J Korean Ophthalmol Soc.
2009 Dec;50(12):1774-1779. 10.3341/jkos.2009.50.12.1774.
Effect of Inferior Conjunctival Transposition Flap Surgery for Primary Pterygium
- Affiliations
-
- 1Department of Ophthalmology, Wonkwang University College of Medicine, Iksan, Korea. sangduck@wonkwang.ac.kr
- KMID: 2212987
- DOI: http://doi.org/10.3341/jkos.2009.50.12.1774
Abstract
- PURPOSE
To evaluate the efficacy and safety of the inferior conjunctival transposition flap for primary pterygium surgery.
METHODS
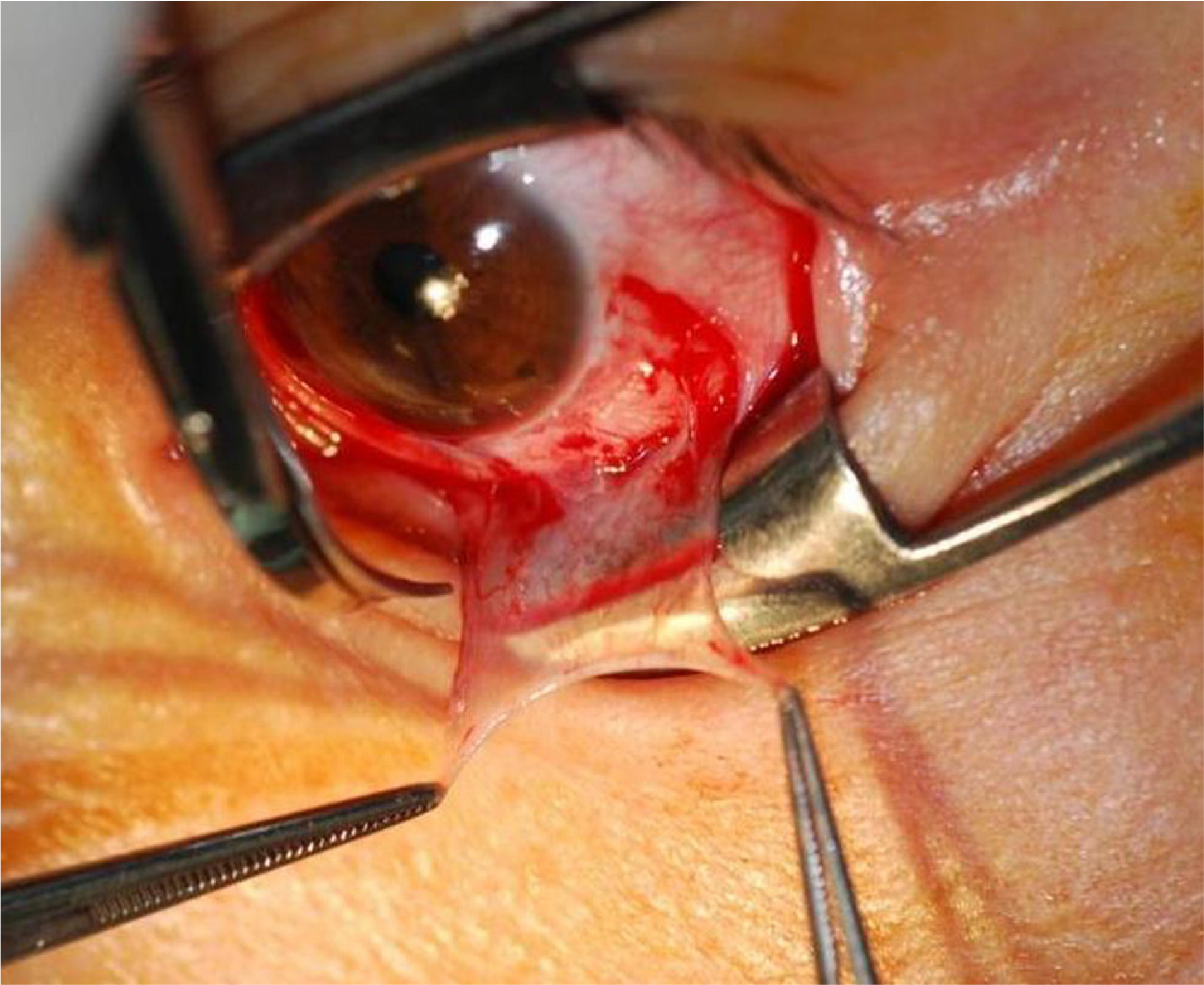
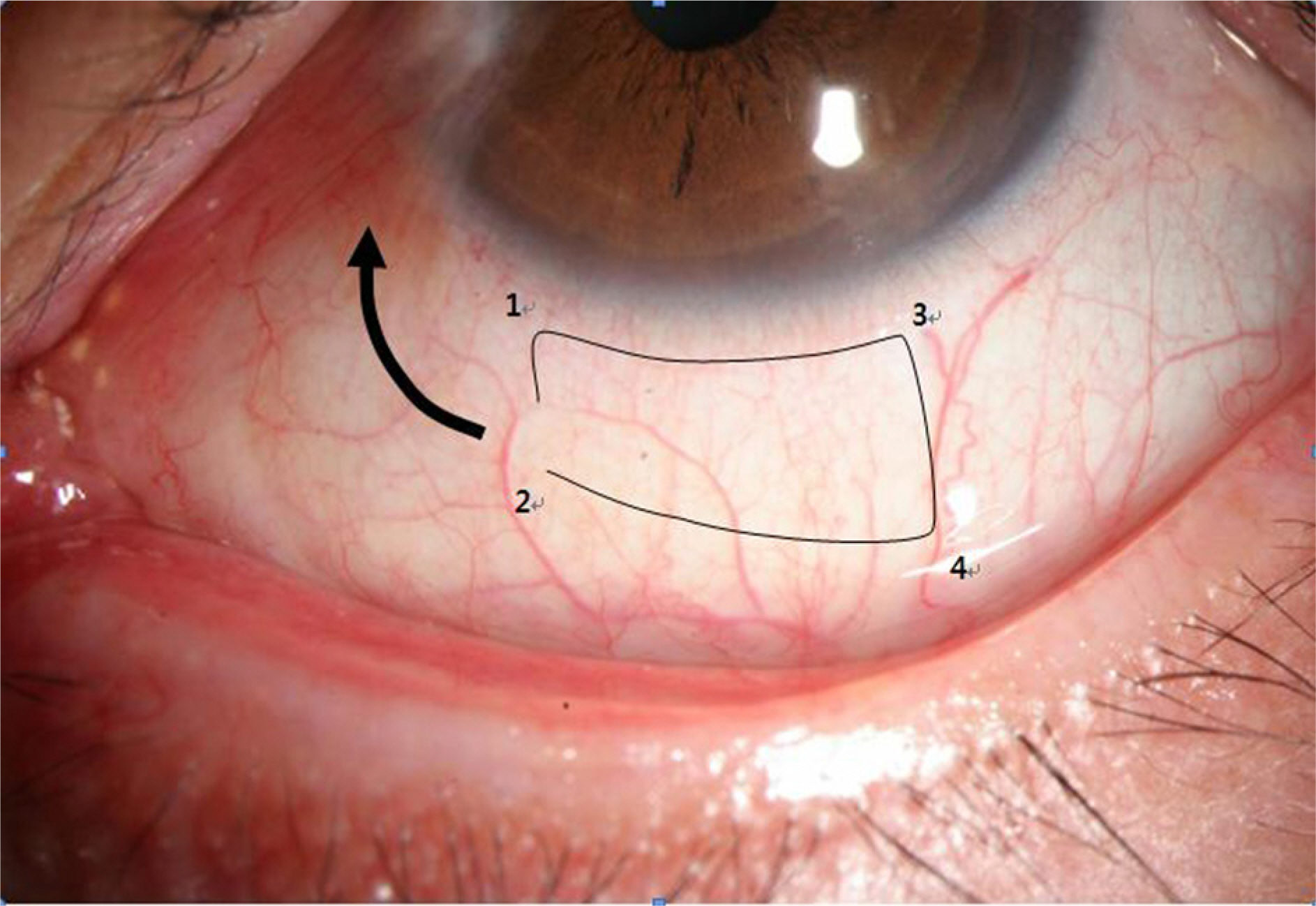
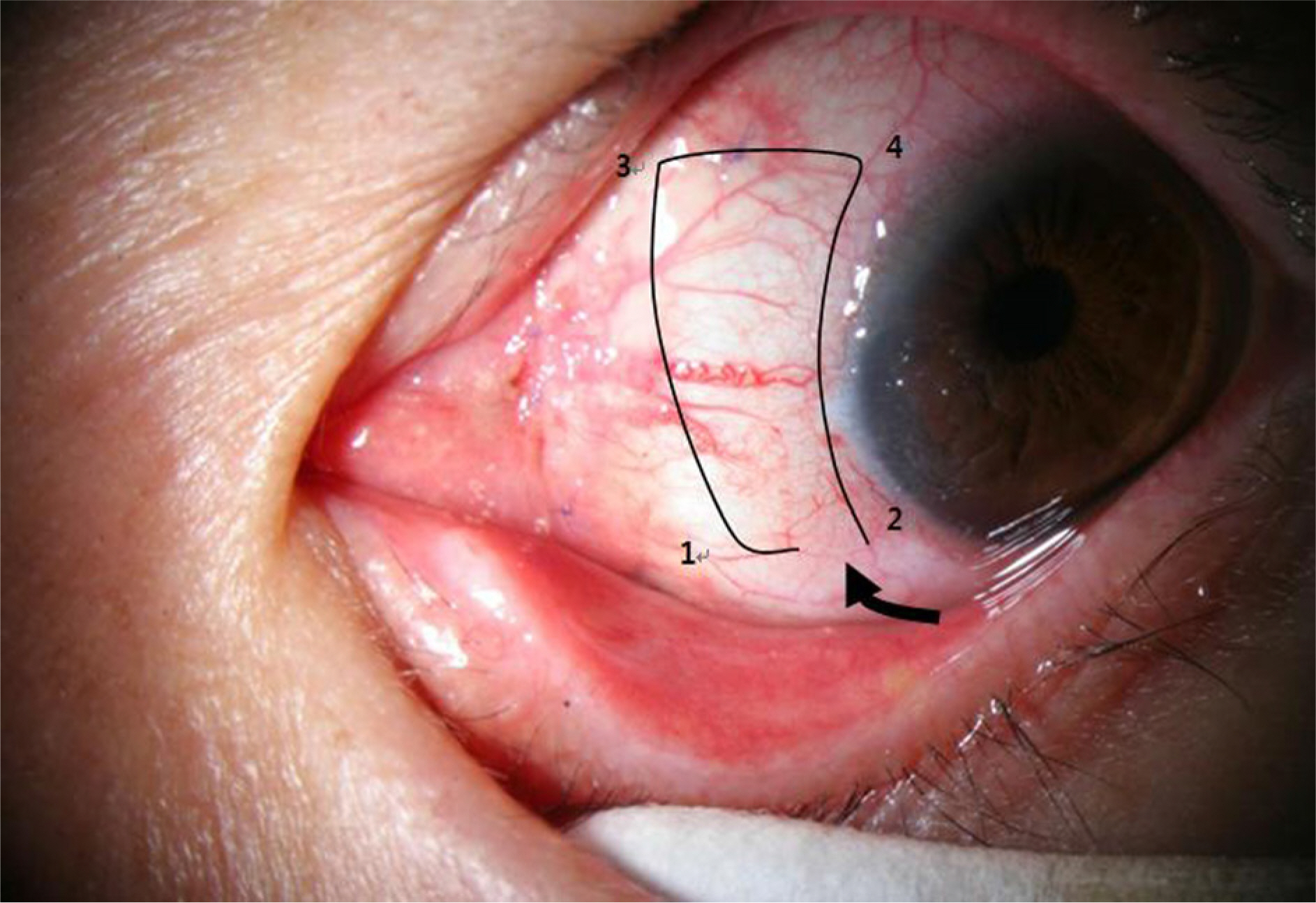
This study reviewed 59 eyes in 59 patients with primary pterygium who were treated with pterygium excision and an inferior conjunctival transposition flap. The inferior conjunctival flap was obtained from lower bulbar conjunctiva and was secured with 8-0 vicryl. Patients were followed-up on the third day after surgery and then at 1, 2, 4 and 12 weeks postoperatively.
