Brain Tumor Res Treat.
2017 Oct;5(2):120-126. 10.14791/btrt.2017.5.2.120.
Astroblastoma in a Young Female Patient: A Case Report and Literature Review of Clinicopathological, Radiological and Prognostic Characteristics and Current Treatment Strategies
- Affiliations
-
- 1Center for Nuclear Medicine and Radiotherapy, Quetta, Pakistan.
- 2Institute of Radiotherapy and Nuclear Medicine, Peshawar, Pakistan. iahmadmp@gmail.com
- 3Agha Khan University Hospital, Karachi, Pakistan.
- KMID: 2396458
- DOI: http://doi.org/10.14791/btrt.2017.5.2.120
Abstract
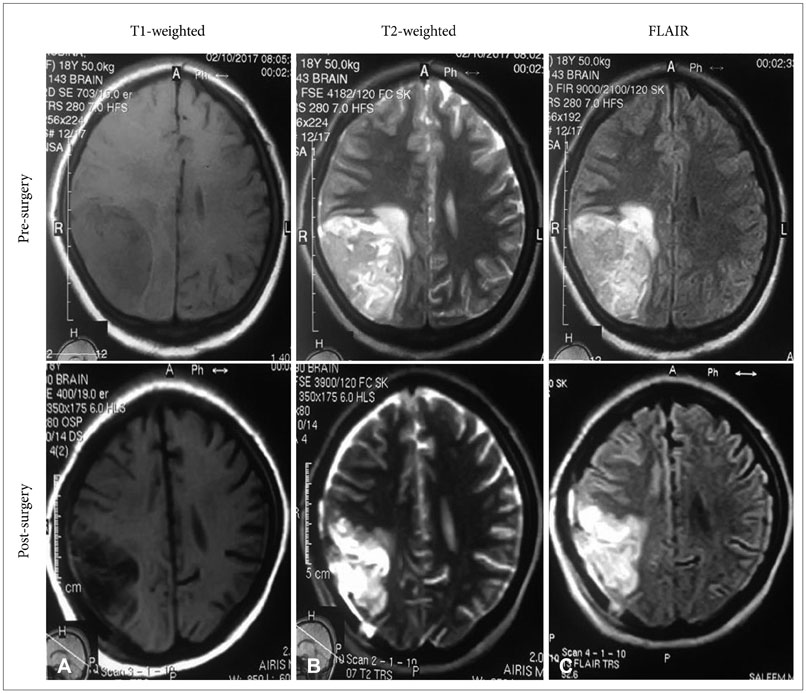
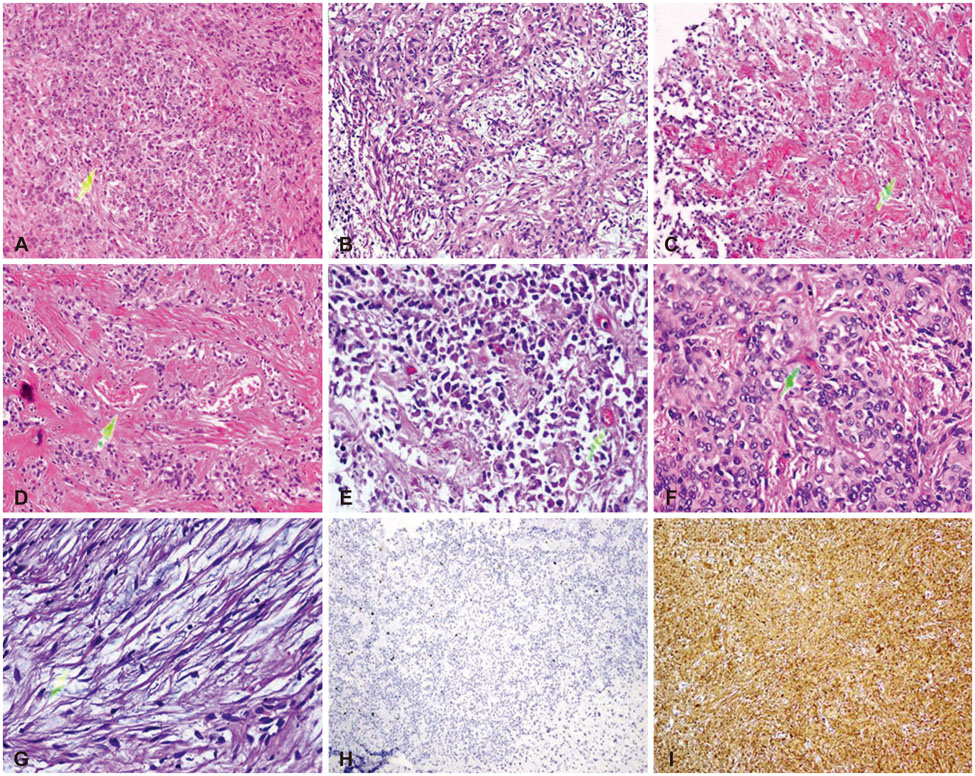
- Astroblastoma is an uncommon glial tumor with predominant manifestation in the young age. Herein, we report a case of 18-year-old astroblastoma female patient who presented with history of two months headache. Magnetic resonance imaging (MRI) of the brain demonstrated well circumscribed, intra-axial abnormal signal intensity lesion (size=5×4 cm²) in the right parieto-occipital region of the brain. The patient underwent complete surgical resection of the gross tumor, as confirmed by an early post-surgical MRI (i.e., within 24 hours of surgery). Histopathological examination revealed neoplastic lesion exhibiting perivascular pseudo-rosettes with centrally hyalinized blood vessel and focal nuclear pleomorphism. Immunohistochemistry staining illustrated reactivity for glial fibrillary acidic protein and integrase interactor 1 (INI-1). These features rendered the diagnosis of astroblastoma. A comprehensive review of the current literature to summarize the clinicopathological and radiological characteristics, prognostic factors and current treatment strategies of astroblastomas is also presented. Our study would expand the pool of this uncommon tumor towards its better understanding and optimal treatment.
MeSH Terms
Figure
Reference
-
1. Pizer BL, Moss T, Oakhill A, Webb D, Coakham HB. Congenital astroblastoma: an immunohistochemical study. Case report. J Neurosurg. 1995; 83:550–555.2. Mallick S, Benson R, Venkatesulu B, Melgandi W, Rath GK. Patterns of care and survival outcomes in patients with astroblastoma: an individual patient data analysis of 152 cases. Childs Nerv Syst. 2017; 33:1295–1302.
