Korean J Endocr Surg.
2017 Mar;17(1):19-24. 10.16956/kaes.2017.17.1.19.
Endoscopic Thyroidectomy Via the Cervico-axillary Approach for Thyroid Cancer: Initial Experience in a Single Institute
- Affiliations
-
- 1Department of Surgery, Ewha Womans University College of Medicine, Seoul, Korea. mbit@ewha.ac.kr
- 2Breast and Thyroid Cancer Center, Ewha Womans University College of Medicine, Seoul, Korea.
- KMID: 2397988
- DOI: http://doi.org/10.16956/kaes.2017.17.1.19
Abstract
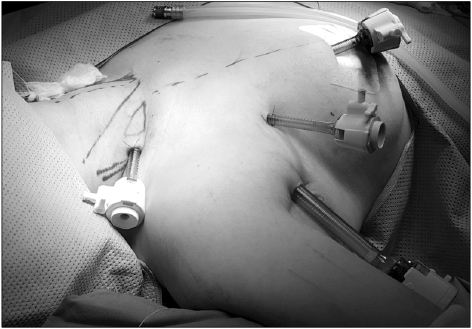
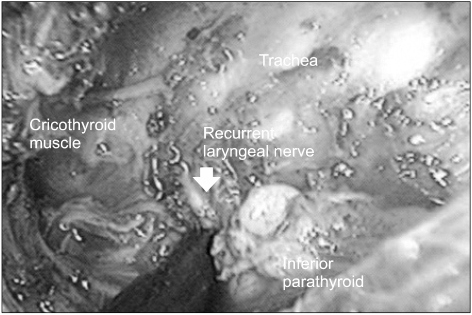
- PURPOSE
Endoscopic thyroidectomy using a cervico-axillary approach (CAA) provides optimal visualization with a smaller dissection plane. Despite the excellent cosmetic results and high patient satisfaction, the surgical and oncologic safety of CAA endoscopic surgery has not been fully established. The present study evaluated the feasibility, safety, and surgical outcomes of CAA endoscopic thyroidectomy.
METHODS
From October 2009 to April 2012, 100 patients with papillary thyroid cancer underwent CAA endoscopic thyroidectomy. Patient demographics, pathologic features, and surgical outcomes including complications and recurrence were collected.
RESULTS
CAA endoscopic thyroidectomy was successful in all patients, and none required conversion to open thyroidectomy. All patients underwent ipsilateral thyroid lobectomy with or without central compartment neck dissection. The mean tumor size was 1.0±0.6 cm (range, 0.5~1.6), and 35.0% of tumors showed extrathyroidal extension. The mean number of harvested lymph nodes was 4.1±4.4, and metastasis was found in 12.0% of patients. The mean surgical time was 175.2±50.4 min, mean intraoperative blood loss was 42.5±69.2 ml, and the mean hospital stay was 3.3±0.6 days. There were five cases of postoperative transient hypocalcemia and eight cases of vocal cord palsy. No permanent complication or postoperative bleeding was observed. Patients continued to be seen for a median period of 63.7 months, and no recurrence of thyroid cancer was seen.
CONCLUSION
CAA endoscopic thyroidectomy is a feasible and safe procedure for low-risk thyroid cancer, with excellent cosmesis. It can be recommended as an alternative option for selected patients with low-risk thyroid cancer.
MeSH Terms
Figure
Reference
-
1. Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol. 2013; 2013:965212.
Article2. Jung KW, Won YJ, Oh CM, Kong HJ, Cho H, Lee JK, et al. Prediction of Cancer Incidence and Mortality in Korea, 2016. Cancer Res Treat. 2016; 48:451–457.
Article3. Lee S, Ryu HR, Park JH, Kim KH, Kang SW, Jeong JJ, et al. Excellence in robotic thyroid surgery: a comparative study of robot-assisted versus conventional endoscopic thyroidectomy in papillary thyroid microcarcinoma patients. Ann Surg. 2011; 253:1060–1066.4. Choi JY, Lee KE, Chung KW, Kim SW, Choe JH, Koo do H, et al. Endoscopic thyroidectomy via bilateral axillo-breast approach (BABA): review of 512 cases in a single institute. Surg Endosc. 2012; 26:948–955.
Article5. Lee S, Kim HY, Lee CR, Park S, Son H, Kang SW, et al. A prospective comparison of patient body image after robotic thyroidectomy and conventional open thyroidectomy in patients with papillary thyroid carcinoma. Surgery. 2014; 156:117–125.
