Ann Surg Treat Res.
2018 Mar;94(3):135-141. 10.4174/astr.2018.94.3.135.
The optimal surgical resection approach for T2 gallbladder carcinoma: evaluating the role of surgical extent according to the tumor location
- Affiliations
-
- 1Department of Surgery, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea. kjkang@dsmc.or.kr
- 2Department of Surgery, Andong Medical Group Hospital, Andong, Korea.
- 3Department of Radiology, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
- KMID: 2405325
- DOI: http://doi.org/10.4174/astr.2018.94.3.135
Abstract
- PURPOSE
The clinical behavior of T2 gallbladder cancer varies among patients. The aims of this study were to identify prognostic factors for survival and recurrence, and to determine the optimal surgical strategy for T2 gallbladder cancer.
METHODS
We conducted a retrospective analysis of 78 patients with T2 gallbladder cancer who underwent surgical resection for gallbladder cancer.
RESULTS
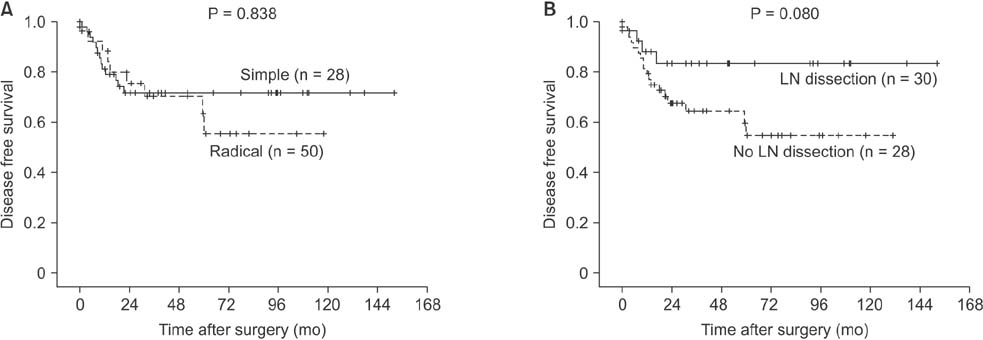
Twenty-eight patients (35.9%) underwent simple cholecystectomy and 50 (64.1%) underwent extended cholecystectomy. Among 56 patients without LN metastasis (n = 20) or unknown LN status (no LN dissection, n = 36), the 5-year disease-free survival rates were 81.6%, and 69.8% (P = 0.080). In an analysis according to tumor location, patients with tumors located on the hepatic side (n = 36) had a higher recurrence rate than patients with tumors located on the peritoneal side only (n = 35) (P = 0.043). On multivariate analysis, R1 resection and lymph node metastasis were significant, independent prognostic factors for poor disease-free and overall survival.
CONCLUSION
R0 resection and LN dissection are an appropriate curative surgical strategy in patients with T2 gallbladder cancer. Tumors located on the hepatic side show worse prognosis than tumors located on the peritoneal side only, hepatic resection should be considered.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Laparoscopic radical cholecystectomy with common bile duct resection for T2 gallbladder cancer
Jonathan Geograpo Navarro, Chang Moo Kang
Ann Hepatobiliary Pancreat Surg. 2019;23(1):69-73. doi: 10.14701/ahbps.2019.23.1.69.
Reference
-
1. Yamaguchi K, Chijiiwa K, Saiki S, Nishihara K, Takashima M, Kawakami K, et al. Retrospective analysis of 70 operations for gallbladder carcinoma. Br J Surg. 1997; 84:200–204.
Article2. Ogura Y, Mizumoto R, Isaji S, Kusuda T, Matsuda S, Tabata M. Radical operations for carcinoma of the gallbladder: present status in Japan. World J Surg. 1991; 15:337–343.
Article3. Kang CM, Lee WJ, Choi GH, Kim JY, Kim KS, Choi JS, et al. Does “clinical” R0 have validity in the choice of simple cholecystectomy for gallbladder carcinoma? J Gastrointest Surg. 2007; 11:1309–1316.
Article4. Kohya N, Miyazaki K. Hepatectomy of segment 4a and 5 combined with extrahepatic bile duct resection for T2 and T3 gallbladder carcinoma. J Surg Oncol. 2008; 97:498–502.
Article5. Shirai Y, Yoshida K, Tsukada K, Muto T. Inapparent carcinoma of the gallbladder. An appraisal of a radical second operation after simple cholecystectomy. Ann Surg. 1992; 215:326–331.6. Lee SE, Jang JY, Lim CS, Kang MJ, Kim SW. Systematic review on the surgical treatment for T1 gallbladder cancer. World J Gastroenterol. 2011; 17:174–180.
Article7. Miyakawa S, Ishihara S, Horiguchi A, Takada T, Miyazaki M, Nagakawa T. Biliary tract cancer treatment: 5,584 results from the Biliary Tract Cancer Statistics Registry from 1998 to 2004 in Japan. J Hepatobiliary Pancreat Surg. 2009; 16:1–7.
Article8. Chan SY, Poon RT, Lo CM, Ng KK, Fan ST. Management of carcinoma of the gallbladder: a single-institution experience in 16 years. J Surg Oncol. 2008; 97:156–164.
