Korean Circ J.
2018 Jan;48(1):48-58. 10.4070/kcj.2017.0124.
Clinical Characteristics of Korean Patients with Bicuspid Aortic Valve Who Underwent Aortic Valve Surgery
- Affiliations
-
- 1Department of Cardiology, Internal Medicine, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea.
- 2Valvular Heart Disease Center, Asan Medical Center Heart Institute, Seoul, Korea. jksong@amc.seoul.kr
- 3Research Institute for Valvular Heart Disease, University of Ulsan College of Medicine, Seoul, Korea.
- 4Cardiovascular Center, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- 5Division of Cardiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Cardiovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2405045
- DOI: http://doi.org/10.4070/kcj.2017.0124
Abstract
- BACKGROUND AND OBJECTIVES
Clinical data for Korean patients with bicuspid aortic valve (BAV) that underwent aortic valve (AV) surgery are currently limited.
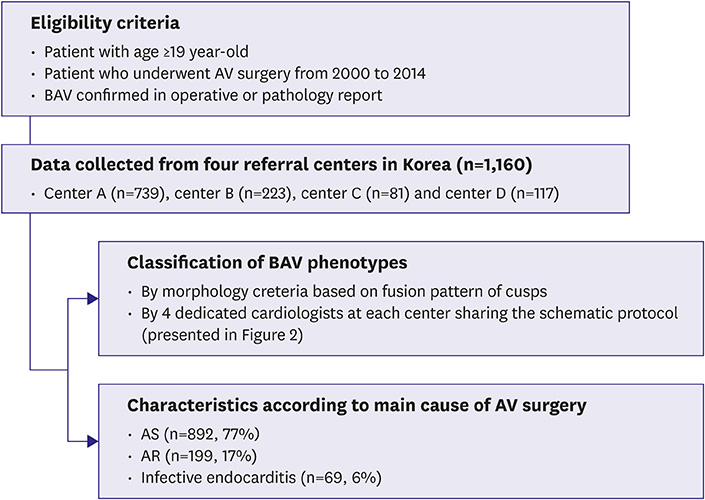
METHODS
Data for 1,160 consecutive adult BAV patients who underwent AV surgery from 2000 to 2014 in 4 tertiary referral centers were retrospectively analyzed. A standard case report form was used for clinical and echocardiographic parameters.
RESULTS
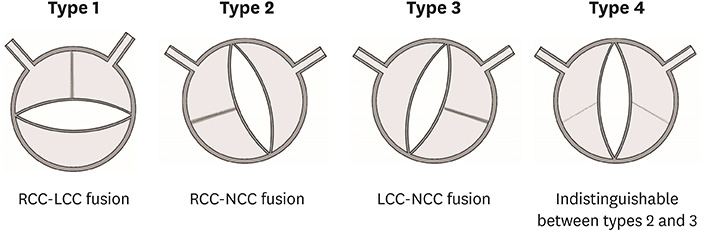
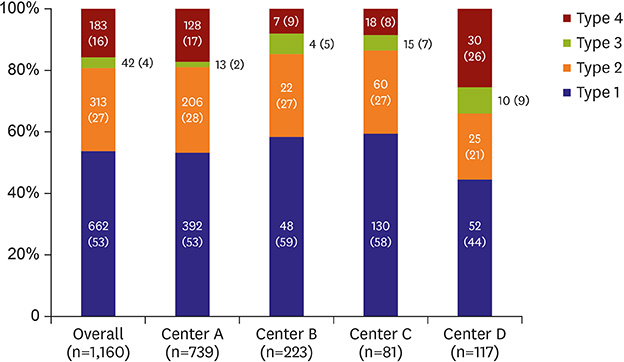
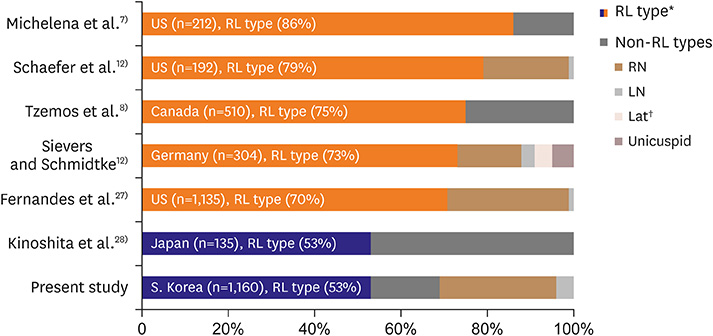
Mean age at the time of AV surgery was 59±13 years. The most common cause of AV surgery was aortic stenosis (AS, 892 [77%]), followed by aortic regurgitation (AR, 199 [17%]), and infective endocarditis (69 [6%]). AS showed a skewed peak in the aged population and was the predominant cause of AV surgery (87%) in patients ≥50 years of age, whereas AR (46%) and active infective endocarditis (19%) were more common in younger patients (p < 0.001). Echocardiographic determination of the BAV phenotype revealed that fusion of the right coronary cusp (RCC) and left coronary cusp (LCC) was most common (622 [53%]), followed by fusion of RCC and non-coronary cusp (NCC) (313 [27%]), and fusion of LCC and NCC (42 [4%]); the BAV phenotype could not be determined in the remaining 183 patients (16%). Fusion of RCC and LCC was more commonly observed in patients with AR than in those with AS (74% vs. 49%; p < 0.001).