Article6. Lee J, Kwon IS, Bae EH, Chung WY. Comparative analysis of oncological outcomes and quality of life after robotic versus conventional open thyroidectomy with modified radical neck dissection in patients with papillary thyroid carcinoma and lateral neck node metastases. J Clin Endocrinol Metab. 2013; 98:2701–2708.
Article7. Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg. 1996; 83:875.
Article8. Huscher CS, Chiodini S, Napolitano C, Recher A. Endoscopic right thyroid lobectomy. Surg Endosc. 1997; 11:877.
Article9. Miccoli P, Berti P, Raffaelli M, Conte M, Materazzi G, Galleri D. Minimally invasive video-assisted thyroidectomy. Am J Surg. 2001; 181:567–570.
Article10. Jeong JJ, Kang SW, Yun JS, Sung TY, Lee SC, Lee YS, et al. Comparative study of endoscopic thyroidectomy versus conventional open thyroidectomy in papillary thyroid microcarcinoma (PTMC) patients. J Surg Oncol. 2009; 100:477–480.
Article11. Lee H, Lee J, Sung KY. Comparative study comparing endoscopic thyroidectomy using the axillary approach and open thyroidectomy for papillary thyroid microcarcinoma. World J Surg Oncol. 2012; 10:269.
Article12. Moon BI, Yi NJ. Supraclavicular endoscopic thyroidectomy. J Minim Invasive Surg. 2002; 5:175–180.13. Lee A, Jang J, Lim W, Moon BI. Comparison of endoscopic thyroidectomy versus conventional thyroidectomy in patient satisfaction with cosmestic result. Korean J Endocr Surg. 2010; 10:170–175.
Article14. Park YM, Lim WS, Moon BI. Comparison study endoscopic thyroidectomy versus robot-assisted thyroidectomy by a cervico-transaxillary approach. Korean J Endocr Surg. 2012; 12:264–270.
Article15. Choe JH, Kim SW, Chung KW, Park KS, Han W, Noh DY, et al. Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg. 2007; 31:601–606.
Article16. Ikeda Y, Takami H, Niimi M, Kan S, Sasaki Y, Takayama J. Endoscopic thyroidectomy by the axillary approach. Surg Endosc. 2001; 15:1362–1364.
Article17. Witzel K, von Rahden BH, Kaminski C, Stein HJ. Transoral access for endoscopic thyroid resection. Surg Endosc. 2008; 22:1871–1875.
Article18. Park KN, Cho SH, Lee SW. Nationwide multicenter survey for current status of endoscopic thyroidectomy in Korea. Clin Exp Otorhinolaryngol. 2015; 8:149–154.
Article19. Inabnet WB 3rd. Robotic thyroidectomy: must we drive a luxury sedan to arrive at our destination safely? Thyroid. 2012; 22:988–990.
Article20. Ito Y, Fukushima M, Higashiyama T, Kihara M, Takamura Y, Kobayashi K, et al. Tumor size is the strongest predictor of microscopic lymph node metastasis and lymph node recurrence of N0 papillary thyroid carcinoma. Endocr J. 2013; 60:113–117.
Article21. Chai YJ, Suh H, Woo JW, Yu HW, Song RY, Kwon H, et al. Surgical safety and oncological completeness of robotic thyroidectomy for thyroid carcinoma larger than 2 cm. Surg Endosc. 2016; in press.22. Li Y, Zhou X. Comparison between endoscopic thyroidectomy and conventional open thyroidectomy for papillary thyroid microcarcinoma: a meta-analysis. J Cancer Res Ther. 2016; 12:550–555.
Article23. Randolph GW. Surgery of the thyroid and parathyroid glands. 2nd ed. Philadelphia: Elsevier Saunders;2013.24. Bakkar S, Frustaci G, Papini P, Fregoli L, Matteucci V, Materazzi G, et al. Track recurrence after robotic transaxillary thyroidectomy: a case report highlighting the importance of controlled surgical indications and addressing unprecedented complications. Thyroid. 2016; 26:559–561.
Article25. Beninato T, Kleiman DA, Scognamiglio T, Fahey TJ, Zarnegar R. Tract recurrence of a follicular thyroid neoplasm following transaxillary endoscopic thyroidectomy. Thyroid. 2012; 22:214–217.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Thyroidectomy
- Gasless Endoscopic Thyroidectomy by an Axillary Approach(Preliminary Report)
- A Clinical Analysis of Endoscopic Thyroidectomy by the Axillary and Anterior Chest Approach
- Gasless Endoscopic Thyroidectomy via an Axillary Approach: Short-term Outcomes and Modifications of Approach
- Gasless Endoscopic Thyroidectomy Via an Axillary Approach: Experience of 30 Cases