Anesth Pain Med.
2017 Oct;12(4):342-347. 10.17085/apm.2017.12.4.342.
Hemodynamic response to tracheal intubation and postoperative pharyngeal morbidity using GlideScope®, Lightwand and Macintosh laryngoscopes during remifentanil infusion
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. khlee6006@yonsei.ac.kr
- KMID: 2405852
- DOI: http://doi.org/10.17085/apm.2017.12.4.342
Abstract
- BACKGROUND
Use of GlideScope® laryngoscopes and lightwands for tracheal intubation does not require much force. Theoretically, less stimulation can reduce hemodynamic changes during intubation. We investigated the hemodynamic response to tracheal intubation using different laryngoscope types during remifentanil infusion.
METHODS
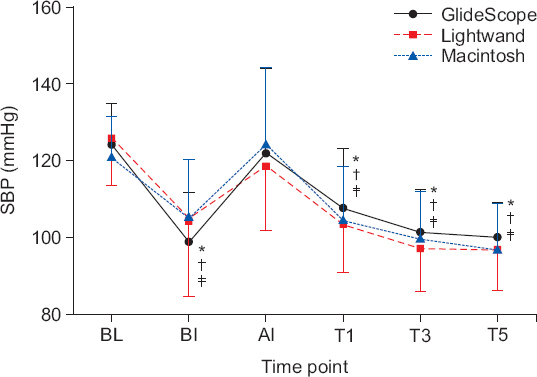
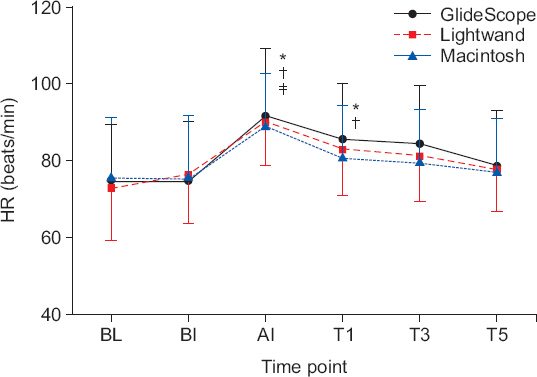
Sixty American Society of Anesthesiologists class I-II patients were compared in terms of tracheal intubation time, hemodynamic changes, and postoperative pharyngeal complications when using a GlideScope®, lightwand, or Macintosh laryngoscope. Propofol and rocuronium were injected and remifentanil was infused for three minutes. Blood pressure and heart rate were measured before and 1, 3, and 5 minutes after tracheal intubation. Patients were assessed for postoperative oral and tracheal bleeding as well as hoarseness, dysphagia, and sore throat.
RESULTS
Intubation time was prolonged in the GlideScope® group. All three groups showed a significant decrease in systolic and diastolic blood pressure 1, 3, and 5 minutesafter tracheal intubation. Heart rates increased significantly in all three groups immediately after intubation as well as 1 minute later in the GlideScope® group. However, there were no differences in blood pressure, heart rate, or the occurrence of hoarseness, dysphagia, and sore throat among the three groups.
CONCLUSIONS
No differences in hemodynamic change were found among the three different techniques.
Keyword
MeSH Terms
Figure
Reference
-
1. Prys-Roberts C, Greene LT, Meloche R, Foëx P. Studies of anaesthesia in relation to hypertension. II. Haemodynamic consequences of induction and endotracheal intubation. Br J Anaesth. 1971; 43:531–47. DOI: 10.1093/bja/43.6.531. PMID: 5089931.2. Martin DE, Rosenberg H, Aukburg SJ, Bartkowski RR, Edwards MW Jr, Greenhow DE, et al. Low-dose fentanyl blunts circulatory responses to tracheal intubation. Anesth Analg. 1982; 61:680–4. DOI: 10.1213/00000539-198208000-00011. PMID: 7201271.3. Nishikawa T, Namiki A. Attenuation of the pressor response to laryngoscopy and tracheal intubation with intravenous verapamil. Acta Anaesthesiol Scand. 1989; 33:232–5. DOI: 10.1111/j.1399-6576.1989.tb02896.x. PMID: 2728827.4. Oh YS, Han SH, Lee YS, Huh J. Arterial blood pressure and heart rate response to lightwand or direct laryngoscopy for endotracheal intubation. Korean J Anesthesiol. 1997; 33:858–63. DOI: 10.4097/kjae.1997.33.5.858.5. Forbes AM, Dally FG. Acute hypertension during induction of anaesthesia and endotracheal intubation in normotensive man. Br J Anaesth. 1970; 42:618–24. DOI: 10.1093/bja/42.7.618.6. Omote K, Kirita A, Namiki A, Iwasaki H. Effects of nicardipine on the circulatory responses to tracheal intubation in normotensive and hypertensive patients. Anaesthesia. 1992; 47:24–7. DOI: 10.1111/j.1365-2044.1992.tb01947.x. PMID: 1536397.7. Loh KS, Irish JC. Traumatic complications of intubation and other airway management procedures. Anesthesiol Clin North America. 2002; 20:953–69. DOI: 10.1016/S0889-8537(02)00022-6.8. Maruyama K, Nakagawa H, Imanishi H, Kitamura A, Hayashida M. Comparison of postoperative pharyngeal morbidity using the Macintosh laryngoscope or AirWay Scope after mastectomy. J Anesth. 2011; 25:773–6. DOI: 10.1007/s00540-011-1195-3. PMID: 21728080.9. Hung OR, Pytka S, Morris I, Murphy M, Launcelott G, Stevens S, et al. Clinical trial of a new lightwand device (Trachlight) to intubate the trachea. Anesthesiology. 