Cancer Treatment near the End-of-Life Becomes More Aggressive: Changes in Trend during 10 Years at a Single Institute
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea. heo1013@snu.ac.kr
- 2Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2403371
- DOI: http://doi.org/10.4143/crt.2014.200
Abstract
- PURPOSE
The purpose of this study was to investigate and compare cancer treatment near the end-of-life (EOL) over a 10-year period.
MATERIALS AND METHODS
Patients with advanced solid cancer at Seoul National University Hospital who received palliative chemotherapy and had died were enrolled. We categorized the consecutive patients according to two time periods: 2002 (n=57) and 2012 (n=206). Aggressiveness of cancer treatment near the EOL was evaluated.
RESULTS
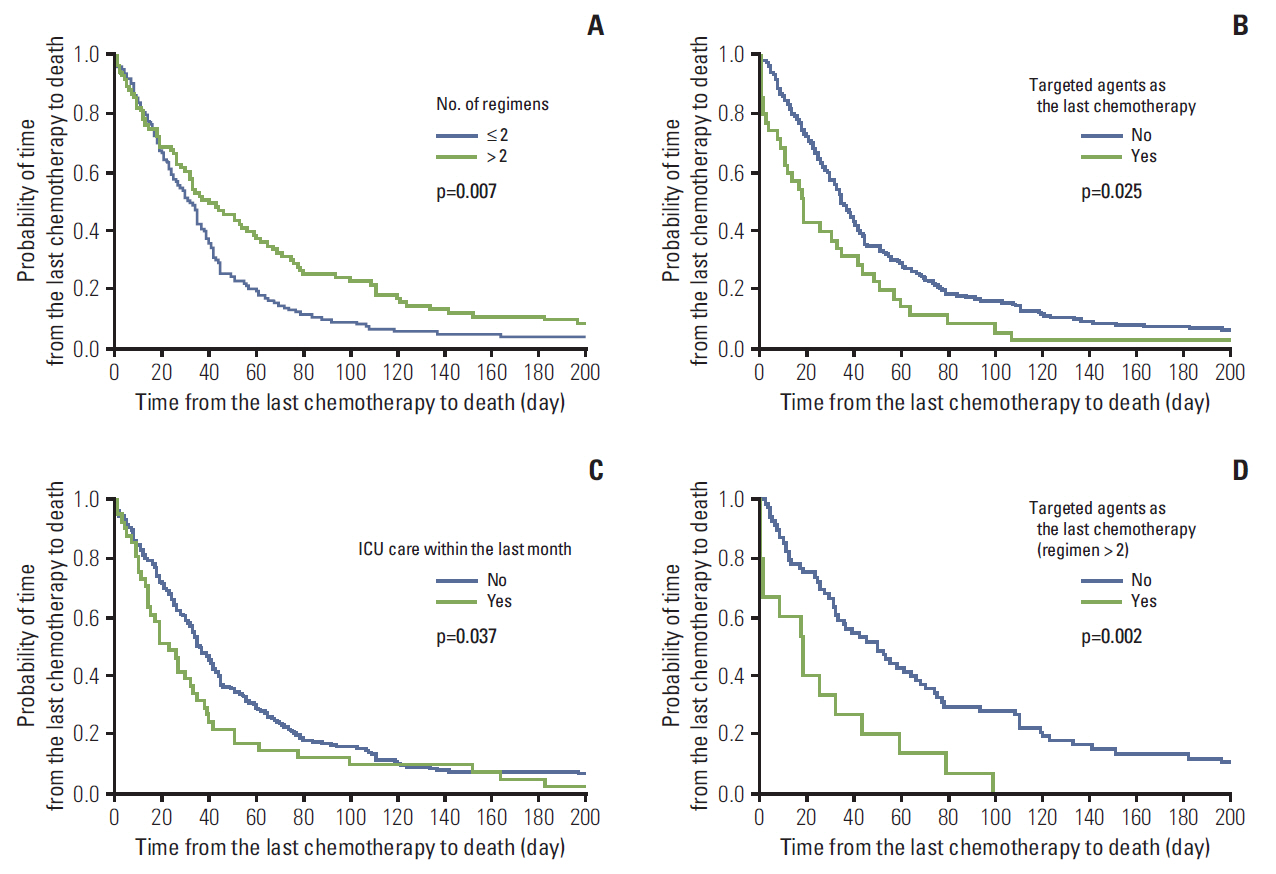
The median patient age was 62, and 65.4% of patients (n=172) were male. Time from the last chemotherapy to death (TCD) was found to have been significantly shortened, from 66.0 days to 34.0 days during 10 years (p < 0.001); 17% of patients received molecular targeted agents as the last chemotherapy regimen in 2012. The proportion of patients who received intensive care unit care within the last month increased from 1.8% in 2002 to 19.9% in 2012 (p < 0.001), and emergency room visits within the last month also increased from 22.8% to 74.8% (p < 0.001). Although hospice referral increased from 9.1% to 37.4% (p < 0.001), timing of referral was delayed from median 53 days to 8 days before death (p=0.004). Use of targeted agents as the last chemotherapy for over-two-regimen users was associated with shortened TCD (hazard ratio, 2.564; p=0.002).
