandhu L, Dixon PR, Greig PD, Grant DR, McGilvray ID. Living vs. deceased donor liver transplantation for hepatocellular carcinoma: a systematic review and meta-analysis. Clin Transplant. 2013; 27:140–147.
Article44. Roberts JP, Venook A, Kerlan R, Yao F. Hepatocellular carcinoma: Ablate and wait versus rapid transplantation. Liver Transpl. 2010; 16:925–929.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Liver transplantation for hepatocellular carcinoma with portal vein tumor thrombosis
- Liver Transplantation for Hepatocellular Carcinoma
- Can hepatocellular carcinoma recurrence be prevented after liver transplantation?
- Stereotactic Body Radiotherapy: Does It Have a Role in Management of Hepatocellular Carcinoma?
- Sorafenib for Recurrent Hepatocellular Carcinoma after Liver Transplantation