J Korean Med Assoc.
2018 Feb;61(2):125-129. 10.5124/jkma.2018.61.2.125.
Diagnosis and treatment of acute rhinosinusitis in children
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. hyunjulee@snu.ac.kr
- KMID: 2409020
- DOI: http://doi.org/10.5124/jkma.2018.61.2.125
Abstract
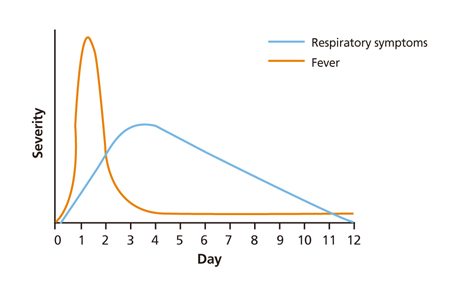
- Acute rhinosinusitis is a common entity in children, most are due to viral infections, however up to over 80% children with rhinosinusitis are prescribed with antibiotics. Acute bacterial sinusitis should be diagnosed in when a child has 1) a severe onset with a fever over 39℃, purulent nasal discharge or facial pain for 3 to 4 days; 2) persistent illness with rhinorrhea, daytime cough or both for over 10 days with no clinical improvement; or 3) worsening course with symptoms aggravating or new onset symptoms including fever, headache, cough or rhinorrhea after clinical improvement. Radiographic imaging is not recommended for differentiation of viral and bacterial rhinosinusitis, however a contrast-enhanced computed tomography or magnetic resonance imaging may be done in cases with orbital or central nervous system complications. Antibiotics may be prescribed in cases with severe onset or worsening course. Antibiotics may be prescribed after additional observation for 3 days in children with persistent illness. Amoxicillin-clavulanate (amoxicillin 40 to 50 mg/kg/day, every 12 hours) is recommended for initial treatment and high dose amoxicillin-clavulanate (amoxicillin 90 mg/kg/day every 12 hours) may be considered in cases with severe infection, children in day care center, under 2 years of age, recent admission history, previous antibiotics within 1 month and immunocompromised children. Clinical response should be reassessed in cases of worsening or failure to improve within 72 hours of treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Revai K, Dobbs LA, Nair S, Patel JA, Grady JJ, Chonmaitree T. Incidence of acute otitis media and sinusitis complicating upper respiratory tract infection: the effect of age. Pediatrics. 2007; 119:e1408–e1412.
Article2. Gwaltney JM Jr, Wiesinger BA, Patrie JT. Acute community-acquired bacterial sinusitis: the value of antimicrobial treatment and the natural history. Clin Infect Dis. 2004; 38:227–233.
Article3. DeMuri GP, Gern JE, Moyer SC, Lindstrom MJ, Lynch SV, Wald ER. Clinical features, virus identification, and sinusitis as a complication of upper respiratory tract illness in children ages 4-7 years. J Pediatr. 2016; 171:133–139.e1.4. Kronman MP, Zhou C, Mangione-Smith R. Bacterial prevalence and antimicrobial prescribing trends for acute respiratory tract infections. Pediatrics. 2014; 134:e956–e965.
Article5. Korea Centers for Disease Control and Prevention. Guidelines for the antibiotic use in children with acute upper respiratory tract infections. Cheongju: Korea Centers for Disease Control and Prevention;2016.6. Gwaltney JM Jr. Acute community-acquired sinusitis. Clin Infect Dis. 1996; 23:1209–1223.
Article7. Wald ER, Milmoe GJ, Bowen A, Ledesma-Medina J, Salamon N, Bluestone CD. Acute maxillary sinusitis in children. N Engl J Med. 1981; 304:749–754.
Article8. Wald ER, Reilly JS, Casselbrant M, Ledesma-Medina J, Milmoe GJ, Bluestone CD, Chiponis D. Treatment of acute maxillary sinusitis in childhood: a comparative study of amoxicillin and cefaclor. J Pediatr. 1984; 104:297–302.
Article9. Parsons DS, Wald ER. Otitis media and sinusitis: similar diseases. Otolaryngol Clin North Am. 1996; 29:11–25.
