Allergy Asthma Immunol Res.
2018 Mar;10(2):184-186. 10.4168/aair.2018.10.2.184.
A Case of Intraoperative Anaphylaxis Caused by Bovine-Derived Thrombin
- Affiliations
-
- 1Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. craft7820@yuhs.ac
- 2Department of Orthopedic Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 3Division of Allergy and Immunology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2402980
- DOI: http://doi.org/10.4168/aair.2018.10.2.184
Abstract
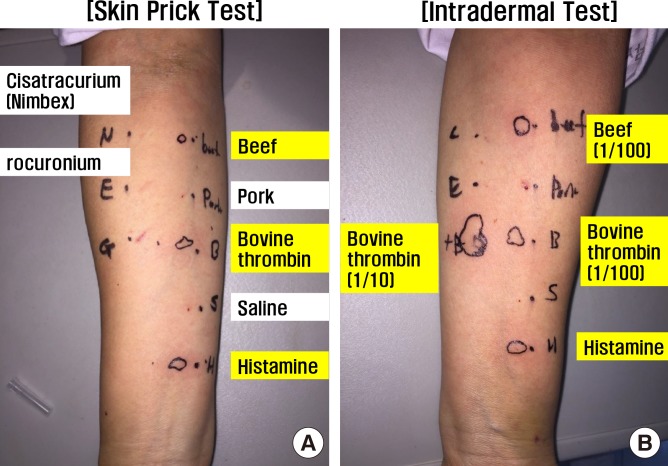
- Intraoperative bovine-derived topical thrombin is still widely used for hemostasis during surgery. A 38-year-old woman with chronic spontaneous urticaria was referred to the orthopedic surgery department for herniated disk and myelopathy. During the first stage of operation, bovine-derived thrombin powder soaked in Gelfoam was used as a hemostatic aid. After 30 minutes, the patient developed anaphylactic shock with systemic skin rash and angioedema. Repeated intravenous bolus and infusion of vasopressor were carried out, and her blood pressure normalized. Skin test and specific immunoglobulin E test showed positive results for bovine thrombin and beef, respectively. During the second stage of operation (After 10 days from first stage of operation), bovine-derived thrombin powder was excluded and the operation was successful without any unexpected events. Therefore, bovine thrombin should be used with caution because it might cause anaphylaxis.
Keyword
MeSH Terms
Figure
Reference
-
1. Bae KC, Cho CH, Lee KJ, Son ES, Lee SW, Lee SJ, et al. Efficacy of intra-articular injection of thrombin-based hemostatic agent in the control of bleeding after primary total knee arthroplasty. Knee Surg Relat Res. 2014; 26:236–240. PMID: 25505706.
Article2. Suzuki R, Matsuhashi M, Kuwahara T, Kase T. Topical use of thrombin in prostatic surgery. Hinyokika Kiyo. 1986; 32:1461–1464. PMID: 2436462.3. Lawson JH. The clinical use and immunologic impact of thrombin in surgery. Semin Thromb Hemost. 2006; 32(Suppl 1):98–110.
Article4. Clark JA, Humphries JE, Crean S, Reynolds MW. Topical bovine thrombin: a 21-year review of topical bovine thrombin spontaneous case safety reports submitted to FDA's Adverse Event Reporting System. Pharmacoepidemiol Drug Saf. 2010; 19:107–114. PMID: 20014051.
Article5. Ortel TL, Mercer MC, Thames EH, Moore KD, Lawson JH. Immunologic impact and clinical outcomes after surgical exposure to bovine thrombin. Ann Surg. 2001; 233:88–96. PMID: 11141230.
Article6. Streiff MB, Ness PM. Acquired FV inhibitors: a needless iatrogenic complication of bovine thrombin exposure. Transfusion. 2002; 42:18–26. PMID: 11896308.
Article7. Chapman WC, Singla N, Genyk Y, McNeil JW, Renkens KL Jr, Reynolds TC, et al. A phase 3, randomized, double-blind comparative study of the efficacy and safety of topical recombinant human thrombin and bovine thrombin in surgical hemostasis. J Am Coll Surg. 2007; 205:256–265. PMID: 17660072.
Article8. Ham SW, Lew WK, Weaver FA. Thrombin use in surgery: an evidence-based review of its clinical use. J Blood Med. 2010; 1:135–142. PMID: 22282693.9. Tanaka KA, Key NS, Levy JH. Blood coagulation: hemostasis and thrombin regulation. Anesth Analg. 2009; 108:1433–1446. PMID: 19372317.
Article10. Tadokoro K, Ohtoshi T, Takafuji S, Nakajima K, Suzuki S, Yamamoto K, et al. Topical thrombin-induced IgE-mediated anaphylaxis: RAST analysis and skin test studies. J Allergy Clin Immunol. 1991; 88:620–629. PMID: 1918728.
Article11. Sim DW, Lee JS, Park KH, Jeong KY, Ye YM, Lee JH, et al. Accurate assessment of alpha-gal syndrome using cetuximab and bovine thyroglobulin-specific IgE. Mol Nutr Food Res. 2017; 61:1601046.
Article12. Liang KL, Su MC, Jiang RS. Comparison of the skin test and ImmunoCAP system in the evaluation of mold allergy. J Chin Med Assoc. 2006; 69:3–6. PMID: 16447919.
Article13. Yanagida N, Sato S, Takahashi K, Nagakura KI, Ogura K, Asaumi T, et al. Skin prick test is more useful than specific IgE for diagnosis of buckwheat allergy: a retrospective cross-sectional study. Allergol Int. Forthcoming 2017.
Article14. Nacaroglu HT, Erdem SB, Karaman S, Dogan D, U Karkiner CS, Kanık ET, et al. Diagnostic values for egg white specific IgE levels with the skin prick test in Turkish children with egg white allergy. Allergol Immunopathol (Madr). 2017; 45:445–451. PMID: 28237131.
Article15. Coop CA, Schapira RS, Freeman TM. Are ACE inhibitors and beta-blockers dangerous in patients at risk for anaphylaxis? J Allergy Clin Immunol Pract. 2017; 5:1207–1211. PMID: 28552379.
Article16. Park HJ, Lee JH, Kim SR, Kim SH, Park KH, Lee CK, et al. A new practical desensitization protocol for oxaliplatin-induced immediate hypersensitivity reactions: a necessary and useful approach. J Investig Allergol Clin Immunol. 2016; 26:168–176.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anaphylaxis to topical bovine thrombin used for hemostasis during surgery for herniated nucleus pulposus: A case report
- Endovascular Thrombin Injection for a Pulmonary Artery Pseudoaneurysm: Case Report
- Intraoperative allergic reaction to fentanyl: A case report
- Percutaneous Ultrasound-Guided Thrombin Injection in Iatrogenic Arterial Pseudoaneurysms: Effectiveness and Complications
- Experimental study of sclerosing efficacy of the ethanolamine oleate and thrombin