Endocrinol Metab.
2017 Dec;32(4):466-474. 10.3803/EnM.2017.32.4.466.
Characteristics of Korean Patients with Primary Adrenal Insufficiency: A Registry-Based Nationwide Survey in Korea
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. swkimmd@snu.ac.kr
- 2Department of Internal Medicine, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea.
- 3Department of Internal Medicine, Hallym University Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea.
- 4Department of Internal Medicine, Gyeongsang National University Changwon Hospital, Gyeongsang National University School of Medicine, Changwon, Korea.
- KMID: 2406191
- DOI: http://doi.org/10.3803/EnM.2017.32.4.466
Abstract
- BACKGROUND
Primary adrenal insufficiency (PAI) is a rare, potentially life-threatening condition. There are few Korean studies on PAI, and most have had small sample sizes. We aimed to examine the etiology, clinical characteristics, treatment, and mortality of PAI in Korean patients.
METHODS
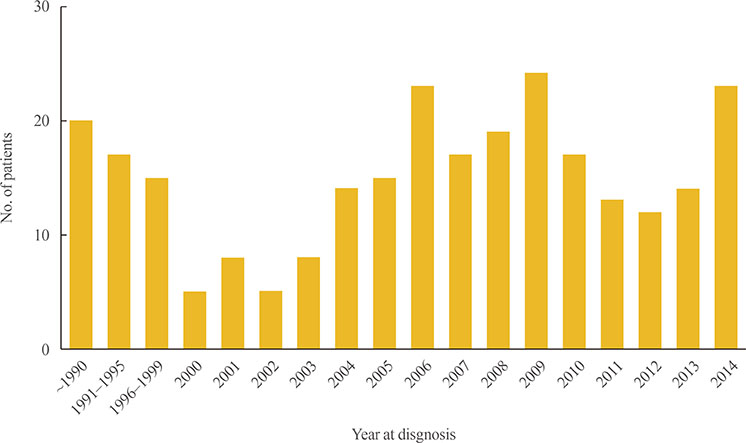
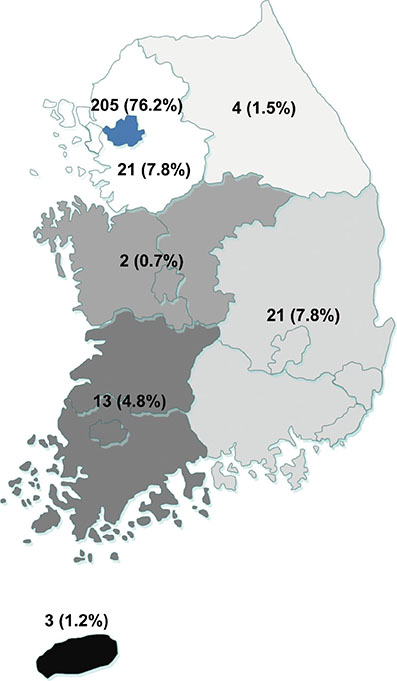
A nationwide, multicenter, registry-based survey was conducted to identify adults diagnosed with or treated for PAI at 30 secondary or tertiary care institutions in Korea between 2000 and 2014.
RESULTS
A total of 269 patients with PAI were identified. The prevalence of PAI was 4.17 per million. The estimated incidence was 0.45 per million per year. The mean age at diagnosis was 49.0 years, and PAI was more prevalent in men. Adrenal tuberculosis was the most common cause of PAI in patients diagnosed before 2000; for those diagnosed thereafter, adrenal metastasis and tuberculosis were comparable leading causes. The etiology of PAI was not identified in 34.9% of cases. Of the patients receiving glucocorticoid replacement therapy, prednisolone was more frequently administered than hydrocortisone (69.4% vs. 26.5%, respectively), and only 27.1% of all patients received fludrocortisone. We observed an increased prevalence of metabolic disease and osteoporosis during the follow-up period (median, 60.2 months). The observed overall mortality and disease-specific mortality rates were 11.9% and 3.1%, respectively.
CONCLUSION
The prevalence of PAI is significantly lower in Koreans than in reports from Western countries. The high frequency undetermined etiology in patients with PAI suggests the need to reveal accurate etiology of PAI in Korea.