Article10. Casey JR, Adlowitz DG, Pichichero ME. New patterns in the otopathogens causing acute otitis media six to eight years after introduction of pneumococcal conjugate vaccine. Pediatr Infect Dis J. 2010; 29:304–309.
Article11. Wald ER, Applegate KE, Bordley C, Darrow DH, Glode MP, Marcy SM, Nelson CE, Rosenfeld RM, Shaikh N, Smith MJ, Williams PV, Weinberg ST. American Academy of Pediatrics. Clinical practice guideline for the diagnosis and management of acute bacterial sinusitis in children aged 1 to 18 years. Pediatrics. 2013; 132:e262–e280.
Article12. Choe YJ, Lee HJ, Lee H, Oh CE, Cho EY, Choi JH, Kang HM, Yoon IA, Jung HJ, Choi EH. Emergence of antibiotic-resistant non-vaccine serotype pneumococci in nasopharyngeal carriage in children after the use of extended-valency pneumococcal conjugate vaccines in Korea. Vaccine. 2016; 34:4771–4776.
Article13. Meltzer EO, Hamilos DL, Hadley JA, Lanza DC, Marple BF, Nicklas RA, Bachert C, Baraniuk J, Baroody FM, Benninger MS, Brook I, Chowdhury BA, Druce HM, Durham S, Ferguson B, Gwaltney JM Jr, Kaliner M, Kennedy DW, Lund V, Naclerio R, Pawankar R, Piccirillo JF, Rohane P, Simon R, Slavin RG, Togias A, Wald ER, Zinreich SJ. American Academy of Allergy, Asthma and Immunology. American Academy of Otolaryngic Allergy. American Academy of Otolaryngology-Head and Neck Surgery. American College of Allergy, Asthma and Immunology. American Rhinologic Society. Rhinosinusitis: establishing definitions for clinical research and patient care. Otolaryngol Head Neck Surg. 2004; 131:6 Suppl. S1–S62.
Article14. Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJ, Hicks LA, Pankey GA, Seleznick M, Volturo G, Wald ER, File TM Jr. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012; 54:e72–e112.
Article15. Kovatch AL, Wald ER, Ledesma-Medina J, Chiponis DM, Bedingfield B. Maxillary sinus radiographs in children with nonrespiratory complaints. Pediatrics. 1984; 73:306–308.
Article16. Shopfner CE, Rossi JO. Roentgen evaluation of the paranasal sinuses in children. Am J Roentgenol Radium Ther Nucl Med. 1973; 118:176–186.
Article17. Diament MJ, Senac MO Jr, Gilsanz V, Baker S, Gillespie T, Larsson S. Prevalence of incidental paranasal sinuses opacification in pediatric patients: a CT study. J Comput Assist Tomogr. 1987; 11:426–431.
Article18. Kristo A, Alho OP, Luotonen J, Koivunen P, Tervonen O, Uhari M. Cross-sectional survey of paranasal sinus magnetic resonance imaging findings in schoolchildren. Acta Paediatr. 2003; 92:34–36.
Article19. Kristo A, Uhari M, Luotonen J, Koivunen P, Ilkko E, Tapiainen T, Alho OP. Paranasal sinus findings in children during respiratory infection evaluated with magnetic resonance imaging. Pediatrics. 2003; 111(5 Pt 1):e586–e589.
Article20. Younis RT, Lazar RH, Anand VK. Intracranial complications of sinusitis: a 15-year review of 39 cases. Ear Nose Throat J. 2002; 81:636–638. 640–642. 644
Article21. Fallon RM, Kuti JL, Doern GV, Girotto JE, Nicolau DP. Pharmacodynamic target attainment of oral beta-lactams for the empiric treatment of acute otitis media in children. Paediatr Drugs. 2008; 10:329–335.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric Chronic Rhinosinusitis
- The diagnosis of pediatric sinusitis
- Clinical Characteristics and Treatment of Fungal Rhinosinusitis
- Factors associated with chronic and recurrent rhinosinusitis in preschool children with obstructive sleep apnea syndrome
- Medical treatment according to phenotypes of chronic rhinosinusitis