J Korean Ophthalmol Soc.
2008 Dec;49(12):2006-2010.
A Case of Conjunctival Autotransplantation Using Conjunctival Flap of Pterygium in Treating Corneal Ulcer Perforation
- Affiliations
-
- 1Department of Ophthalmology, Wallace Memorial Baptist Hospital, Pusan, Korea. oph@wmbh.co.kr
Abstract
-
PURPOSE: To report a case of conjunctival autotransplantation using the conjunctival flap of the pterygium for thetreatment corneal ulcer perforation.
CASE SUMMARY
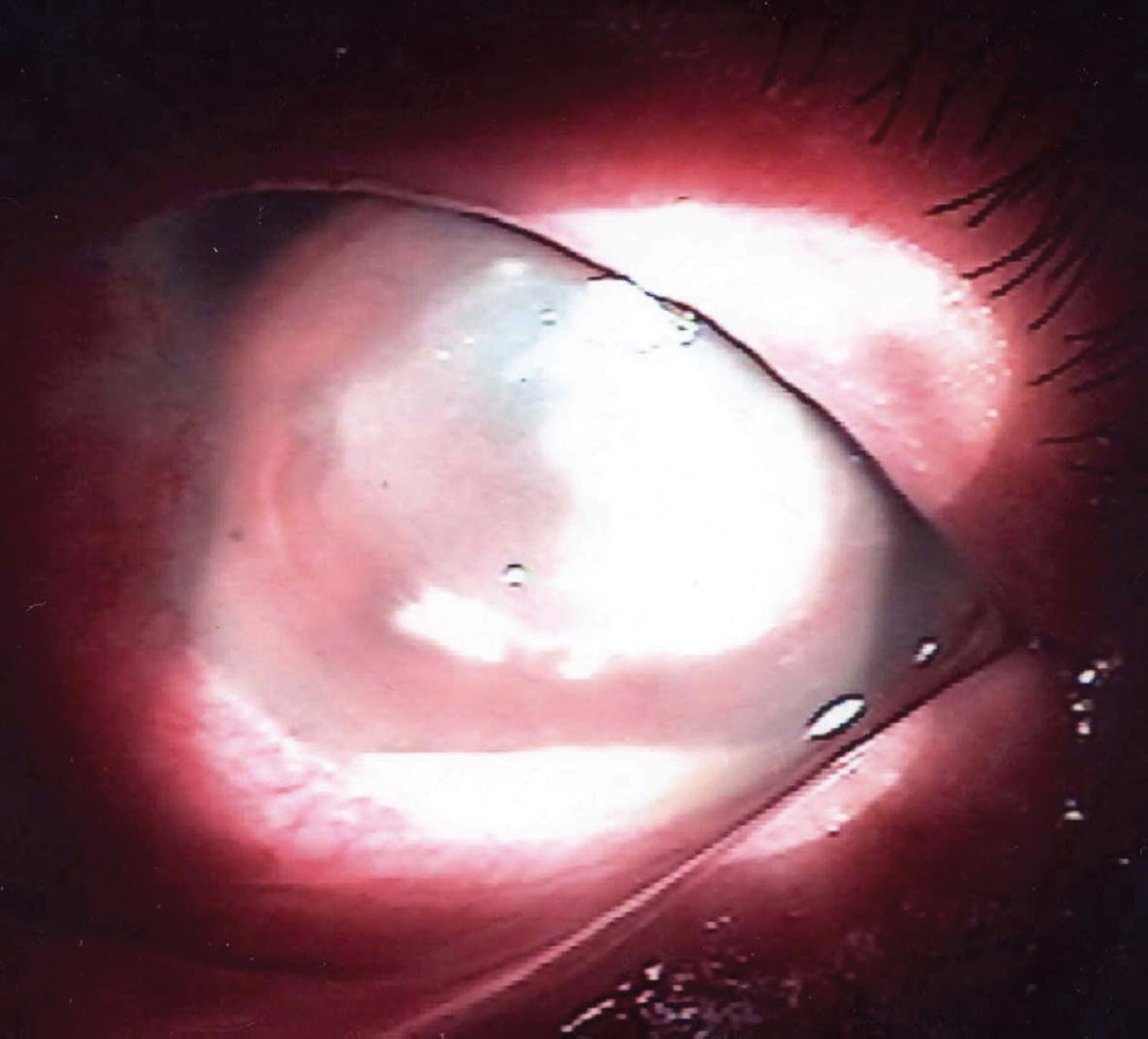
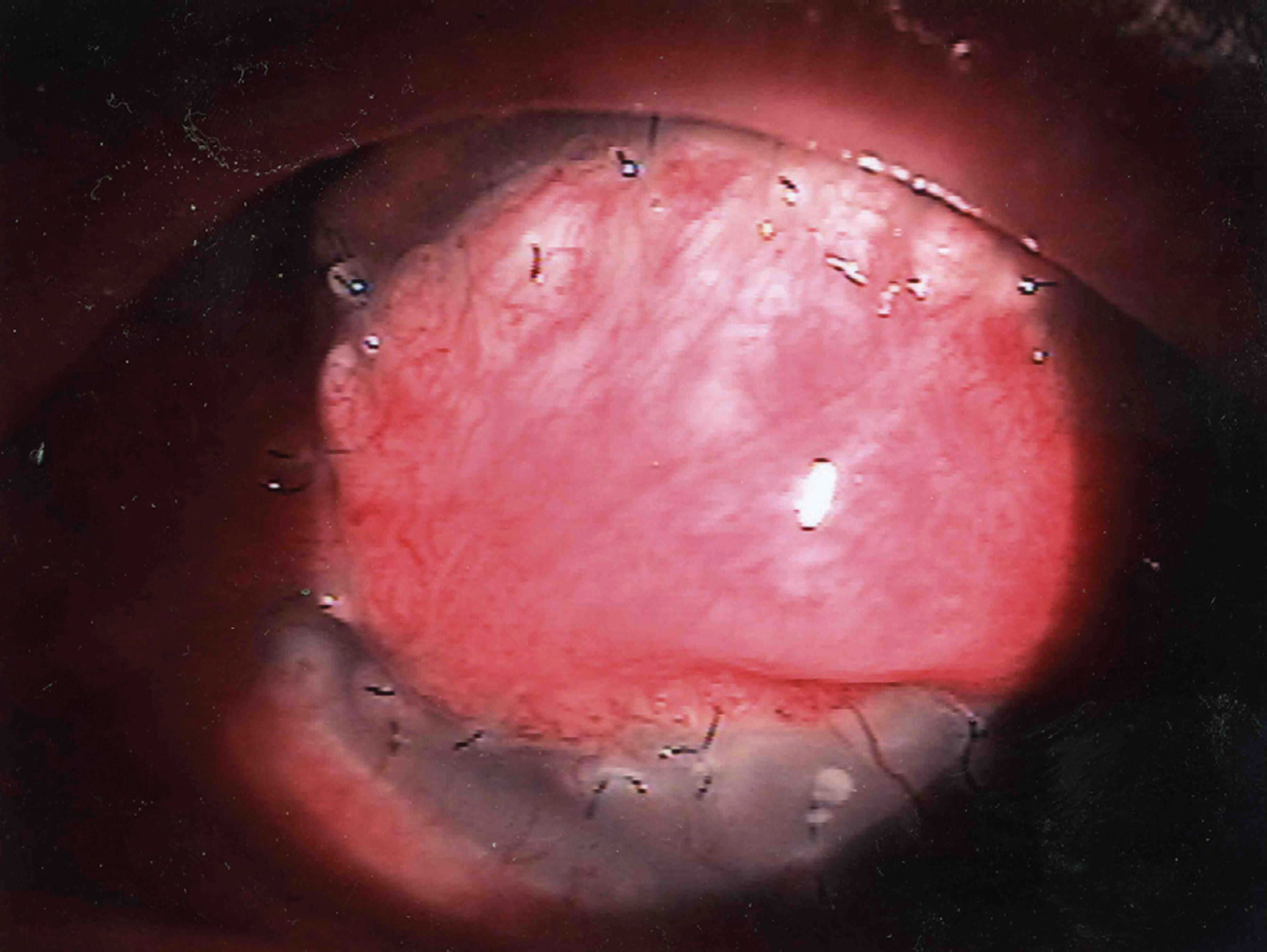
A 72-year-old woman was referred to our hospital because her left eye had a corneal ulcer due topine needle trauma, and she did not respond to the initial therapy in a private clinic for 1 week. We first applied topical and systemic antibiotics. However, the lesion did not subside, and necrosis progressed in the stroma at the center of the cornea. On day 6 of admission, perforation was found at the center of the cornea, and we excised the necrotic tissue and performed bilateral pedicle conjunctival flap transposition. After the operation, an ischemic change was observed, and in the fourth week perforation occured at the center of the transplanted conjunctival flap. Because we considered it difficult to perform the transplantation of a conjunctival flap in the left eye, we performed autotransplantation on the corneal perforation in the left eye using conjunctival flap obtained through a pterygium excision in the right eye. After the operation, vascular ingrowth started from the edge of the flap, and there were no symptoms of inflammation, shrinkage, or necrosis of the flap. During the follow-up observation, the flap survived well without necrosis.
