Ann Rehabil Med.
2013 Feb;37(1):96-102. 10.5535/arm.2013.37.1.96.
Evaluation of Salivary Aspiration in Brain-Injured Patients With Tracheostomy
- Affiliations
-
- 1Department of Rehabilitation Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. mhchun@amc.seoul.kr
- KMID: 2266656
- DOI: http://doi.org/10.5535/arm.2013.37.1.96
Abstract
OBJECTIVE
To determine the useful tool for evaluating salivary aspiration in brain-injured patients with tracheostomy.
METHODS
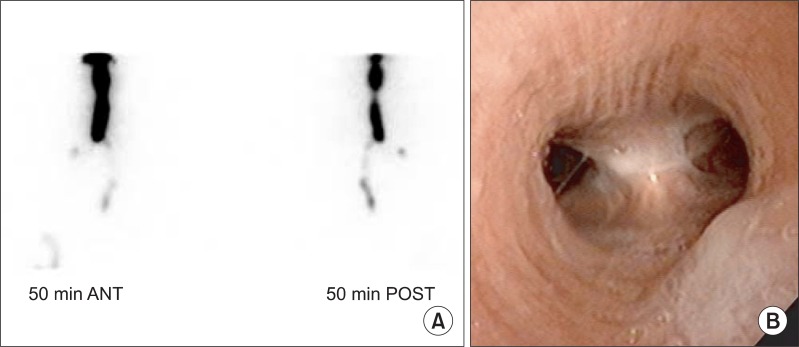
Radionuclide salivagram and laryngoscopy was done in 27 brain-injured patients with tracheostomy. During salivagram, 99mTc sulfur colloid was placed sublingually in the supine position, and 50-minute dynamic images and 2-hour delayed images were obtained. Salivary aspiration was detected when the tracer was entered into the major airways or lung parenchyma. Laryngoscopy was done by otolaryngologists, and saliva aspiration, saliva pooling, and vocal cord palsy were evaluated. Videofluoroscopic swallowing study was done in patients who were able to undergo the test.
RESULTS
The detection rate of salivary aspiration was 44.4% with salivagram, and 29.6% with laryngoscopy. The correlation of the two tests was 70.4%. Of the laryngoscopy findings, salivary pooling had significant correlation with positive salivagram results (p=0.04). Frequent need of suction correlated with salivary aspiration in both salivagram (p=0.01) and laryngoscopy (p=0.01). Patients with negative results in salivagram or laryngoscopy had higher rates of progressing to oral feeding or tapering tracheostomy. Two patients developed aspiration pneumonia, and both patients only showed aspiration in salivagram.
CONCLUSION
Brain-injured patients with tracheostomy have a high risk of salivary aspiration. Evaluation of salivary aspiration is important, as it may predict aspiration pneumonia and aids in clinical decisions of oral feeding or tracheostomy removal. Salivagram is more sensitive than laryngoscopy, but laryngoscopy may be useful for evaluating structural abnormalities or for follow-up examinations to assess the changes.
MeSH Terms
Figure
Cited by 2 articles
-
Comparison of Videofluoroscopic Swallowing Study and Radionuclide Salivagram for Aspiration Pneumonia in Children With Swallowing Difficulty
Go Eun Kim, In Young Sung, Eun Jae Ko, Kyoung Hyo Choi, Jae Seung Kim
Ann Rehabil Med. 2018;42(1):52-58. doi: 10.5535/arm.2018.42.1.52.Correlation of Videofluoroscopic Swallowing Study Findings With Radionuclide Salivagram in Chronic Brain-Injured Patients
Ga Yang Shim, Ju Sun Oh, Seunghee Han, Kyungyeul Choi, Son Mi Lee, Min Woo Kim
Ann Rehabil Med. 2021;45(2):108-115. doi: 10.5535/arm.20171.
Reference
-
1. Boesch RP, Daines C, Willging JP, Kaul A, Cohen AP, Wood RE, et al. Advances in the diagnosis and management of chronic pulmonary aspiration in children. Eur Respir J. 2006; 28:847–861. PMID: 17012631.
Article2. Kang IS, Kwon JG, Lee SU, Lee ZI, Park GY, Park HW. Detection of saliva aspiration using salivagram in bedridden patients with brain lesion. J Korean Acad Rehabil Med. 2010; 34:503–507.3. Heyman S, Respondek M. Detection of pulmonary aspiration in children by radionuclide "salivagram". J Nucl Med. 1989; 30:697–699. PMID: 2715832.4. Heyman S. The radionuclide salivagram for detecting the pulmonary aspiration of saliva in an infant. Pediatr Radiol. 1989; 19:208–209. PMID: 2497434.
Article5. Baikie G, South MJ, Reddihough DS, Cook DJ, Cameron DJ, Olinsky A, et al. Agreement of aspiration tests using barium videofluoroscopy, salivagram, and milk scan in children with cerebral palsy. Dev Med Child Neurol. 2005; 47:86–93. PMID: 15707231.
Article6. Murray J, Langmore SE, Ginsberg S, Dostie A. The significance of accumulated oropharyngeal secretions and swallowing frequency in predicting aspiration. Dysphagia. 1996; 11:99–103. PMID: 8721067.
Article7. Elpern EH, Jacobs ER, Bone RC. Incidence of aspiration in tracheally intubated adults. Heart Lung. 1987; 16:527–531. PMID: 3115917.8. Donzelli J, Brady S, Wesling M, Theisen M. Secretions, occlusion status, and swallowing in patients with a tracheotomy tube: a descriptive study. Ear Nose Throat J. 2006; 85:831–834. PMID: 17240710.
Article9. Baikie G, Reddihough DS, South M, Cook DJ. The salivagram in severe cerebral palsy and able-bodied adults. J Paediatr Child Health. 2009; 45:342–345. PMID: 19490413.
Article10. Bar-Sever Z, Connolly LP, Treves ST. The radionuclide salivagram in children with pulmonary disease and a high risk of aspiration. Pediatr Radiol. 1995; 25(Suppl 1):S180–S183. PMID: 8577521.
Article11. Levin K, Colon A, DiPalma J, Fitzpatrick S. Using the radionuclide salivagram to detect pulmonary aspiration and esophageal dysmotility. Clin Nucl Med. 1993; 18:110–114. PMID: 8432052.
Article12. Silver KH, Van Nostrand D. Scintigraphic detection of salivary aspiration: description of a new diagnostic technique and case reports. Dysphagia. 1992; 7:45–49. PMID: 1424829.
Article13. Cook SP, Lawless S, Mandell GA, Reilly JS. The use of the salivagram in the evaluation of severe and chronic aspiration. Int J Pediatr Otorhinolaryngol. 1997; 41:353–361. PMID: 9350494.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correlation of Videofluoroscopic Swallowing Study Findings With Radionuclide Salivagram in Chronic Brain-Injured Patients
- Effect of Passy-Muir Speaking Valve in Brain-injured Patients with Dysphagia: Two cases report
- Effect of Tracheostomy Tube on Swallowing in Patients with Stroke
- Dextrose Swallowing Test to Detect Aspiration for Patient with Tracheostomy
- The Effects of Tracheostomy for the Functional Outcomes of Severe Traumatic Brain Injury Patients