Asia Pac Allergy.
2016 Jul;6(3):187-191. 10.5415/apallergy.2016.6.3.187.
Delayed diagnosis of allergic bronchopulmonary aspergillosis due to absence of asthmatic symptoms
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul 06974, Korea. jwjung@cau.ac.kr
- KMID: 2400421
- DOI: http://doi.org/10.5415/apallergy.2016.6.3.187
Abstract
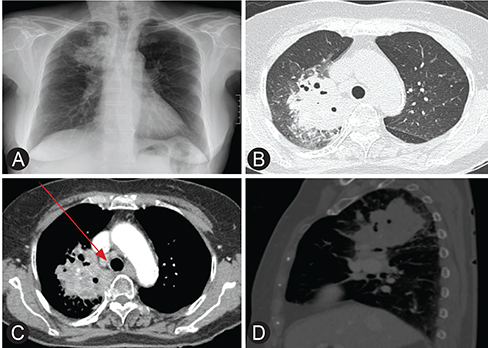
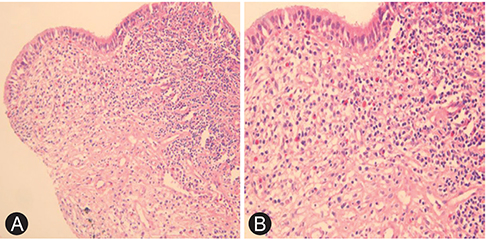
- Allergic bronchopulmonary aspergillosis (ABPA) is a pulmonary disease with small prevalence. Exposure to aspergillus mold causes immunologic hypersensitivity and may cause ranges of symptoms from minimal to detrimental outcomes. Diagnosing and treating the disease before the development of bronchiectasis may save the patient from poor outcomes. This report presents a case of recurrent ABPA without any symptom of asthma, which impeded the correct diagnosis even after numerous hospitalizations.
MeSH Terms
Figure
Cited by 1 articles
-
Advances in technology are changing the future of medicine
Yoon-Seok Chang
Asia Pac Allergy. 2016;6(3):137-138. doi: 10.5415/apallergy.2016.6.3.137.
Reference
-
1. Greenberger PA. Allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol. 2002; 110:685–692.
Article2. Agarwal R. Allergic bronchopulmonary aspergillosis. Chest. 2009; 135:805–826.
Article3. Riscili BP, Wood KL. Noninvasive pulmonary Aspergillus infections. Clin Chest Med. 2009; 30:315–335.
Article4. Agarwal R, Chakrabarti A, Shah A, Gupta D, Meis JF, Guleria R, Moss R, Denning DW. ABPA complicating asthma ISHAM working group. Allergic bronchopulmonary aspergillosis: review of literature and proposal of new diagnostic and classification criteria. Clin Exp Allergy. 2013; 43:850–873.
Article5. Wang JL, Patterson R, Rosenberg M, Roberts M, Cooper BJ. Serum IgE and IgG antibody activity against Aspergillus fumigatus as a diagnostic aid in allergic bronchopulmonary aspergillosis. Am Rev Respir Dis. 1978; 117:917–927.6. Glancy JJ, Elder JL, McAleer R. Allergic bronchopulmonary fungal disease without clinical asthma. Thorax. 1981; 36:345–349.
Article7. Agarwal R, Aggarwal AN, Gupta D, Bal A, Das A. Case report: a rare cause of miliary nodules -- allergic bronchopulmonary aspergillosis. Br J Radiol. 2009; 82:e151–e154.8. Yoshida N, Suguro H, Kohara F, Akiyama Y, Katoh H, Hashimoto N, Majima T, Yamaguchi M, Horie T, Kawabata Y. A case of allergic bronchopulmonary aspergillosis with no history of bronchial asthma. Nihon Kyobu Shikkan Gakkai Zasshi. 1992; 30:2123–2127.9. Reiff DB, Wells AU, Carr DH, Cole PJ, Hansell DM. CT findings in bronchiectasis: limited value in distinguishing between idiopathic and specific types. AJR Am J Roentgenol. 1995; 165:261–267.
Article10. Ward S, Heyneman L, Lee MJ, Leung AN, Hansell DM, Muller NL. Accuracy of CT in the diagnosis of allergic bronchopulmonary aspergillosis in asthmatic patients. AJR Am J Roentgenol. 1999; 173:937–942.
Article11. Agarwal R, Gupta D, Aggarwal AN, Saxena AK, Chakrabarti A, Jindal SK. Clinical significance of hyperattenuating mucoid impaction in allergic bronchopulmonary aspergillosis: an analysis of 155 patients. Chest. 2007; 132:1183–1190.12. D'Urzo AD, McIvor AR. Case report: allergic bronchopulmonary aspergillosis in asthma. Can Fam Physician. 2000; 46:882–884.13. Agarwal R, Gupta D, Aggarwal AN, Behera D, Jindal SK. Allergic bronchopulmonary aspergillosis: lessons from 126 patients attending a chest clinic in north India. Chest. 2006; 130:442–448.14. Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, Morrison VA, Segal BH, Steinbach WJ, Stevens DA, van Burik JA, Wingard JR, Patterson TF. Infectious Diseases Society of America. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008; 46:327–360.
Article15. Erwin GE, Fitzgerald JE. Case report: allergic bronchopulmonary aspergillosis and allergic fungal sinusitis successfully treated with voriconazole. J Asthma. 2007; 44:891–895.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Allergic Bronchopulmonary Aspergillosis Coupled with Broncholithiasis in a Non-asthmatic Patient
- Diagnosis and Treatment of Allergic Bronchopulmonary Aspergillosis
- Allergic Bronchopulmonary Aspergillosis Presenting as Recurrent Mass-like Consolidation
- A Case of Allergic Bronchopulmonary Aspergillosis
- A case of allergic bronchopulmonary aspergillosis shown as bilateral pulmonary masses