J Rheum Dis.
2018 Jan;25(1):65-68. 10.4078/jrd.2018.25.1.65.
Bilateral Involvement of Juvenile Temporal Arteritis Associated with Kimura Disease
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea. ymkang@knu.ac.kr
- 2Division of Rheumatology, Department of Internal Medicine, Andong Medical Group Hospital, Andong, Korea.
- 3Department of Pathology, Kyungpook National University School of Medicine, Daegu, Korea.
- KMID: 2405022
- DOI: http://doi.org/10.4078/jrd.2018.25.1.65
Abstract
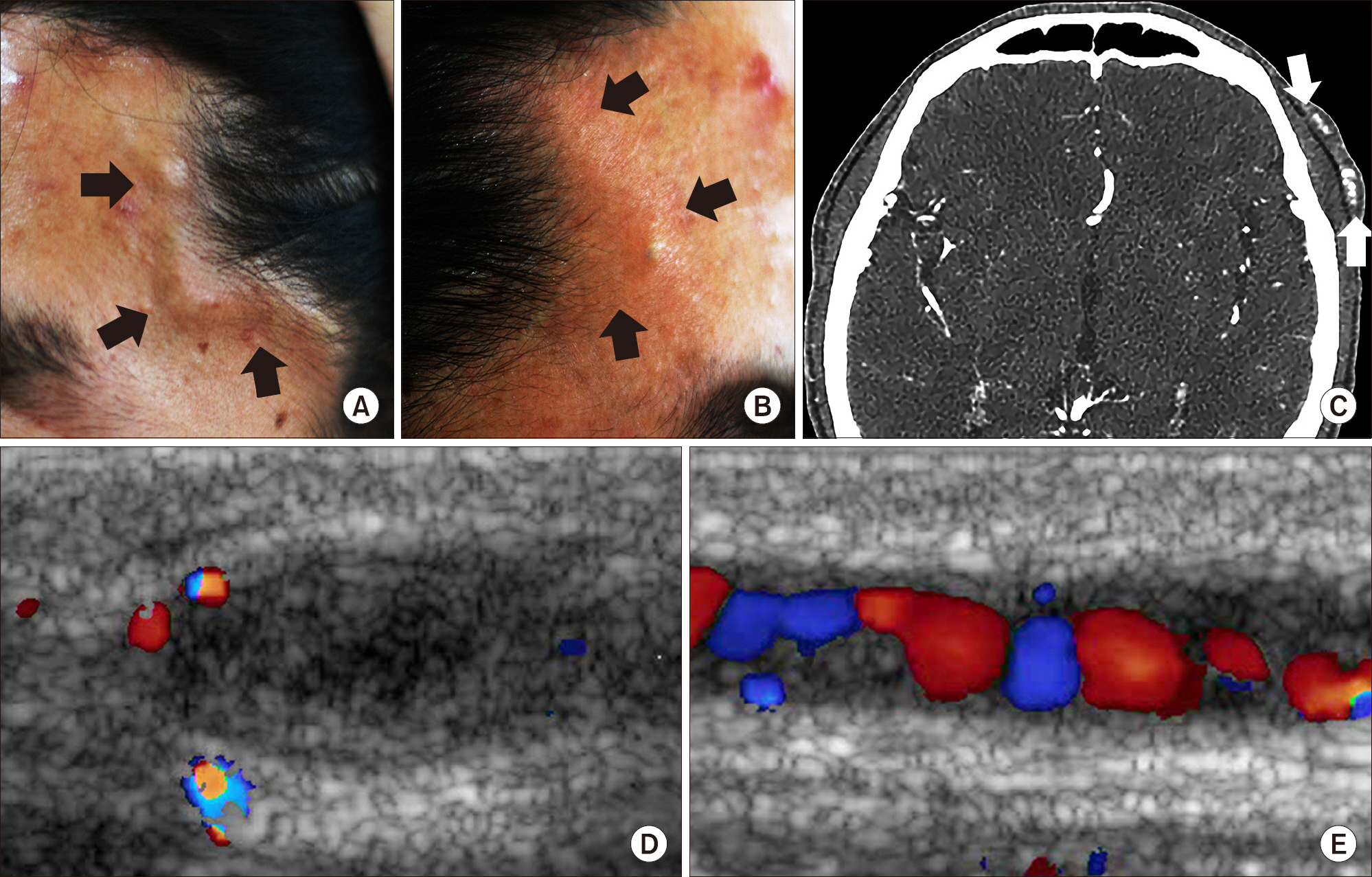
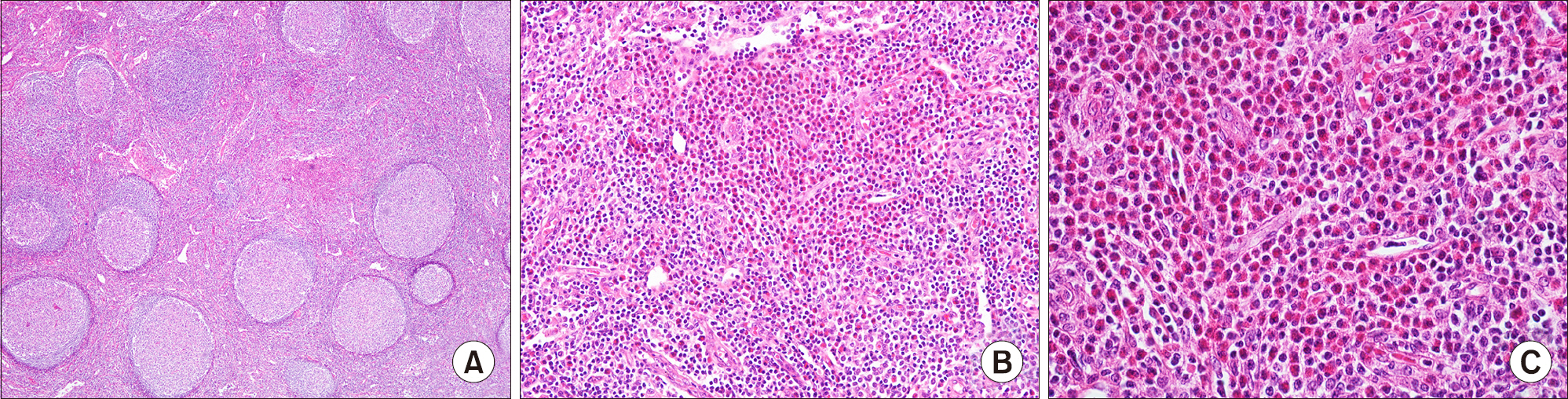
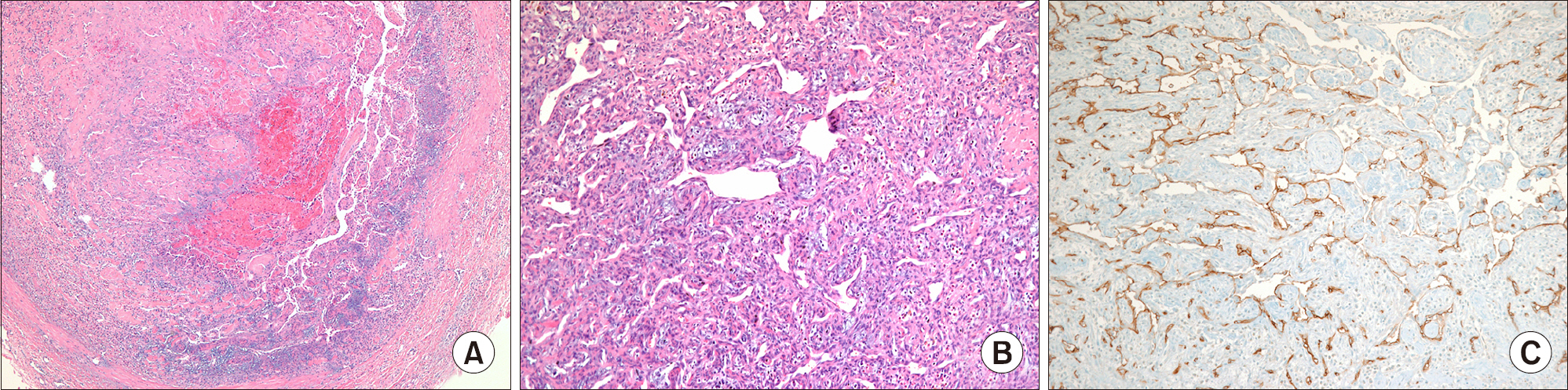
- Juvenile temporal arteritis (JTA) is a localized nodular arteritis confined to the temporal artery without evidence of systemic inflammation, and it occurs mainly in patients younger than 50 years. From the first case report, the pathological features of JTA have been suspected to be the morphological equivalent of Kimura disease (KD), which has been supported further by the concurrent cases of JTA with KD. We present the first case of bilateral JTA accompanying KD, which was confirmed by histological and ultrasound evaluations and supports the hypothesis that JTA is a manifestation of KD. The un-excised JTA lesion was resolved completely after corticosteroid therapy with no recurrence.
