Ann Rehabil Med.
2017 Dec;41(6):915-923. 10.5535/arm.2017.41.6.915.
The Correlation Between Clinical Characteristics and Radionuclide Salivagram Findings in Patients With Brain Lesions: A Preliminary Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Daegu Fatima Hospital, Daegu, Korea. wsb0301@gmail.com
- KMID: 2400275
- DOI: http://doi.org/10.5535/arm.2017.41.6.915
Abstract
OBJECTIVE
To evaluate the correlation between radionuclide salivagram findings and clinical characteristics in dysphagic patients with brain lesions.
METHODS
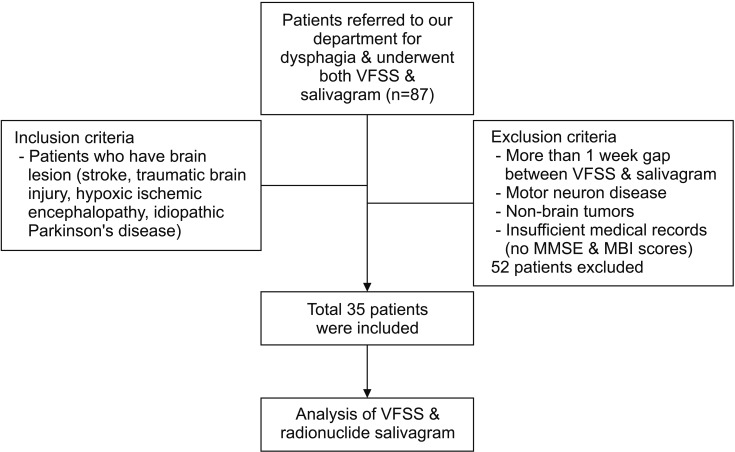
The medical records of 35 dysphagic patients with brain lesions who simultaneously underwent both a videofluoroscopic swallowing study (VFSS) and radionuclide salivagram were analyzed retrospectively. The subjects were divided into two groups according to the presence of aspiration on a salivagram (group A, patients with aspiration on the salivagram; group B, patients with no aspiration on the salivagram). The differences between clinical characteristics and VFSS findings (penetration-aspiration scale [PAS]) between the two groups were analyzed.
RESULTS
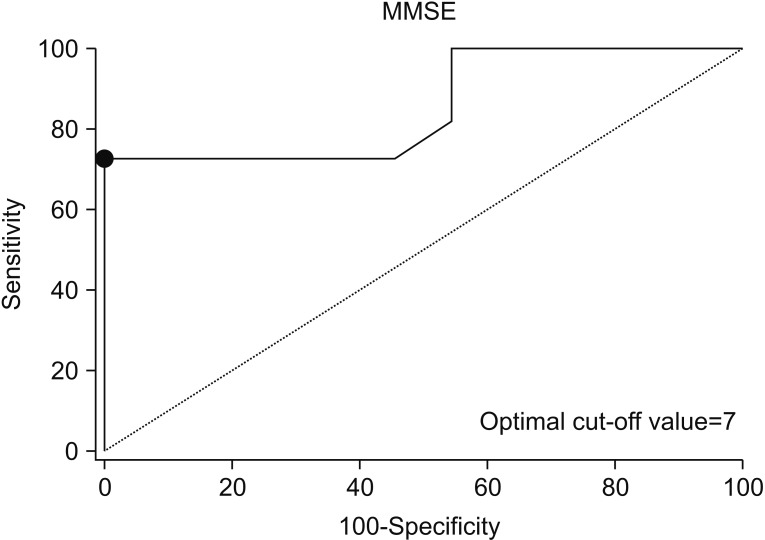
Eleven out of 35 patients displayed salivary aspiration on the radionuclide salivagram. There were no significant differences between the two groups according to age, sex, disease duration, PAS on VFSS and feeding methods (p≥0.05). The incidence of aspiration pneumonia was significantly higher in group A. In a multivariate logistic regression analysis with forward stepwise method, the Mini-Mental State Examination (MMSE) score was the only significant parameter in predicting positive findings in salivagrams (odds ratio=0.760; 95% confidence interval [CI], 0.625-0.923; p=0.006). The area under the receiver operating characteristic curve (AUC) of the MMSE score for positive detection in salivagrams was 0.855 (95% CI, 0.689-0.953; p < 0.0001). The optimal cut-off value was 7 for the MMSE score (sensitivity 72.73%, specificity 100%).
CONCLUSION
In patients with brain lesions who complain of dysphagia, the MMSE score was correlated with salivary aspiration. If patients present with a score of 7 or less on the MMSE, performing a radionuclide salivagram may helpful for early detection of patients at high risk of aspiration pneumonia induced from salivary aspiration.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Correlation of Videofluoroscopic Swallowing Study Findings With Radionuclide Salivagram in Chronic Brain-Injured Patients
Ga Yang Shim, Ju Sun Oh, Seunghee Han, Kyungyeul Choi, Son Mi Lee, Min Woo Kim
Ann Rehabil Med. 2021;45(2):108-115. doi: 10.5535/arm.20171.