CONCLUSION
BAV patients were characterized by distinct surgical indications according to their age. Possible associations between BAV phenotypes and surgical indications with potential impacts of ethnicity need to be tested in further studies.
MeSH Terms
Figure
Cited by 2 articles
-
Timing and Indications for Aortic Valve Surgery in Korean Bicuspid Aortic Valve Patients
Chi Young Shim, Geu-Ru Hong
Korean Circ J. 2018;48(1):82-83. doi: 10.4070/kcj.2017.0380.Mid-term Clinical Outcomes in a Cohort of Asymptomatic or Mildly Symptomatic Korean Patients with Bicuspid Aortic Valve in a Tertiary Referral Hospital
Byung Joo Sun, Jin Kyung Oh, Sun Hack Lee, Jeong Yoon Jang, Ji Hye Lee, Sahmin Lee, Dae-Hee Kim, Jong-Min Song, Duk-Hyun Kang, Jae-Kwan Song
J Cardiovasc Imaging. 2019;27(2):105-118. doi: 10.4250/jcvi.2019.27.e19.
Reference
-
1. Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002; 39:1890–1900.
Article2. Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation. 2011; 123:e18–e209.3. Fedak PW, Verma S, David TE, Leask RL, Weisel RD, Butany J. Clinical and pathophysiological implications of a bicuspid aortic valve. Circulation. 2002; 106:900–904.
Article4. Prakash SK, Bossé Y, Muehlschlegel JD, et al. A roadmap to investigate the genetic basis of bicuspid aortic valve and its complications: insights from the International BAVCon (Bicuspid Aortic Valve Consortium). J Am Coll Cardiol. 2014; 64:832–839.5. Verma S, Siu SC. Aortic dilatation in patients with bicuspid aortic valve. N Engl J Med. 2014; 370:1920–1929.
Article6. Garg V, Muth AN, Ransom JF, et al. Mutations in NOTCH1 cause aortic valve disease. Nature. 2005; 437:270–274.
Article7. Michelena HI, Desjardins VA, Avierinos JF, et al. Natural history of asymptomatic patients with normally functioning or minimally dysfunctional bicuspid aortic valve in the community. Circulation. 2008; 117:2776–2784.
Article8. Tzemos N, Therrien J, Yip J, et al. Outcomes in adults with bicuspid aortic valves. JAMA. 2008; 300:1317–1325.
Article9. Michelena HI, Khanna AD, Mahoney D, et al. Incidence of aortic complications in patients with bicuspid aortic valves. JAMA. 2011; 306:1104–1112.
Article10. Michelena HI, Prakash SK, Della Corte A, et al. Bicuspid aortic valve: identifying knowledge gaps and rising to the challenge from the International Bicuspid Aortic Valve Consortium (BAVCon). Circulation. 2014; 129:2691–2704.11. Chandra S, Lang RM, Nicolarsen J, et al. Bicuspid aortic valve: inter-racial difference in frequency and aortic dimensions. JACC Cardiovasc Imaging. 2012; 5:981–989.
Article12. Sievers HH, Schmidtke C. A classification system for the bicuspid aortic valve from 304 surgical specimens. J Thorac Cardiovasc Surg. 2007; 133:1226–1233.