Article9. Sikora SS, Singh RK. Surgical strategies in patients with gallbladder cancer: nihilism to optimism. J Surg Oncol. 2006; 93:670–681.
Article10. Choi SB, Han HJ, Kim CY, Kim WB, Song TJ, Suh SO, et al. Surgical outcomes and prognostic factors for T2 gallbladder cancer following surgical resection. J Gastrointest Surg. 2010; 14:668–678.
Article11. Suzuki S, Yokoi Y, Kurachi K, Inaba K, Ota S, Azuma M, et al. Appraisal of surgical treatment for pT2 gallbladder carcinomas. World J Surg. 2004; 28:160–165.
Article12. Chijiiwa K, Noshiro H, Nakano K, Okido M, Sugitani A, Yamaguchi K, et al. Role of surgery for gallbladder carcinoma with special reference to lymph node metastasis and stage using western and Japanese classification systems. World J Surg. 2000; 24:1271–1276.
Article13. Wakai T, Shirai Y, Yokoyama N, Ajioka Y, Watanabe H, Hatakeyama K. Depth of subserosal invasion predicts long-term survival after resection in patients with T2 gallbladder carcinoma. Ann Surg Oncol. 2003; 10:447–454.
Article14. Chijiiwa K, Nakano K, Ueda J, Noshiro H, Nagai E, Yamaguchi K, et al. Surgical treatment of patients with T2 gallbladder carcinoma invading the subserosal layer. J Am Coll Surg. 2001; 192:600–607.
Article15. Benoist S, Panis Y, Fagniez PL. Long-term results after curative resection for carcinoma of the gallbladder. French University Association for Surgical Research. Am J Surg. 1998; 175:118–122.16. Mayo SC, Shore AD, Nathan H, Edil B, Wolfgang CL, Hirose K, et al. National trends in the management and survival of surgically managed gallbladder adenocarcinoma over 15 years: a population-based analysis. J Gastrointest Surg. 2010; 14:1578–1591.17. Kim DH, Kim SH, Choi GH, Kang CM, Kim KS, Choi JS, et al. Role of cholecystectomy and lymph node dissection in patients with T2 gallbladder cancer. World J Surg. 2013; 37:2635–2640.
Article18. Shimada H, Endo I, Togo S, Nakano A, Izumi T, Nakagawara G. The role of lymph node dissection in the treatment of gallbladder carcinoma. Cancer. 1997; 79:892–899.
Article19. Isambert M, Leux C, Métairie S, Paineau J. Incidentally-discovered gallbladder cancer: When, why and which reoperation? J Visc Surg. 2011; 148:e77–e84.
Article20. Goetze TO, Paolucci V. Benefits of reoperation of T2 and more advanced incidental gallbladder carcinoma: analysis of the German registry. Ann Surg. 2008; 247:104–108.21. Yokomizo H, Yamane T, Hirata T, Hifumi M, Kawaguchi T, Fukuda S. Surgical treatment of pT2 gallbladder carcinoma: a reevaluation of the therapeutic effect of hepatectomy and extrahepatic bile duct resection based on the long-term outcome. Ann Surg Oncol. 2007; 14:1366–1373.
Article22. Shindoh J, de Aretxabala X, Aloia TA, Roa JC, Roa I, Zimmitti G, et al. Tumor location is a strong predictor of tumor progression and survival in T2 gallbladder cancer: an international multicenter study. Ann Surg. 2015; 261:733–739.23. Lee H, Choi DW, Park JY, Youn S, Kwon W, Heo JS, et al. Surgical strategy for T2 gallbladder cancer according to tumor location. Ann Surg Oncol. 2015; 22:2779–2786.
Article24. Endo I, Shimada H, Takimoto A, Fujii Y, Miura Y, Sugita M, et al. Microscopic liver metastasis: prognostic factor for patients with pT2 gallbladder carcinoma. World J Surg. 2004; 28:692–696.
Article25. Yoshimitsu K, Honda H, Kaneko K, Kuroiwa T, Irie H, Chijiiwa K, et al. Anatomy and clinical importance of cholecystic venous drainage: helical CT observations during injection of contrast medium into the cholecystic artery. AJR Am J Roentgenol. 1997; 169:505–510.
Article26. Fahim RB, McDonald JR, Richards JC, Ferris DO. Carcinoma of the gallbladder: a study of its modes of spread. Ann Surg. 1962; 156:114–124.27. Sons HU, Borchard F, Joel BS. Carcinoma of the gallbladder: autopsy findings in 287 cases and review of the literature. J Surg Oncol. 1985; 28:199–206.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Surgical Methods and Tumor Location on Survival and Recurrence Patterns after Curative Resection in Patients with T2 Gallbladder Cancer
- Extent of Surgical Resection in Gallbladder Cancer
- Supramaximal Resection for Glioblastoma: Redefining the Extent of Resection Criteria and Its Impact on Survival
- The Survival Rate of Gallbladder Carcinoma Based on the presence of Lymph Node Metastasis and the Depth of the Primary Tumor Invasion
- Surgical Outcome and Prognostic Factors of Primary Gallbladder Carcinoma