Reference
-
1. Vermeij FH, Scholte op Reimer WJ, de Man P, van Oostenbrugge RJ, Franke CL, de Jong G, et al. Stroke-associated infection is an independent risk factor for poor outcome after acute ischemic stroke: data from the Netherlands Stroke Survey. Cerebrovasc Dis. 2009; 27:465–471. PMID: 19329851.
Article2. Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics: 2012 update: a report from the American Heart Association. Circulation. 2012; 125:e2–e220. PMID: 22179539.3. Marik PE. Pulmonary aspiration syndromes. Curr Opin Pulm Med. 2011; 17:148–154. PMID: 21311332.
Article4. Boesch RP, Daines C, Willging JP, Kaul A, Cohen AP, Wood RE, et al. Advances in the diagnosis and management of chronic pulmonary aspiration in children. Eur Respir J. 2006; 28:847–861. PMID: 17012631.
Article5. Aviv JE, Sacco RL, Mohr JP, Thompson JL, Levin B, Sunshine S, et al. Laryngopharyngeal sensory testing with modified barium swallow as predictors of aspiration pneumonia after stroke. Laryngoscope. 1997; 107:1254–1260. PMID: 9292613.
Article6. Croghan JE, Burke EM, Caplan S, Denman S. Pilot study of 12-month outcomes of nursing home patients with aspiration on videofluoroscopy. Dysphagia. 1994; 9:141–146. PMID: 8082320.
Article7. Heyman S, Respondek M. Detection of pulmonary aspiration in children by radionuclide “salivagram”. J Nucl Med. 1989; 30:697–699. PMID: 2715832.8. Heyman S. The radionuclide salivagram for detecting the pulmonary aspiration of saliva in an infant. Pediatr Radiol. 1989; 19:208–209. PMID: 2497434.
Article9. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–98. PMID: 8721066.
Article10. Lee ZI, Cho DH, Choi WD, Park DH, Byun SD. Effect of botulinum toxin type a on morphology of salivary glands in patients with cerebral palsy. Ann Rehabil Med. 2011; 35:636–640. PMID: 22506185.
Article11. Li X, Kolltveit KM, Tronstad L, Olsen I. Systemic diseases caused by oral infection. Clin Microbiol Rev. 2000; 13:547–558. PMID: 11023956.
Article12. Baikie G, South MJ, Reddihough DS, Cook DJ, Cameron DJ, Olinsky A, et al. Agreement of aspiration tests using barium videofluoroscopy, salivagram, and milk scan in children with cerebral palsy. Dev Med Child Neurol. 2005; 47:86–93. PMID: 15707231.
Article13. Heyman S. Volume-dependent pulmonary aspiration of a swallowed radionuclide bolus. J Nucl Med. 1997; 38:103–104. PMID: 8998162.14. Silver KH, Van Nostrand D. The use of scintigraphy in the management of patients with pulmonary aspiration. Dysphagia. 1994; 9:107–115. PMID: 8005005.
Article15. Nakagawa T, Sekizawa K, Arai H, Kikuchi R, Manabe K, Sasaki H. High incidence of pneumonia in elderly patients with basal ganglia infarction. Arch Intern Med. 1997; 157:321–324. PMID: 9040300.
Article16. Kang IS, Kwon JG, Lee SU, Lee ZI, Park GY, Park HW. Detection of saliva aspiration using salivagram in bedridden patients with brain lesion. J Korean Acad Rehabil Med. 2010; 34:503–507.17. Kang Y, Chun MH, Lee SJ. Evaluation of salivary aspiration in brain-injured patients with tracheostomy. Ann Rehabil Med. 2013; 37:96–102. PMID: 23525725.18. Jang DH, Choi KH, Kim DH, Lim CM, Kim JS. Comparison between the radionuclide salivagram and videofluoroscopic swallowing study methods for evaluating patients with aspiration pneumonia. Ann Nucl Med. 2013; 27:247–252. PMID: 23283641.
Article19. Meningaud JP, Pitak-Arnnop P, Chikhani L, Bertrand JC. Drooling of saliva: a review of the etiology and management options. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:48–57. PMID: 16360607.
Article20. Lee ZI, Yu KJ, Lee DH, Hong SK, Woo SB, Kim JM, et al. The effect of nebulized glycopyrrolate on posterior drooling in patients with brain injury: two cases of different brain lesions. Am J Phys Med Rehabil. 2017; 96:e155–e158. PMID: 28081026.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correlation of Videofluoroscopic Swallowing Study Findings With Radionuclide Salivagram in Chronic Brain-Injured Patients
- Detection of Saliva Aspiration Using Salivagram in Bedridden Patients with Brain Lesion
- Evaluation of Salivary Aspiration in Brain-Injured Patients With Tracheostomy
- Comparison of Videofluoroscopic Swallowing Study and Radionuclide Salivagram for Aspiration Pneumonia in Children With Swallowing Difficulty
- Radionuclide Cisternographic Findings in Patients with Intracranial Hypotension