MeSH Terms
-
Addison Disease*
Adult
Autoimmune Diseases
Diagnosis
Fludrocortisone
Follow-Up Studies
Glucocorticoids
Humans
Hydrocortisone
Incidence
Korea*
Male
Metabolic Diseases
Mortality
Neoplasm Metastasis
Osteoporosis
Prednisolone
Prevalence
Sample Size
Tertiary Healthcare
Tuberculosis
Fludrocortisone
Glucocorticoids
Hydrocortisone
Prednisolone
Figure
Cited by 2 articles
-
Encountering COVID-19 as Endocrinologists
Eun-Jung Rhee, Jung Hee Kim, Sun Joon Moon, Won-Young Lee
Endocrinol Metab. 2020;35(2):197-205. doi: 10.3803/EnM.2020.35.2.197.Novel
ABCD1 Gene Mutation in a Korean Patient with X-Linked Adrenoleukodystrophy Presenting with Addison's Disease
Yun Kyung Cho, Seo-Young Lee, Sang-Wook Kim
Endocrinol Metab. 2020;35(1):188-191. doi: 10.3803/EnM.2020.35.1.188.
Reference
-
1. Bornstein SR, Allolio B, Arlt W, Barthel A, Don-Wauchope A, Hammer GD, et al. Diagnosis and treatment of primary adrenal insufficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016; 101:364–389.2. Bensing S, Hulting AL, Husebye ES, Kampe O, Lovas K. Management of endocrine disease: epidemiology, quality of life and complications of primary adrenal insufficiency. A review. Eur J Endocrinol. 2016; 175:R107–R116.3. Erichsen MM, Lovas K, Fougner KJ, Svartberg J, Hauge ER, Bollerslev J, et al. Normal overall mortality rate in Addison's disease, but young patients are at risk of premature death. Eur J Endocrinol. 2009; 160:233–237.4. Wallace I, Cunningham S, Lindsay J. The diagnosis and investigation of adrenal insufficiency in adults. Ann Clin Biochem. 2009; 46(Pt 5):351–367.5. Chakera AJ, Vaidya B. Addison disease in adults: diagnosis and management. Am J Med. 2010; 123:409–413.6. Laureti S, Vecchi L, Santeusanio F, Falorni A. Is the prevalence of Addison's disease underestimated? J Clin Endocrinol Metab. 1999; 84:1762.7. Olafsson AS, Sigurjonsdottir HA. Increasing prevalence of Addison disease: results from a nationwide study. Endocr Pract. 2016; 22:30–35.8. Nomura K, Demura H, Saruta T. Addison's disease in Japan: characteristics and changes revealed in a nationwide survey. Intern Med. 1994; 33:602–606.9. Mazziotti G, Formenti AM, Frara S, Roca E, Mortini P, Berruti A, et al. Management of endocrine disease: risk of overtreatment in patients with adrenal insufficiency. Current and emerging aspects. Eur J Endocrinol. 2017; 177:R231–R248.10. Lee KS, Chung YS, Park KH, Kim HS, Kim HM. A case of primary bilateral adrenal lymphoma with partial adrenal insufficiency. Yonsei Med J. 1999; 40:297–300.11. Park HD, Park SJ, Choi YM, Kang JH. Adrenomyeloneuropathy presenting with adrenal insufficiency. Ann Rehabil Med. 2013; 37:563–566.12. Lee YW, Won JC, Ki CS, Lee HY, Ahn HS, Lee YK, et al. Clinical and genetic analysis of a Korean patient with late-onset X-linked adrenal hypoplasia congenita and hypogonadotropic hypogonadism: identification of a novel mutation in the NR0B1 gene. J Int Med Res. 2008; 36:357–361.13. Sung SK, Kwon YJ, Lee BW, Kim DM, Yoo HJ. Clinical review of 20 cases of Addison's disease in Korea: including previously reported cases and 6 new cases at the National Medical Center. Korean J Intern Med. 1988; 3:72–76.14. Meyer G, Neumann K, Badenhoop K, Linder R. Increasing prevalence of Addison's disease in German females: health insurance data 2008-2012. Eur J Endocrinol. 2014; 170:367–373.15. Mason AS, Meade TW, Lee JA, Morris JN. Epidemiological and clinical picture of Addison's disease. Lancet. 1968; 2:744–747.16. Nerup J. Addison's disease: clinical studies. A report of 108 cases. Acta Endocrinol (Copenh). 1974; 76:127–141.17. Bjornsdottir S, Sundstrom A, Ludvigsson JF, Blomqvist P, Kampe O, Bensing S. Drug prescription patterns in patients with Addison's disease: a Swedish population-based cohort study. J Clin Endocrinol Metab. 