Cancer Res Treat.
2017 Oct;49(4):1088-1096. 10.4143/crt.2016.473.
Can We Skip Intraoperative Evaluation of Sentinel Lymph Nodes? Nomogram Predicting Involvement of Three or More Axillary Lymph Nodes before Breast Cancer Surgery
- Affiliations
-
- 1Department of Surgery, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea.
- 2Department of Surgery, Chung-Ang University College of Medicine, Seoul, Korea.
- 3Department of Surgery, Seoul National University College of Medicine, Seoul, Korea. hanw@snu.ac.kr
- 4Department of Surgery, Seoul St. Mary's Hospital, Seoul, Korea.
- 5Department of Surgery, Asan Medical Center, Seoul, Korea.
- 6Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- 7Department of Pathology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2394827
- DOI: http://doi.org/10.4143/crt.2016.473
Abstract
- PURPOSE
The American College of Surgeons Oncology Group Z0011 trial reported that complete dissection of axillary lymph nodes (ALNs) may not be warranted in women with clinical T1-T2 tumors and one or two involved ALNs who were undergoing lumpectomy plus radiation followed by systemic therapy. The present study was conducted to identify preoperative imaging predictors of ≥ 3 ALNs.
MATERIALS AND METHODS
The training set consisted of 1,917 patients with clinical T1-T2 and node negative invasive breast cancer. Factors associated with ≥ 3 involved ALNs were evaluated by logistic regression analysis. The validation set consisted of 378 independent patients. The nomogram was applied prospectively to 512 patients who met the Z0011 criteria.
RESULTS
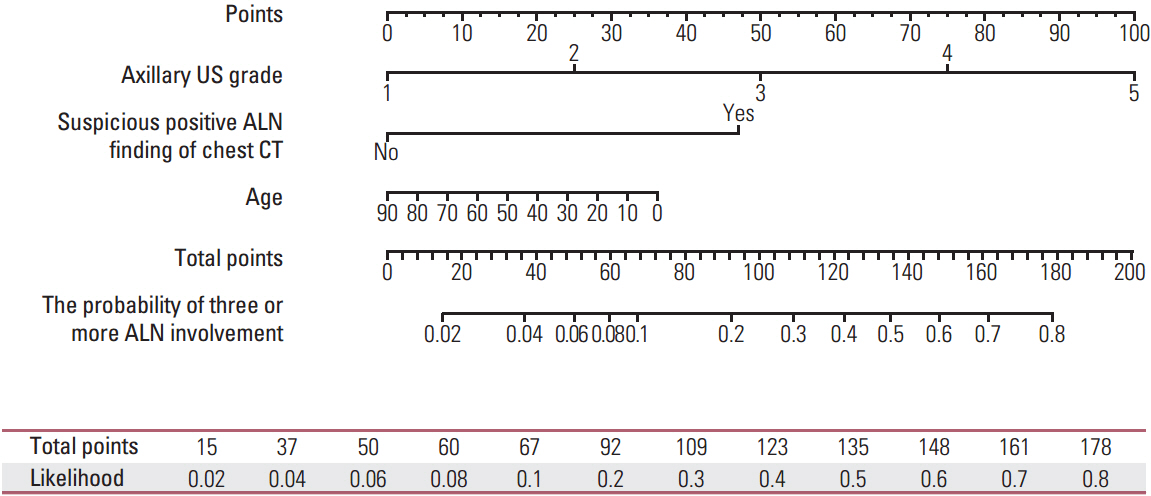
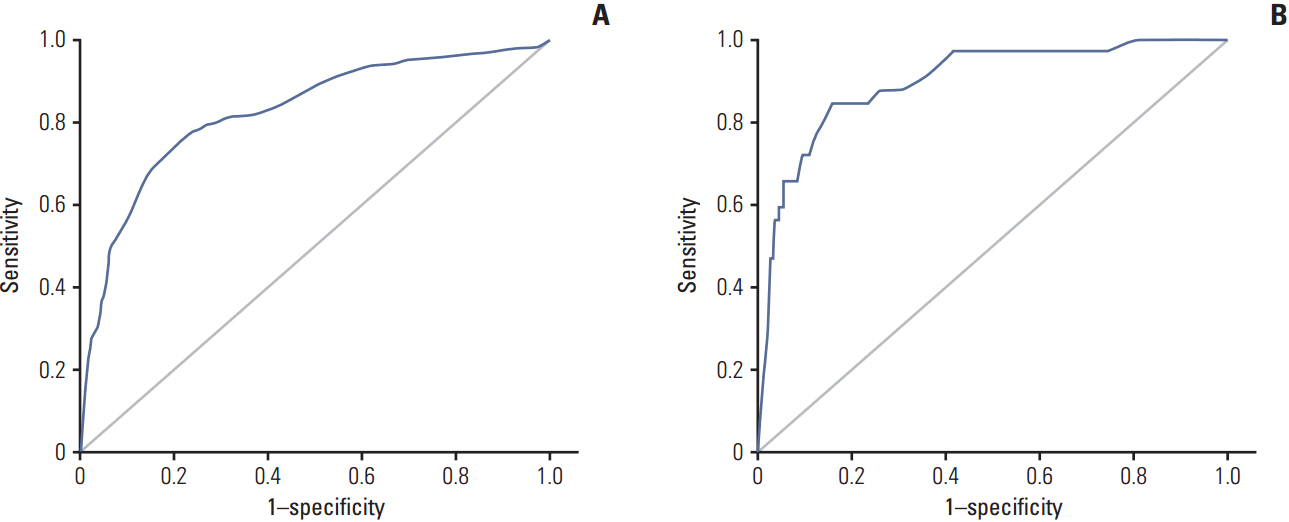
Of the 1,917 patients, 204 (10.6%) had ≥ 3 positive nodes. Multivariate analysis showed that involvement of ≥ 3 nodes was significantly associated with ultrasonographic and chest computed tomography findings of suspicious ALNs (p < 0.001 each). These two imaging criteria, plus patient age, were used to develop a nomogram calculating the probability of involvement of ≥ 3 ALNs. The areas under the receiver operating characteristic