MeSH Terms
Figure
Cited by 1 articles
-
Concurrent bilateral juvenile temporal arteritis and hypereosinophilic syndrome: a case report and review of the literature
Ji-Su Shim, Ji Hyun Oh, Soo Jie Chung, Byung-Keun Kim, Yoon-Seok Chang, Sae-Hoon Kim
Asia Pac Allergy. 2019;9(3):. doi: 10.5415/apallergy.2019.9.e23.
Reference
-
1. Nesher G, Oren S, Lijovetzky G, Nesher R. Vasculitis of the temporal arteries in the young. Semin Arthritis Rheum. 2009; 39:96–107.
Article2. Watanabe C, Koga M, Honda Y, Oh-I T. Juvenile temporal arteritis is a manifestation of Kimura disease. Am J Dermatopathol. 2002; 24:43–9.
Article3. Brown I, Adkins G, McClymont K. Juvenile temporal arteritis: a case report. Pathology. 2005; 37:559–60.
Article4. Fukunaga M. Juvenile temporal arteritis associated with Kimura's disease. APMIS. 2005; 113:379–84.5. Kim MB, Shin DH, Seo SH. Juvenile temporal arteritis with perifollicular lymphoid proliferation resembling Kimura disease. Report of a case. Int J Dermatol. 2011; 50:70–3.
Article6. Sun QF, Xu DZ, Pan SH, Ding JG, Xue ZQ, Miao CS, et al. Kimura disease: review of the literature. Intern Med J. 2008; 38:668–72.
Article7. Kolman OK, Spinelli HM, Magro CM. Juvenile temporal arteritis. J Am Acad Dermatol. 2010; 62:308–14.
Article8. Durant C, Connault J, Graveleau J, Toquet C, Brisseau JM, Hamidou M. Juvenile temporal vasculitis: a rare case in a middle-aged woman. Ann Vasc Surg. 2011; 25:384.e5-7.
Article9. McGeoch L, Silecky WB, Maher J, Carette S, Pagnoux C. Temporal arteritis in the young. Joint Bone Spine. 2013; 80:324–7.
Article10. Bollinger A, Leu HJ, Brunner U. Juvenile arteritis of ex-tracranial arteries with hypereosinophilia. Klin Wochenschr. 1986; 64:526–9.
Article11. Lie JT. Bilateral juvenile temporal arteritis. J Rheumatol. 1995; 22:774–6.12. Fujimoto M, Sato S, Hayashi N, Wakugawa M, Tsuchida T, Tamaki K. Juvenile temporal arteritis with eosinophilia: a distinct clinicopathological entity. Dermatology. 1996; 192:32–5.
Article13. Arnander MW, Anderson NG, Schönauer F. The ultrasound halo sign in angiolymphoid hyperplasia of the temporal artery. Br J Radiol. 2006; 79:e184–6.
Article14. Arida A, Kyprianou M, Kanakis M, Sfikakis PP. The diagnostic value of ultrasonography-derived edema of the temporal artery wall in giant cell arteritis: a second meta-analysis. BMC Musculoskelet Disord. 2010; 11:44.
Article15. Dai L, Wei XN, Zheng DH, Mo YQ, Pessler F, Zhang BY. Effective treatment of Kimura's disease with leflunomide in combination with glucocorticoids. Clin Rheumatol. 2011; 30:859–65.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bilateral Involvement of Juvenile Temporal Arteritis with Eosinophilia: A Rare Case
- Concurrent bilateral juvenile temporal arteritis and hypereosinophilic syndrome: a case report and review of the literature
- Giant cell arteritis of the breast: a case report
- Generalized Actinic Granuloma with Ocular Involvement,Subsequent Development of Temporal Arteritis
- A Case of Takayasu Arteritis in a Patient with Juvenile Onset Ankylosing Spondylitis