Pediatr Gastroenterol Hepatol Nutr.
2018 Jan;21(1):43-50. 10.5223/pghn.2018.21.1.43.
Clostridium difficile Infection at Diagnosis and during the Disease Course of Pediatric Inflammatory Bowel Disease
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea. hryang@snubh.org
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2401772
- DOI: http://doi.org/10.5223/pghn.2018.21.1.43
Abstract
- PURPOSE
Clostridium difficile colonization and infection are commonly associated with poor outcomes in patients with pediatric inflammatory bowel disease (PIBD). We aimed to investigate the prevalence of C. difficile colonization and infection at the time of diagnosis and to evaluate risk factors associated with the development of C. difficile infection during the course of PIBD treatment.
METHODS
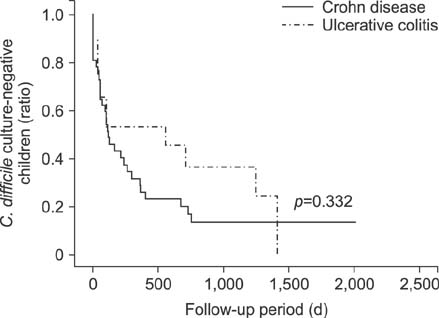
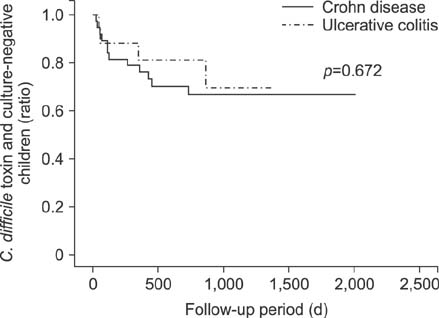
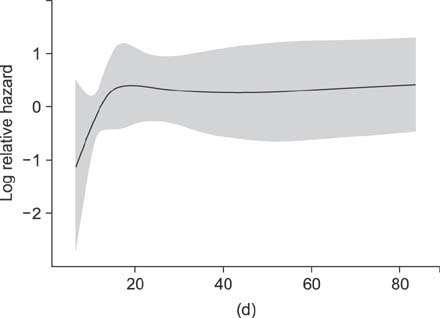
We retrospectively enrolled a total of 59 children who were newly diagnosed with PIBD at the tertiary medical center. All patients underwent C. difficile toxin assays and cultures initially and at every follow-up during the disease course. Kaplan-Meier survival analysis and Cox regression test were used for statistical analysis.
RESULTS
Initial cultures for C. difficile were positive in 13 (22.0%) of 59 PIBD patients, whereas initial toxin assays were positive in 3 patients (5.1%). During treatment, C. difficile cultures converted to positive in 28 (47.5%) in addition to 13 patients who were initially culture-positive, and C. difficile toxins converted to positive in 13 (22.0%) in addition to 3 originally toxin-positive patients. Antibiotic usage alone was significantly associated with the development of C. difficile colonization (p=0.011), and the length of hospitalization was associated with the development of C. difficile infection (p=0.032).
CONCLUSION
C. difficile colonization and infection occur frequently during the disease course of PIBD. Antibiotic usage and longer hospital stay were significant risks factors for the conversion of C. difficile status in PIBD patients undergoing treatment.
MeSH Terms
Figure
Reference
-
1. Kelly CP, Pothoulakis C, LaMont JT. Clostridium difficile colitis. N Engl J Med. 1994; 330:257–262.
Article2. Pascarella F, Martinelli M, Miele E, Del Pezzo M, Roscetto E, Staiano A. Impact of Clostridium difficile infection on pediatric inflammatory bowel disease. J Pediatr. 2009; 154:854–858.
Article3. Sokol H, Lay C, Seksik P, Tannock GW. Analysis of bacterial bowel communities of IBD patients: what has it revealed? Inflamm Bowel Dis. 2008; 14:858–867.
Article4. Ananthakrishnan AN, McGinley EL, Saeian K, Binion DG. Temporal trends in disease outcomes related to Clostridium difficile infection in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011; 17:976–983.
Article5. Mezoff E, Mann EA, Hart KW, Lindsell CJ, Cohen MB. Clostridium difficile infection and treatment in the pediatric inflammatory bowel disease population. J Pediatr Gastroenterol Nutr. 2011; 52:437–441.
Article6. Wultańska D, Banaszkiewicz A, Radzikowski A, Obuch-Woszczatyński P, Młynarczyk G, Brazier JS, et al. Clostridium difficile infection in Polish pediatric outpatients with inflammatory bowel disease. Eur J Clin Microbiol Infect Dis. 2010; 29:1265–1270.
Article7. Kelsen JR, Kim J, Latta D, Smathers S, McGowan KL, Zaoutis T, et al. Recurrence rate of Clostridium difficile infection in hospitalized pediatric patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011; 17:50–55.