RESULTS
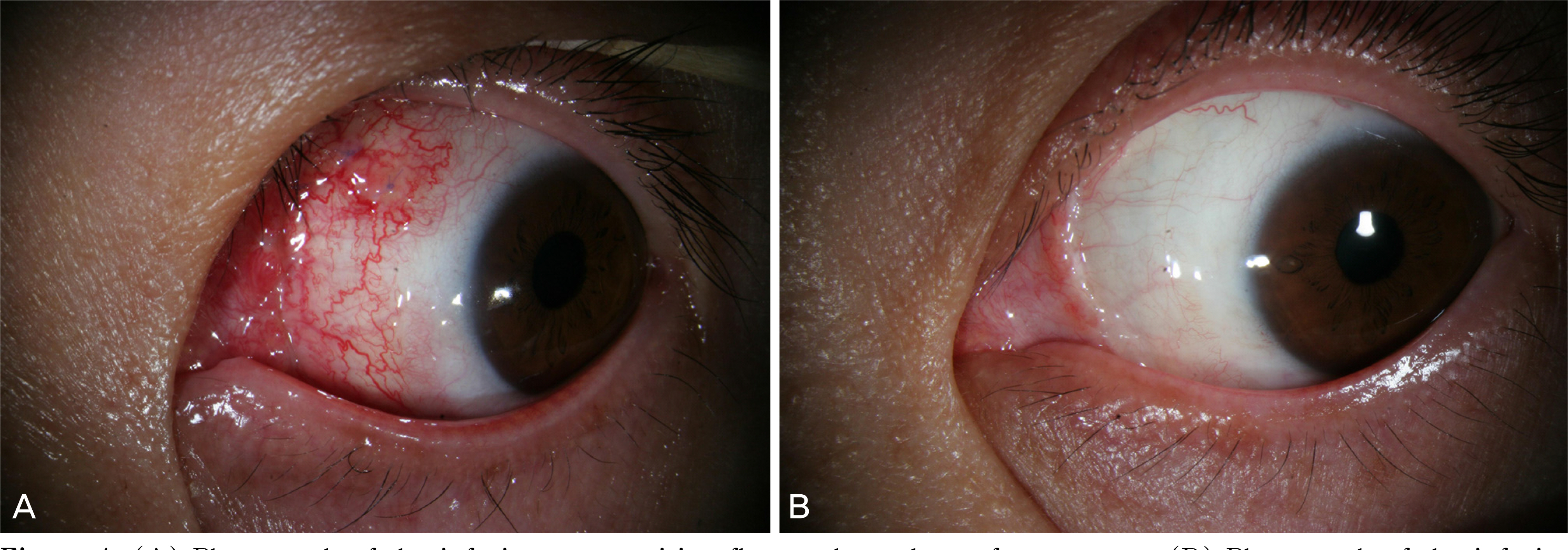
The mean patient age was 55.6 (ranging from 34 to 74) years. The mean follow-up period was 24.9 (ranging from 12 to 46) months. During the follow-up period, the pterygium recurred in one (1.7%) of the 59 eyes. There were no severe complications except for mild congestion and hemorrhage of the conjunctival flap.
CONCLUSIONS
Inferior conjunctival transposition flap technique may be considered as a safe and effective method that reduces complications and recurrences after primary pterygium excision.
MeSH Terms
Figure
Reference
-
References
1. Farid M, Pirnazar JR. Pterygium recurrence after excision with conjunctival autograft: a comparison of fibrin tissue adhesive to absorbable sutures. Cornea. 2009; 28:43–5.
Article2. Lee SH, Jeong HJ. Immune reactions in pterygium. J Korean Ophthalmol Soc. 1987; 28:933–7.3. Hirst LW. The treatment of pterygium. Surv Ophthalmol. 2003; 48:145–80.
Article4. Jaros PA, DeLuise VP. Pingueculae and pterygia. Surv Ophthalmol. 1998; 33:41–9.
Article5. Kaufman HE. Companion handbook to the cornea. 2nd ed.Woburn: Butterworth-Heinemann;2000. p. 473–98.6. Prabhasawat P, Barton K, Burkett G, Tseng SC. Comparison of conjunctival autografts, amniotic membrane grafts and primary – closure for pterygium cases. Ophthalmology. 1997; 104:974–85.7. Dushku N, Reid TW. Immunohistochemical evidence that human terygia originate from an invasion of vimentin expressing altered limbal epithelial basal cells. Curr Eye Res. 1994; 13:473–81.8. Kim S, Yang Y, Kim J. Primary pterygium surgery using the inferior conjunctival transposition flap. Ophthalmic Surg Lasers. 1998; 29:608–611.
Article9. Starck T, Kenyon KR, Serrano F. Conjunctival autograft for primary and recurrent pterygia: surgical technique and problem management. Cornea. 1991; 10:196–202.
Article10. Mahar PS, Nwokora GE. Role of mitomycin C in pterygium surgery. Br J Ophthalmol. 1993; 77:433–5.
Article11. Nishimura Y, Nakai A, Yoshimasu T, et al. Long-term results of fractionated strontium-90 radiation therapy for pterygia. Int J Radiation Oncology Biol Phys. 2000; 46:137–41.
Article12. Rubinfeld RS, Pfister RR, Stein RM, et al. Serious complications of topical mitomycin-C after pterygium surgery. Ophthalmology. 1992; 99:1647–54.
Article13. Kenyon KR, Wagoner MD, Hettinger ME. Conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology. 1985; 92:1461–70.
Article14. Frucht-Pery J, Ilsar M, Hemo I. Single dosage of mitomycin C for prevention of recurrent pterygium: preliminary report. Cornea. 1994; 13:411–3.
