The Effect of Hospice Consultation on Aggressive Treatment of Lung Cancer
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea. bhumsuk@snu.ac.kr
- 2Cancer Research Institute, Seoul National University, Seoul, Korea.
- KMID: 2417861
- DOI: http://doi.org/10.4143/crt.2017.169
Abstract
- PURPOSE
The aims of this study were to investigate trends of aggressive treatment of non-small cell lung cancer (NSCLC) patients at the end-of-life (EOL) during the recent 5 years and examine the relationship between hospice consultation (HC) and aggressive care.
MATERIALS AND METHODS
The medical records of 789 patients with stage IIIB-IV NSCLC at Seoul National University Hospital (SNUH) who received palliative chemotherapy and died from 2010 to 2014 were retrospectively reviewed. Indicators of aggressive treatment were evaluated, and the association of HC with these indicators was analyzed.
RESULTS
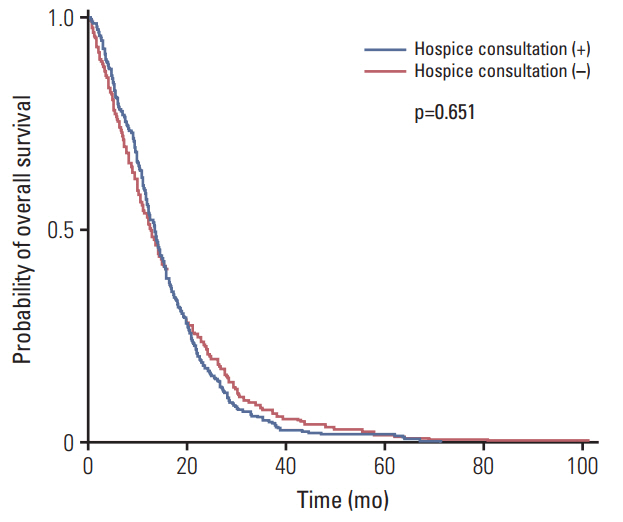
During the last 5 years, the frequency of HC increased from 26.7% to 43.6%. The time interval from last chemotherapy to death increased, and the proportion of patients who received palliative chemotherapy, visited an emergency room, were admitted to intensive care unit, during the last month of life, and died in SNUH significantly decreased over time. Referral to HC was significantly associated with lower intensive care unit admission rates, lower out-of-hospital death rates, and less use of the chemotherapy within 1 month prior to death. Overall survival did not differ by HC.
CONCLUSION
The pattern of cancer care nearthe EOL has become less aggressivewhen HCwas provided. The positive association of HCwith better EOL care suggests that providing HC at the optimal time might help to avoid futile aggressive treatment.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Demographic and Socioeconomic Factors for Renouncing Further Active Therapy for Patients with Brain Metastasis of Non-Small Cell Lung Cancer
Gyuseo Jung, Seok-Hyun Kim, Tae Gyu Kim, Young Zoon Kim
Brain Tumor Res Treat. 2019;7(2):112-121. doi: 10.14791/btrt.2019.7.e35.Changes of End of Life Practices for Cancer Patients and Their Association with Hospice Palliative Care Referral over 2009-2014: A Single Institution Study
Hyun Jung Jho, Eun Jung Nam, Il Won Shin, Sun Young Kim
Cancer Res Treat. 2020;52(2):419-425. doi: 10.4143/crt.2018.648.Implication of the Life-Sustaining Treatment Decisions Act on End-of-Life Care for Korean Terminal Patients
Jung Sun Kim, Shin Hye Yoo, Wonho Choi, Yejin Kim, Jinui Hong, Min Sun Kim, Hye Yoon Park, Bhumsuk Keam, Dae Seog Heo
Cancer Res Treat. 2020;52(3):917-924. doi: 10.4143/crt.2019.740.
Reference
-
References
1. Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, Rowland JH, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016; 66:271–89.
Article2. Forde PM, Ettinger DS. Targeted therapy for non-small-cell lung cancer: past, present and future. Expert Rev Anticancer Ther. 2013; 13:745–58.
Article3. Oh CM, Won YJ, Jung KW, Kong HJ, Cho H, Lee JK, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2013. Cancer Res Treat. 2016; 48:436–50.
Article4. Zarogoulidis P, Pataka A, Terzi E, Hohenforst-Schmidt W, Machairiotis N, Huang H, et al. Intensive care unit and lung cancer: when should we intubate? J Thorac Dis. 2013; 5 Suppl 4:S407–12.5. Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? CMAJ. 2010; 182:563–8.
Article6. Kotajima F, Kobayashi K, Sakaguchi H, Nemoto M. Lung cancer patients frequently visit the emergency room for cancer-related and -unrelated issues. Mol Clin Oncol. 2014; 2:322–6.
Article7. Massarelli E, Andre F, Liu DD, Lee JJ, Wolf M, Fandi A, et al. A retrospective analysis of the outcome of patients who have received two prior chemotherapy regimens including platinum and docetaxel for recurrent non-small-cell lung cancer. Lung Cancer. 2003; 39:55–61.
Article8. Sharma G, Freeman J, Zhang D, Goodwin JS. Trends in end-of-life ICU use among older adults with advanced lung cancer. Chest. 2008; 133:72–8.
Article9. Ho TH, Barbera L, Saskin R, Lu H, Neville BA, Earle CC. Trends in the aggressiveness of end-of-life cancer care in the universal health care system of Ontario, Canada. J Clin Oncol. 2011; 29:1587–91.
Article10. Kumar P, Wright AA, Hatfield LA, Temel JS, Keating NL. Family perspectives on hospice care experiences of patients with cancer. J Clin Oncol. 2017; 35:432–9.