Article8. Pant C, Anderson MP, Deshpande A, Altaf MA, Grunow JE, Atreja A, et al. Health care burden of Clostridium difficile infection in hospitalized children with inflammatory bowel disease. Inflamm Bowel Dis. 2013; 19:1080–1085.
Article9. Banaszkiewicz A, Kowalska-Duplaga K, Pytrus T, Pituch H, Radzikowski A. Clostridium difficile infection in newly diagnosed pediatric patients with inflammatory bowel disease: prevalence and risk factors. Inflamm Bowel Dis. 2012; 18:844–848.
Article10. Banaszkiewicz A, Pituch H. Clostridium difficile infection in children with inflammatory bowel disease: current evidence. Curr Pharm Des. 2014; 20:4549–4555.
Article11. Issa M, Vijayapal A, Graham MB, Beaulieu DB, Otterson MF, Lundeen S, et al. Impact of Clostridium difficile on inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007; 5:345–351.
Article12. Rodemann JF, Dubberke ER, Reske KA, Seo DH, Stone CD. Incidence of Clostridium difficile infection in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007; 5:339–344.
Article13. Nguyen GC, Kaplan GG, Harris ML, Brant SR. A national survey of the prevalence and impact of Clostridium difficile infection among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008; 103:1443–1450.
Article14. Schutze GE, Willoughby RE. Committee on Infectious Diseases. American Academy of Pediatrics. Clostridium difficile infection in infants and children. Pediatrics. 2013; 131:196–200.
Article15. Ananthakrishnan AN, Issa M, Binion DG. Clostridium difficile and inflammatory bowel disease. Gastroenterol Clin North Am. 2009; 38:711–728.
Article16. Musa S, Thomson S, Cowan M, Rahman T. Clostridium difficile infection and inflammatory bowel disease. Scand J Gastroenterol. 2010; 45:261–272.17. Goodhand JR, Alazawi W, Rampton DS. Systematic review: Clostridium difficile and inflammatory bowel disease. Aliment Pharmacol Ther. 2011; 33:428–441.
Article18. Gryboski JD. Clostridium difficile in inflammatory bowel disease relapse. J Pediatr Gastroenterol Nutr. 1991; 13:39–41.
Article19. Markowitz JE, Brown KA, Mamula P, Drott HR, Piccoli DA, Baldassano RN. Failure of single-toxin assays to detect Clostridium difficile infection in pediatric inflammatory bowel disease. Am J Gastroenterol. 2001; 96:2688–2690.
Article20. Monaghan TM, Cockayne A, Mahida YR. Pathogenesis of Clostridium difficile infection and its potential role in inflammatory bowel disease. Inflamm Bowel Dis. 2015; 21:1957–1966.
Article21. Gómez S, Chaves F, Orellana MA. Clinical, epidemiological and microbiological characteristics of relapse and re-infection in Clostridium difficile infection. Anaerobe. 2017; 48:147–151.
Article22. Ott C, Girlich C, Klebl F, Plentz A, Iesalnieks I, Schölmerich J, et al. Low risk of Clostridium difficile infections in hospitalized patients with inflammatory bowel disease in a German tertiary referral center. Digestion. 2011; 84:187–192.
Article23. Sokol H, Lalande V, Landman C, Bourrier A, Nion-Larmurier I, Rajca S, et al. Clostridium difficile infection in acute flares of inflammatory bowel disease: a prospective study. Dig Liver Dis. 2017; 49:643–646.
Article24. Erb S, Frei R, Strandén AM, Dangel M, Tschudin-Sutter S, Widmer AF. Low sensitivity of fecal toxin A/B enzyme immunoassay for diagnosis of Clostridium difficile infection in immunocompromised patients. Clin Microbiol Infect. 2015; 21:998.e9–998.e15.
Article25. Martinelli M, Strisciuglio C, Veres G, Paerregaard A, Pavic AM, Aloi M, et al. Clostridium difficile and pediatric inflammatory bowel disease: a prospective, comparative, multicenter, ESPGHAN study. Inflamm Bowel Dis. 2014; 20:2219–2225.26. Saffouri G, Gupta A, Loftus EV Jr, Baddour LM, Pardi DS, Khanna S. The incidence and outcomes from Clostridium difficile infection in hospitalized adults with inflammatory bowel disease. Scand J Gastroenterol. 2017; 52:1240–1247.
Article27. Hojsak I, Ferenc T, Bojanić K, Mišak Z, Močić Pavić A, et al. Incidence of Clostridium difficile infection in children with inflammatory bowel disease compared to oncology and immunocompetent patients. Digestion. 2012; 86:6–11.
Article28. Peterson LR, Manson RU, Paule SM, Hacek DM, Robicsek A, Thomson RB Jr, et al. Detection of toxigenic Clostridium difficile in stool samples by real-time polymerase chain reaction for the diagnosis of C. difficile-associated diarrhea. Clin Infect Dis. 2007; 45:1152–1160.
Article