1995; 83:509–14. DOI: 10.1097/00000542-199509000-00009. PMID: 7661351.10. Hung OR, Pytka S, Morris I, Murphy M, Stewart RD. Lightwand intubation:II--Clinical trial of a new lightwand for tracheal intubation in patients with difficult airways. Can J Anaesth. 1995; 42:826–30. DOI: 10.1007/BF03011187. PMID: 7497568.11. Friedman PG, Rosenberg MK, Lebenbom-Mansour M. A comparison of light wand and suspension laryngoscopic intubation techniques in outpatients. Anesth Analg. 1997; 85:578–82. DOI: 10.1213/00000539-199709000-00017. PMID: 9296412.12. Koyama Y, Nishihama M, Inagawa G, Kamiya Y, Miki T, Kurihara R, et al. Comparison of haemodynamic responses to tracheal intubation using the Airway Scope(®) and Macintosh laryngoscope in normotensive and hypertensive patients. Anaesthesia. 2011; 66:895–900. DOI: 10.1111/j.1365-2044.2011.06802.x. PMID: 21770906.13. Yoon C, Park KS, Park SY, Chae YJ, Min SK, Lee SY, et al. Hemodynamic changes after endotracheal intubation in patients with cerebral aneurysm. Anesth Pain Med. 2008; 3:49–54.14. Nishikawa K, Omote K, Kawana S, Namiki A. A comparison of hemodynamic changes after endotracheal intubation by using the lightwand device and the laryngoscope in normotensive and hypertensive patients. Anesth Analg. 2000; 90:1203–7. DOI: 10.1097/00000539-200005000-00038. PMID: 10781480.15. Hirabayashi Y, Hiruta M, Kawakami T, Inoue S, Fukuda H, Saitoh K, et al. Effects of lightwand (Trachlight) compared with direct laryngoscopy on circulatory responses to tracheal intubation. Br J Anaesth. 1998; 81:253–5. DOI: 10.1093/bja/81.2.253. PMID: 9813535.16. Teoh WH, Saxena S, Shah MK, Sia AT. Comparison of three videolaryngoscopes:Pentax Airway Scope, C-MAC, Glidescope vs the Macintosh laryngoscope for tracheal intubation. Anaesthesia. 2010; 65:1126–32. DOI: 10.1111/j.1365-2044.2010.06513.x. PMID: 20883502.17. Lim TJ, Lim Y, Liu EH. Evaluation of ease of intubation with the GlideScope or Macintosh laryngoscope by anaesthetists in simulated easy and difficult laryngoscopy. Anaesthesia. 2005; 60:180–3. DOI: 10.1111/j.1365-2044.2004.04038.x. PMID: 15644017.18. Dahlgren N, Messeter K. Treatment of stress response to laryngoscopy and intubation with fentanyl. Anaesthesia. 1981; 36:1022–6. DOI: 10.1111/j.1365-2044.1981.tb08676.x. PMID: 7032347.19. Ko SH, Kim DC, Han YJ, Song HS. Small-dose fentanyl:optimal time of injection for blunting the circulatory responses to tracheal intubation. Anesth Analg. 1998; 86:658–61. DOI: 10.1213/00000539-199803000-00041.20. Choi YJ, Shin HW, Kim YH, Choi SU, Park JY, Yoon SZ, et al. Effect of remifentanil or esmolol on bispectral index and entropy to tracheal intubation during propofol anesthesia. Anesth Pain Med. 2010; 5:304–9.21. Kim JS, Kim DH, Joe HB, Oh CK, Kim JY. Effect of tracheal lidocaine on intubating conditions during propofol-remifentanil target-controlled infusion without neuromuscular blockade in day-case anesthesia. Korean J Anesthesiol. 2013; 65:425–30. DOI: 10.4097/kjae.2013.65.5.425. PMID: 24363845. PMCID: PMC3866338.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of effect-site concentration of remifentanil for tracheal intubation with the lightwand and laryngoscopy during propofol target-controlled infusion
- The effect of tracheal intubation with the McCoy or Macintosh laryngoscope on the blood pressure and heart rate during propofol-remifentanil induction
- Hemodynamic Changes after Endotracheal Intubation in Patients with Cerebral Aneurysm
- Comparison of the Cervical Spine Motion during Endotracheal Intubation with Lightwands and Macintosh Laryngoscopes
- Effect-site concentration of remifentanil for blunting hemodynamic responses to tracheal intubation using light wand during target controlled infusion-total intravenous anesthesia