Article3. Ahmed KA, Allen PK, Mahajan A, Brown PD, Ghia AJ. Astroblastomas: a Surveillance, Epidemiology, and End Results (SEER)-based patterns of care analysis. World Neurosurg. 2014; 82:e291–e297.
Article4. Johnson KA, Bonnin JM, Boaz JC, Douglas-Akinwande AC, Hattab EM. Anaplastic astroblastoma presenting as massive, sudden-onset, intraparenchymal hemorrhage. Pediatr Neurosurg. 2010; 46:457–461.
Article5. Miranda P, Lobato RD, Cabello A, Gómez PA, Martínez de. Complete surgical resection of high-grade astroblastoma with long time survival: case report and review of the literature. Neurocirugia (Astur). 2006; 17:60–63.
Article6. Mangano FT, Bradford AC, Mittler MA, Valderrama E, Schneider SJ. Astroblastoma. Case report, review of the literature, and analysis of treatment strategies. J Neurosurg Sci. 2007; 51:21–27. discussion 27.7. Cunningham DA, Lowe LH, Shao L, Acosta NR. Neuroradiologic characteristics of astroblastoma and systematic review of the literature: 2 new cases and 125 cases reported in 59 publications. Pediatr Radiol. 2016; 46:1301–1308.
Article8. Baka JJ, Patel SC, Roebuck JR, Hearshen DO. Predominantly extraaxial astroblastoma: imaging and proton MR spectroscopy features. AJNR Am J Neuroradiol. 1993; 14:946–950.9. Samples DC, Henry J, Bazan C, Tarasiewicz I. A case of astroblastoma: radiological and histopathological characteristics and a review of current treatment options. Surg Neurol Int. 2016; 7:Suppl 40. S1008–S1012.
Article10. Sugita Y, Terasaki M, Shigemori M, Morimatsu M, Honda E, Oshima Y. Astroblastoma with unusual signet-ring-like cell components: a case report and literature review. Neuropathology. 2002; 22:200–205.
Article11. Port JD, Brat DJ, Burger PC, Pomper MG. Astroblastoma: radiologic-pathologic correlation and distinction from ependymoma. AJNR Am J Neuroradiol. 2002; 23:243–247.12. Salvati M, D'Elia A, Brogna C, et al. Cerebral astroblastoma: analysis of six cases and critical review of treatment options. J Neurooncol. 2009; 93:369–378.
Article13. Unal E, Koksal Y, Vajtai I, Toy H, Kocaogullar Y, Paksoy Y. Astroblastoma in a child. Childs Nerv Syst. 2008; 24:165–168.