Article15. Singh G, Wilson MR, Foster CS. Mitomycin eye drops as treatment for pterygium. Ophthalmology. 1988; 95:813–21.
Article16. Mastropasqua L, Carpineto P, Ciancaglini M, et al. Effectiveness of intraoperative mitomycin C in the treatment of recurrent pterygium. Ophthalmologica. 1994; 208:247–9.
Article17. Kenyon KR, Tseng SC. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989; 96:709–23.
Article18. Kim JC, Tseng SC. Transplantation of preserved human amniotic membrane for surface reconstruction in severely damaged rabbit corneas. Cornea. 1995; 14:473–484.
Article19. Tseng SC, Li DQ, Ma X. Suppression of transforming growth factor-beta isoforms, TGF-beta receptor type II, and myofibroblast differentiation in cultured human corneal and limbal fibroblasts by amniotic membrane matrix. J Cell Physiol. 1999; 179:325–35.20. Kim JC, Lee DH, Shyn KH. Clinical use of human amniotic membrane for ocular surface diseases. Jonathan HL, editor. Advances in Corneal Research. Selected transections of the Proceedings of the World Congress on the Cornea. 1st ed.Florida: Plenum;1997. 4:chap. 12.21. Ma DH, See LC, Liau SB, Tsai RJ. Amniotic membrane graft for primary pterygium: comparison with conjunctival autograft and topical mitomycin C drops. Br J Ophthalmol. 2000; 84:973–8.22. Solomon A, Pires RT, Tseng SC. Amniotic membrane transplantation after extensive removal of primary and recurrent pterygia. Ophthalmology. 2001; 108:449–60.
Article23. Riordan-Eva P, Kielhorn I, Ficker LA, et al. Conjunctival autografting in the surgical management of pterygium. Eye. 1993; 7:634–8.
Article24. Dushku N, Reid TW. Immunohistochemical evidence that human pterygia originate from an invasion of vimentin expressing altered limbal epithelial basal cells. Curr Eye Res. 1994; 13:473–81.25. Dushku N, Mollyutty K, Schultz GS, Reid TW. Pterygium pathogenesis: corneal invasion by matrix metalloproteinase expressing altered limbal epithelial basal cells. Arch Ophthalmol. 2001; 119:695–706.26. Oh TH, Choi KY, Yoon BJ. The effect of conjunctival autograft for recurrent pterygium. J Korean Ophthalmol Soc. 1994; 35:1335–9.27. Ti SE, Tseng SC. Management of primary and recurrent pterygium using amniotic membrane transplantation. Curr Opin Ophthalmol. 2002; 13:204–12.
Article28. Kim YS, Kim JH, Byun YJ. Limbal-conjunctival autograft transplantation for the treatment of primary pterygium. J Korean Ophthalmol Soc. 1999; 40:1804–10.29. Allan BD, Short P, Crawford GJ, et al. Pterygium excision with conjunctival autografting: an effective and safe technique. Br J Ophthalmol. 1993; 77:698–701.
Article30. Jap A, Chan C, Lim L, et al. Conjunctival rotation autograft for pterygium. Ophthalmology. 1999; 106:67–71.
Article31. Uçakhan OO, Kanpolat A. Combined “symmetrical conjunctival flap transposition” and intraoperative low-dose mitomycin C in the treatment of primary pterygium. Clin Experiment Ophthalmol. 2006; 34:197–8.32. Mutlu FM, Sobacı G, Tatar T, Yildirim E. A comparative study of recurrent pterygium surgery. Ophthalmology. 1999; 106:817–21.33. McCoombes JA, Hirst LW, Isbell GP. Sliding conjunctival flap for the treatment of primary pterygium. Ophthalmology. 1994; 101:169–73.
Article34. Lei G. Surgery for pterygium using a conjunctival pedunculated flap slide. Br J Ophthalmol. 1996; 80:33–4.
Article35. Cho JW, Chung SH, Seo KY, Kim EK. Conjunctival Mini-flap Technique and Conjunctival Autotransplantation in Pterygium Surgery. J Korean Ophthalmol Soc. 2005; 46:1471–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Inferior Conjunctival Transposition Flap for Recurrent Pterygium
- Autogenous Temporalis Fascia Grafting and Conjunctival Flap Transposition in Scleromalacia after Pterygium Excision
- Conjunctival Mini-flap Technique and Conjunctival Autotransplantation in Pterygium Surgery
- Superior-inferior Sliding Conjunctival Flap for Pterygium with a Fibrin Tissue Adhesive (Tisseel(R))
- Postoperative Recurrence Rate of Superior-Inferior Sliding Conjunctival Flap and Mytomycin-C for the Treatment of Primary Pterygium