Article11. Cherny NI, Catane R; European Society of Medical Oncology Taskforce on Palliative and Supportive Care. Attitudes of medical oncologists toward palliative care for patients with advanced and incurable cancer: report on a survery by the European Society of Medical Oncology Taskforce on Palliative and Supportive Care. Cancer. 2003; 98:2502–10.12. Choi Y, Keam B, Kim TM, Lee SH, Kim DW, Heo DS. Cancer treatment near the end-of-life becomes more aggressive: changes in trend during 10 years at a single institute. Cancer Res Treat. 2015; 47:555–63.
Article13. Lee JR, Lee JK, Hwang S, Kim JE, Chung JI, Kim SY. Doctor's perception and referral barriers toward palliative care for advanced cancer patients. Korean J Hosp Palliat Care. 2012; 15:10–7.
Article14. Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010; 363:733–42.
Article15. Hui D, Kim SH, Roquemore J, Dev R, Chisholm G, Bruera E. Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer. 2014; 120:1743–9.
Article16. Ford DW, Nietert PJ, Zapka J, Zoller JS, Silvestri GA. Barriers to hospice enrollment among lung cancer patients: a survey of family members and physicians. Palliat Support Care. 2008; 6:357–62.
Article17. Lu CY, Shen WC, Kao CY, Wang HM, Tang SC, Chin TL, et al. Impact of palliative care consultation service on terminally ill cancer patients: a 9-year observational cohort study in Taiwan. Medicine (Baltimore). 2016; 95:e2981.18. Wu LF, Chu CM, Chen YG, Ho CL, Pan HH. Relationship between palliative care consultation service and end-of-life outcomes. Support Care Cancer. 2016; 24:53–60.
Article19. Lee JE, Goo AJ, Cho BL. The current status of end-of-life care in Korea and legislation of well-dying act. J Korean Geriatr Soc. 2016; 20:65–70.
Article20. Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, Weeks JC. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol. 2004; 22:315–21.
Article21. Keam B, Oh DY, Lee SH, Kim DW, Kim MR, Im SA, et al. Aggressiveness of cancer-care near the end-of-life in Korea. Jpn J Clin Oncol. 2008; 38:381–6.
Article22. Nasir SS, Muthiah M, Ryder K, Clark K, Niell H, Weir A. ICU deaths in patients with advanced cancer. Am J Hosp Palliat Care. 2017; 34:173–9.
Article23. Brooks GA, Li L, Sharma DB, Weeks JC, Hassett MJ, Yabroff KR, et al. Regional variation in spending and survival for older adults with advanced cancer. J Natl Cancer Inst. 2013; 105:634–42.
Article24. Wright AA, Keating NL, Balboni TA, Matulonis UA, Block SD, Prigerson HG. Place of death: correlations with quality of life of patients with cancer and predictors of bereaved caregivers' mental health. J Clin Oncol. 2010; 28:4457–64.
Article25. Yun YH, Lee MK, Chang YJ, You CH, Kim S, Choi JS, et al. The life-sustaining treatments among cancer patients at end of life and the caregiver's experience and perspectives. Support Care Cancer. 2010; 18:189–96.
Article26. An AR, Lee JK, Yun YH, Heo DS. Terminal cancer patients' and their primary caregivers' attitudes toward hospice/palliative care and their effects on actual utilization: a prospective cohort study. Palliat Med. 2014; 28:976–85.
Article27. Baek SK, Chang HJ, Byun JM, Han JJ, Heo DS. The association between end-of-life care and the time interval between provision of a do-not-resuscitate consent and death in cancer patients in Korea. Cancer Res Treat. 2017; 49:502–8.
Article28. Kim DY, Lee KE, Nam EM, Lee HR, Lee KW, Kim JH, et al. Do-not-resuscitate orders for terminal patients with cancer in teaching hospitals of Korea. J Palliat Med. 2007; 10:1153–8.
Article29. Alsirafy SA, Mohammed AA, Al-Zahrani AS, Raheem AA, El-Kashif AT. The relation between the timing of palliative care and the frequency and timing of do-not-resuscitate orders among cancer deaths in a tertiary care hospital. Am J Hosp Palliat Care. 2015; 32:544–8.
Article30. Lee HS, Chun KH, Moon D, Yeon HK, Lee S, Lee S. Trends in receiving chemotherapy for advanced cancer patients at the end of life. BMC Palliat Care. 2015; 14:4.
Article31. Hwang I, Shin DW, Kang KH, Yang HK, Kim SY, Park JH. Medical costs and healthcare utilization among cancer decedents in the last year of life in 2009. Cancer Res Treat. 2016; 48:365–75.
Article32. Ferrell BR, Temel JS, Temin S, Alesi ER, Balboni TA, Basch EM, et al. Integration of palliative care into standard oncology care: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2017; 35:96–112.
Article33. Keating NL, Landrum MB, Rogers SO Jr, Baum SK, Virnig BA, Huskamp HA, et al. Physician factors associated with discussions about end-of-life care. Cancer. 2010; 116:998–1006.
Article34. Tang ST, Huang EW, Liu TW, Wang HM, Chen JS. A population-based study on the determinants of hospice utilization in the last year of life for Taiwanese cancer decedents, 2001-2006. Psychooncology. 2010; 19:1213–20.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Related with Utilizing Hospice Palliative Care Unit among Terminal Cancer Patients in Korea between 2010 and 2014: a Single Institution Study
- Understanding of Changes to Hospice & Palliative Care Brought by the Enforcement of the Act on Hospice & Palliative Care and Dying Patient Determination of Life Sustaining Treatments
- Hospice Medical Guideline, Non-Cancer Diseases
- Perception on Hospice, Attitudes toward Death and Needs of Hospice Care between the Patients with Cancer and Family
- The Medical Costs in Terminally Ill Cancer Patients