2013; 98:2009–2018.18. Lovas K, Husebye ES. High prevalence and increasing incidence of Addison's disease in western Norway. Clin Endocrinol (Oxf). 2002; 56:787–791.19. Reato G, Morlin L, Chen S, Furmaniak J, Smith BR, Masiero S, et al. Premature ovarian failure in patients with autoimmune Addison's disease: clinical, genetic, and immunological evaluation. J Clin Endocrinol Metab. 2011; 96:E1255–E1261.20. Fichna M, Fichna P, Gryczynska M, Walkowiak J, Zurawek M, Sowinski J. Screening for associated autoimmune disorders in Polish patients with Addison's disease. Endocrine. 2010; 37:349–360.21. Betterle C, Scarpa R, Garelli S, Morlin L, Lazzarotto F, Presotto F, et al. Addison's disease: a survey on 633 patients in Padova. Eur J Endocrinol. 2013; 169:773–784.22. Park SM, Joung JY, Cho YY, Sohn SY, Hur KY, Kim JH, et al. Effect of high dietary sodium on bone turnover markers and urinary calcium excretion in Korean postmenopausal women with low bone mass. Eur J Clin Nutr. 2015; 69:361–366.23. Kwon SJ, Ha YC, Park Y. High dietary sodium intake is associated with low bone mass in postmenopausal women: Korea National Health and Nutrition Examination Survey, 2008-2011. Osteoporos Int. 2017; 28:1445–1452.24. Johannsson G, Filipsson H, Bergthorsdottir R, Lennernas H, Skrtic S. Long-acting hydrocortisone for glucocorticoid replacement therapy. Horm Res. 2007; 68:Suppl 5. 182–188.25. Margulies PL, Mullen J. North American survey of individuals with Addison's disease (1997) [Internet]. Great Neck: National Adrenal Diseases Foundation;c1987. cited 2017 Oct 26. Available from: http://www.nadf.us/contact-nadf/.26. Lovas K, Gjesdal CG, Christensen M, Wolff AB, Almas B, Svartberg J, et al. Glucocorticoid replacement therapy and pharmacogenetics in Addison's disease: effects on bone. Eur J Endocrinol. 2009; 160:993–1002.27. Giordano R, Marzotti S, Balbo M, Romagnoli S, Marinazzo E, Berardelli R, et al. Metabolic and cardiovascular profile in patients with Addison's disease under conventional glucocorticoid replacement. J Endocrinol Invest. 2009; 32:917–923.28. Lovas K, Loge JH, Husebye ES. Subjective health status in Norwegian patients with Addison's disease. Clin Endocrinol (Oxf). 2002; 56:581–588.29. Gurnell EM, Hunt PJ, Curran SE, Conway CL, Pullenayegum EM, Huppert FA, et al. Long-term DHEA replacement in primary adrenal insufficiency: a randomized, controlled trial. J Clin Endocrinol Metab. 2008; 93:400–409.30. Kluger N, Matikainen N, Sintonen H, Ranki A, Roine RP, Schalin-Jantti C. Impaired health-related quality of life in Addison's disease: impact of replacement therapy, comorbidities and socio-economic factors. Clin Endocrinol (Oxf). 2014; 81:511–518.31. Bergthorsdottir R, Leonsson-Zachrisson M, Oden A, Johannsson G. Premature mortality in patients with Addison's disease: a population-based study. J Clin Endocrinol Metab. 2006; 91:4849–4853.32. Bensing S, Brandt L, Tabaroj F, Sjoberg O, Nilsson B, Ekbom A, et al. Increased death risk and altered cancer incidence pattern in patients with isolated or combined autoimmune primary adrenocortical insufficiency. Clin Endocrinol (Oxf). 2008; 69:697–704.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adrenal Tuberculosis Mimicking a Malignant Tumor with Primary Adrenal Insufficiency
- A Case of Primary Adrenal Insufficiency Presenting as the Initial Clinical Manifestation of Primary Antiphospholipid Antibody Syndrome
- A case of primary bilateral adrenal lymphoma with partial adrenal insufficiency
- A case of Addison's disease due to tuberculosis: pathologic confirmation by laparoscopic biopsy
- Diverse etiologies, diagnostic approach, and management of primary adrenal insufficiency in pediatric age