CONCLUSION
Cancer treatment near the EOL became more aggressive over 10 years.
Keyword
MeSH Terms
Figure
Cited by 6 articles
-
The Disease Burden of Lung Cancer Attributable to Residential Radon Exposure in Korean Homes
Jong-Hun Kim, Mina Ha
J Korean Med Sci. 2018;33(29):. doi: 10.3346/jkms.2018.33.e223.The Effect of Hospice Consultation on Aggressive Treatment of Lung Cancer
Shin Hye Yoo, Bhumsuk Keam, Miso Kim, Tae Min Kim, Dong-Wan Kim, Dae Seog Heo
Cancer Res Treat. 2018;50(3):720-728. doi: 10.4143/crt.2017.169.Changes of End of Life Practices for Cancer Patients and Their Association with Hospice Palliative Care Referral over 2009-2014: A Single Institution Study
Hyun Jung Jho, Eun Jung Nam, Il Won Shin, Sun Young Kim
Cancer Res Treat. 2020;52(2):419-425. doi: 10.4143/crt.2018.648.Implication of the Life-Sustaining Treatment Decisions Act on End-of-Life Care for Korean Terminal Patients
Jung Sun Kim, Shin Hye Yoo, Wonho Choi, Yejin Kim, Jinui Hong, Min Sun Kim, Hye Yoon Park, Bhumsuk Keam, Dae Seog Heo
Cancer Res Treat. 2020;52(3):917-924. doi: 10.4143/crt.2019.740.Difficulties Doctors Experience during Life-Sustaining Treatment Discussion after Enactment of the Life-Sustaining Treatment Decisions Act: A Cross-Sectional Study
Shin Hye Yoo, Wonho Choi, Yejin Kim, Min Sun Kim, Hye Yoon Park, Bhumsuk Keam, Dae Seog Heo
Cancer Res Treat. 2021;53(2):584-592. doi: 10.4143/crt.2020.735.Life-Sustaining Treatment States in Korean Cancer Patients after Enforcement of Act on Decisions on Life-Sustaining Treatment for Patients at the End of Life
Young-Woong Won, Hwa Jung Kim, Jung Hye Kwon, Ha Yeon Lee, Sun Kyung Baek, Yu Jung Kim, Do Yeun Kim, Hyewon Ryu
Cancer Res Treat. 2021;53(4):908-916. doi: 10.4143/crt.2021.325.
Reference
-
References
1. World Health Organization. The 10 leading causes of death in the world, 2000 and 2011 [Internet]. Geneva: World Health Organization;2013. [cited 2014 Jul 27]. Available from: http://www.who.int/mediacentre/factsheets/fs310/en/.2. Statistics Korea. Annual report on the cause of death statistics (2012). Daejeon: Statistics Korea;2013. p. 127–43.3. Sacred Congregation for the Doctrine of the Faith. Vatican declaration on euthanasia. Origins. 1980; 10:154–7.4. Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, Weeks JC. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol. 2004; 22:315–21.
Article5. Nieder C, Tollali T, Dalhaug A, Haukland E, Aandahl G, Pawinski A, et al. Active anticancer treatment during the final month of life in patients with non-small cell lung cancer. Anticancer Res. 2014; 34:1015–20.6. Emanuel EJ, Young-Xu Y, Levinsky NG, Gazelle G, Saynina O, Ash AS. Chemotherapy use among Medicare beneficiaries at the end of life. Ann Intern Med. 2003; 138:639–43.