Article13. Schaefer BM, Lewin MB, Stout KK, et al. The bicuspid aortic valve: an integrated phenotypic classification of leaflet morphology and aortic root shape. Heart. 2008; 94:1634–1638.
Article14. Cedars A, Braverman AC. The many faces of bicuspid aortic valve disease. Prog Pediatr Cardiol. 2012; 34:91–96.
Article15. Otto CM, Prendergast B. Aortic-valve stenosis--from patients at risk to severe valve obstruction. N Engl J Med. 2014; 371:744–756.16. Roberts WC, Ko JM. Frequency by decades of unicuspid, bicuspid, and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated aortic regurgitation. Circulation. 2005; 111:920–925.
Article17. Anguera I, Miro JM, Cabell CH, et al. Clinical characteristics and outcome of aortic endocarditis with periannular abscess in the International Collaboration on Endocarditis Merged Database. Am J Cardiol. 2005; 96:976–981.
Article18. Tribouilloy C, Rusinaru D, Sorel C, et al. Clinical characteristics and outcome of infective endocarditis in adults with bicuspid aortic valves: a multicentre observational study. Heart. 2010; 96:1723–1729.
Article19. Sabet HY, Edwards WD, Tazelaar HD, Daly RC. Congenitally bicuspid aortic valves: a surgical pathology study of 542 cases (1991 through 1996) and a literature review of 2,715 additional cases. Mayo Clin Proc. 1999; 74:14–26.
Article20. Roberts WC. The congenitally bicuspid aortic valve. A study of 85 autopsy cases. Am J Cardiol. 1970; 26:72–83.21. Angelini A, Ho SY, Anderson RH, et al. The morphology of the normal aortic valve as compared with the aortic valve having two leaflets. J Thorac Cardiovasc Surg. 1989; 98:362–367.
Article22. Boodhwani M, de Kerchove L, Glineur D, et al. Repair of regurgitant bicuspid aortic valves: a systematic approach. J Thorac Cardiovasc Surg. 2010; 140:276–284.e1.
Article23. Bissell MM, Hess AT, Biasiolli L, et al. Aortic dilation in bicuspid aortic valve disease: flow pattern is a major contributor and differs with valve fusion type. Circ Cardiovasc Imaging. 2013; 6:499–507.24. Mahadevia R, Barker AJ, Schnell S, et al. Bicuspid aortic cusp fusion morphology alters aortic three-dimensional outflow patterns, wall shear stress, and expression of aortopathy. Circulation. 2014; 129:673–682.
Article25. Guzzardi DG, Barker AJ, van Ooij P, et al. Valve-related hemodynamics mediate human bicuspid aortopathy: insights from wall shear stress mapping. J Am Coll Cardiol. 2015; 66:892–900.26. Kang JW, Song HG, Yang DH, et al. Association between bicuspid aortic valve phenotype and patterns of valvular dysfunction and bicuspid aortopathy: comprehensive evaluation using MDCT and echocardiography. JACC Cardiovasc Imaging. 2013; 6:150–161.27. Fernandes SM, Sanders SP, Khairy P, et al. Morphology of bicuspid aortic valve in children and adolescents. J Am Coll Cardiol. 2004; 44:1648–1651.
Article28. Kinoshita T, Naito S, Suzuki T, Asai T. Valve phenotype and risk factors of aortic dilatation after aortic valve replacement in Japanese patients with bicuspid aortic valve. Circ J. 2016; 80:1356–1361.
Article29. Fernández B, Durán AC, Fernández-Gallego T, et al. Bicuspid aortic valves with different spatial orientations of the leaflets are distinct etiological entities. J Am Coll Cardiol. 2009; 54:2312–2318.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ascending Aortic Aneurysm Associated with Congenital Bicuspid Aortic Valve
- Timing and Indications for Aortic Valve Surgery in Korean Bicuspid Aortic Valve Patients
- Ruptured Subvalvular Aortic Aneurysm of a Person Who Has Bicuspid Aortic Valve
- A Case of Staphylococcal Tricuspid Valve Endocarditis With Para-Aortic Abscess in a Patient With Bicuspid Aortic Valve
- Bicuspid Aortic Valve and Coronary Artery Stenosis in the Cardiac CT