MeSH Terms
Figure
Reference
-
References
1. Hong MA, Rapuano CJ. Management of corneal perforations. Krachmer JH, Holland EJ, editors. Cornea. 1st. St Louis Missouri: Mosby;1997. v. 3. chap. 146.
Article2. Scott LP, Michael SI, Herbert EK. Surgical management of corneal ulceration and perforation. Surv Ophthalmol. 1989; 34:47–58.3. Kenyon KR. Inflammatory mechanism in corneal ulceration. Trans Am Ophthalmol Soc. 1985; 83:610–63.4. Webster RG, Slansky HH, Refojo MF. The use of adhesive for the closure of corneal perforations. Arch Ophthalmol. 1968; 80:705–9.
Article5. Weiss JL, Williams P, Lindstorm RL, Doughman DJ. The use of tissue adhesive in corneal perforations. Ophthalmology. 1983; 90:610–5.
Article6. Dohlman CH, Boruchoff SA, Sullivan GL. A technique for the repair of perforated corneal ulcer. Arch Ophthalmol. 1967; 77:519–25.7. Nobe JR, Moura BT, Robin JB, Smith RE. Resultsof pene- trating keratoplasty for the treatment of corneal perforations. Arch Ophthalmol. 1990; 108:939–41.8. DeRotth A. Plastic repair of conjunctival defects with fetal membrane. Arch Ophthalmol. 1940; 23:522–5.9. Azuara-Blanco A, Pillai CT, Dua HS. Amniotic membrane transplantation for ocular surface reconstruction. Br J Ophthalmol. 1999; 83:399–402.
Article10. Gunderson T. Conjunctival flaps in the treatment of corneal disease with reference to a new technique of application. Arch Ophthalmol. 1958; 60:880–8.11. Larsson S. Treatment of perforated corneal ulcer by autoplastic sclera transplantation. Br J Ophthalmol. 1948; 32:54–7.12. Azuara-Blanco A, Pillai CT, Dua HS. Amniotic membrane- transplantation for ocular surface. Br J Ophthalmol. 1999; 83:399–402.13. Vanathi M, Sharma N, Titiyal JS. . Tectonic grafts for corneal thinning and perforations. Cornea. 2002; 21:792–7.
Article14. Paton D, Milausskas AT. Indications, surgical technique and results of thin conjunctival flaps on the cornea. Int Ophthalmol Clin. 1970; 10:329–45.
Article15. Lee JY, Kim BY, Kim TY. The result of cyanoacrylate glue application for corneal perforation and impending perforation. J Korean Ophthalmol Soc. 2003; 44:2735–41.16. Kim JH, Jeung TB, Kim JC. Amniotic membrane transplan- tation in corneal perforation and impending perforation. J Korean Ophthalmol Soc. 1999; 40:1487–95.17. Portnoy SL, Insler MS, Kaufman HE. Diagnostic and surgical techniques: Surgical management of corneal ulceration and perforation. Surv Ophthalmol. 1989; 34:47–58.18. Hirst LW, Smiddy WE, Stark WJ. Corneal perforations: Changing methods of treatment, 1960-1980. Ophthalmology. 1982; 89:630–5.19. Arensten JJ, Laibson PR, Cohen EJ. Management of corneal descemetoceles and perforations. Ophthalmic Surg. 1985; 16:29–33.20. Lee JH, LEE TW. Study on the pathogens of corneal ulcer. J Korean Ophthalmol Soc. 1981; 22:745–50.21. Shim IC, Oh JS. A clinical observation of bacterial and fungal corneal ulcers. J Korean Ophthalmol Soc. 1982; 23:915–9.22. Lee JH, Jung YC. Pathogens of corneal ulcer (II). J Korean Ophthalmol Soc. 1987; 28:31–6.23. Mannis MJ. Conjunctival flaps. Int Ophthalmol Clin. 1988; 28:165–8.
Article24. Trakis MP, Rogen J, Brown SI. Transplantation of perforated cornea. Am J Ophthalmol. 1974; 78:518–22.25. Coroneo MT, Di Girolamo N, Wakefield D. The pathogenesis of pterygia. Curr Opin Ophthalmol. 1999; 10:282–8.
Article26. Conn H, Berman M, Kenynon K. . Stromal vascularization prevents corneal ulceration. Invest Ophthalmol Vis Sci. 1980; 19:362–70.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Conjunctival Mini-flap Technique and Conjunctival Autotransplantation in Pterygium Surgery
- Recurrence Rates of Conjunctival Autograft Transplantation With Aminiotic Membrane Transplantation in Primary Pterygium Surgery
- The Effect of Inferior Conjunctival Transposition Flap for Recurrent Pterygium
- Factors Affecting Recurrence of Pterygium
- Effect of Inferior Conjunctival Transposition Flap Surgery for Primary Pterygium