Article14. Brat DJ, Hirose Y, Cohen KJ, Feuerstein BG, Burger PC. Astroblastoma: clinicopathologic features and chromosomal abnormalities defined by comparative genomic hybridization. Brain Pathol. 2000; 10:342–352.
Article15. Sadiq M, Ahmad I, Shuja J, Ahmad K. Primary Ewing sarcoma of the kidney: a case report and treatment review. CEN Case Rep. 2017; [Epub]. DOI: 10.1007/s13730-017-0259-0.
Article16. Shuja J, Ahmad I, Ahmad K, et al. Pleuropulmonary blastoma. J Cancer Res Pract. 2017; 4:111–114.
Article17. Iftikhar S, Ahmad I, Qasmi IM, Ahmad K, Manzoor H. Tuberous sclerosis complex with sub-ependymal giant cell astrocytomas; a case report. J Cancer Res Pract. 2017; [Epub]. DOI: 10.1016/j.jcrpr.2017.05.002.18. Notarianni C, Akin M, Fowler M, Nanda A. Brainstem astroblastoma: a case report and review of the literature. Surg Neurol. 2008; 69:201–205.
Article19. Sughrue ME, Choi J, Rutkowski MJ, et al. Clinical features and postsurgical outcome of patients with astroblastoma. J Clin Neurosci. 2011; 18:750–754.
Article20. Bell JW, Osborn AG, Salzman KL, Blaser SI, Jones BV, Chin SS. Neuroradiologic characteristics of astroblastoma. Neuroradiology. 2007; 49:203–209.
Article21. Tumialán LM, Brat DJ, Fountain AJ, Barrow DL. An astroblastoma mimicking a cavernous malformation: case report. Neurosurgery. 2007; 60:E569–E570. discussion E570.22. Bitoh S, Hasegawa H, Ohtsuki H, Obashi J, Fujiwara M, Sakurai M. Cerebral neoplasms initially presenting with massive intracerebral hemorrhage. Surg Neurol. 1984; 22:57–62.
Article23. Navarro R, Reitman AJ, de León GA, Goldman S, Marymont M, Tomita T. Astroblastoma in childhood: pathological and clinical analysis. Childs Nerv Syst. 2005; 21:211–220.
Article24. Fu YJ, Taniguchi Y, Takeuchi S, et al. Cerebral astroblastoma in an adult: an immunohistochemical, ultrastructural and genetic study. Neuropathology. 2013; 33:312–319.
Article25. Barakat MI, Ammar MG, Salama HM, Abuhashem S. Astroblastoma: case report and review of literature. Turk Neurosurg. 2016; 26:790–794.26. Kubota T, Sato K, Arishima H, Takeuchi H, Kitai R, Nakagawa T. Astroblastoma: immunohistochemical and ultrastructural study of distinctive epithelial and probable tanycytic differentiation. Neuropathology. 2006; 26:72–81.
Article27. Bale TA, Abedalthagafi M, Bi WL, et al. Genomic characterization of recurrent high-grade astroblastoma. Cancer Genet. 2016; 209:321–330.
Article28. Lehman NL, Hattab EM, Mobley BC, et al. Morphological and molecular features of astroblastoma, including BRAFV600E mutations, suggest an ontological relationship to other cortical-based gliomas of children and young adults. Neuro Oncol. 2017; 19:31–42.
Article29. Kato Y. Specific monoclonal antibodies against IDH1/2 mutations as diagnostic tools for gliomas. Brain Tumor Pathol. 2015; 32:3–11.
Article30. Shen F, Chen LC, Yao Y, Zhou LF. Astroblastoma: rare incidence and challenges in the pattern of care. World Neurosurg. 2014; 82:e125–e127.
Article31. Bonnin JM, Rubinstein LJ. Astroblastomas: a pathological study of 23 tumors, with a postoperative follow-up in 13 patients. Neurosurgery. 1989; 25:6–13.
Article32. Bergkåsa M, Sundstrøm S, Gulati S, Torp SH. Astroblastoma-a case report of a rare neuroepithelial tumor with complete remission after chemotherapy. Clin Neuropathol. 2011; 30:301–306.
Article33. Yuzawa S, Nishihara H, Tanino M, et al. A case of cerebral astroblastoma with rhabdoid features: a cytological, histological, and immunohistochemical study. Brain Tumor Pathol. 2016; 33:63–70.
Article34. Caroli E, Salvati M, Esposito V, Orlando ER, Giangaspero F. Cerebral astroblastoma. Acta Neurochir (Wien). 2004; 146:629–633.
Article35. Janz C, Buhl R. Astroblastoma: report of two cases with unexpected clinical behavior and review of the literature. Clin Neurol Neurosurg. 2014; 125:114–124.
Article