Article7. Yun YH, Kwak M, Park SM, Kim S, Choi JS, Lim HY, et al. Chemotherapy use and associated factors among cancer patients near the end of life. Oncology. 2007; 72:164–71.
Article8. Nappa U, Lindqvist O, Rasmussen BH, Axelsson B. Palliative chemotherapy during the last month of life. Ann Oncol. 2011; 22:2375–80.9. Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008; 300:1665–73.
Article10. Casarett DJ, Fishman JM, Lu HL, O'Dwyer PJ, Barg FK, Naylor MD, et al. The terrible choice: re-evaluating hospice eligibility criteria for cancer. J Clin Oncol. 2009; 27:953–9.
Article11. Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004; 291:88–93.
Article12. Keam B, Oh DY, Lee SH, Kim DW, Kim MR, Im SA, et al. Aggressiveness of cancer-care near the end-of-life in Korea. Jpn J Clin Oncol. 2008; 38:381–6.
Article13. Hui D, Karuturi MS, Tanco KC, Kwon JH, Kim SH, Zhang T, et al. Targeted agent use in cancer patients at the end of life. J Pain Symptom Manage. 2013; 46:1–8.
Article14. Soh TI, Yuen YC, Teo C, Lim SW, Chan N, Wong AS. Targeted therapy at the end of life in advanced cancer patients. J Palliat Med. 2012; 15:991–7.
Article15. Wong AS, Teo C, Lim SW, Wong E, Soo RA, Chan N. Targeted therapy at the end of life for patients with lung cancer. J Palliat Med. 2010; 13:945–8.
Article16. Walker H, Anderson M, Farahati F, Howell D, Librach SL, Husain A, et al. Resource use and costs of end-of-Life/palliative care: Ontario adult cancer patients dying during 2002 and 2003. J Palliat Care. 2011; 27:79–88.
Article17. Morishima T, Lee J, Otsubo T, Imanaka Y. Association of healthcare expenditures with aggressive versus palliative care for cancer patients at the end of life: a cross-sectional study using claims data in Japan. Int J Qual Health Care. 2014; 26:79.
Article18. Zhang B, Wright AA, Huskamp HA, Nilsson ME, Maciejewski ML, Earle CC, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009; 169:480–8.19. Jung HM, Kim J, Heo DS, Baek SK. Health economics of a palliative care unit for terminal cancer patients: a retrospective cohort study. Support Care Cancer. 2012; 20:29–37.
Article20. Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010; 363:733–42.
Article21. National Evidence-based Healthcare Collaborating Agency. Evaluation of the effect on medical service of the enforcement of health insurance on cancer [Internet]. Seoul: National Evidence-based Healthcare Collaborating Agency;2011. [cited 2014 Jul 27]. Available from: http://hineca.kr/m/post/164#.22. Lim JH, Choi KS, Kim SG, Park EC, Park JH. Effects of private health insurance on health care utilization and expenditures in Korean cancer patients: focused on 5 major cancers in one cancer center. J Prev Med Public Health. 2007; 40:329–35.
Article23. Chirikos TN. Cancer economics: on variations in the costs of treating cancer. Cancer Control. 2002; 9:59–66.
Article24. Colla CH, Morden NE, Skinner JS, Hoverman JR, Meara E. Impact of payment reform on chemotherapy at the end of life. Am J Manag Care. 2012; 18:e200–8.
Article25. Organization for Economic Co-operation and Development. OECD Health Data 2013 [Internet]. Paris: Organization for Economic Co-operation and Development;2013. [cited 2014 Jul 27]. Available from: http://stats.oecd.org/index.aspx?DataSetCode=HEALTH_STAT .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unmet Needs and Quality of Life of Colorectal Cancer Survivors Immediately after Treatment Ends and 5 Years
- A Mixed Method Study for Exploring the Difficulties in End-of-Life Care and End-of-Life Care Competency in Nurses Who Take Care of Cancer Patients
- The Effect of Hospice Consultation on Aggressive Treatment of Lung Cancer
- Recent Trend in the Treatment of Rheumatoid Arthritis
- Notification of Terminal Status and Advance Care Planning in Patients with Cancer