curve of the nomogram were 0.852 (95% confidence interval [CI], 0.820 to 0.883) for the training set and 0.896 (95% CI, 0.836 to 0.957) for the validation set. Prospective application of the nomogram showed that 60 of 512 patients (11.7%) had scores above the cut-off. Application of the nomogram reduced operation time and cost, with a very low re-operation rate (1.6%).
CONCLUSION
Patients likely to have ≥ 3 positive ALNs could be identified by preoperative imaging. The nomogram was helpful in selective intraoperative examination of sentinel lymph nodes.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Value of Axillary Ultrasonography in Breast Cancer with Lymph Node Metastases
Jung Ho Park, Hyun Ryung Kim, Sanghwa Kim, Young Ah Lim, Kyoonsoon Jung, Lee Su Kim
J Surg Ultrasound. 2021;8(2):41-47. doi: 10.46268/jsu.2021.8.2.41.
Reference
-
References
1. Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011; 305:569–75.2. Setton J, Cody H, Tan L, Morrow M, Hudis C, Catalano J, et al. Radiation field design and regional control in sentinel lymph node-positive breast cancer patients with omission of axillary dissection. Cancer. 2012; 118:1994–2003.
Article3. Taffurelli M, Montroni I, Santini D, Fiacchi M, Zanotti S, Ugolini G, et al. Effectiveness of sentinel lymph node intraoperative examination in 753 women with breast cancer: are we overtreating patients? Ann Surg. 2012; 255:976–80.4. Valente SA, Levine GM, Silverstein MJ, Rayhanabad JA, Weng-Grumley JG, Ji L, et al. Accuracy of predicting axillary lymph node positivity by physical examination, mammography, ultrasonography, and magnetic resonance imaging. Ann Surg Oncol. 2012; 19:1825–30.
Article5. Moon HG, Han W, Noh DY. Underweight and breast cancer recurrence and death: a report from the Korean Breast Cancer Society. J Clin Oncol. 2009; 27:5899–905.
Article6. Cho N, Moon WK, Han W, Park IA, Cho J, Noh DY. Preoperative sonographic classification of axillary lymph nodes in patients with breast cancer: node-to-node correlation with surgical histology and sentinel node biopsy results. AJR Am J Roentgenol. 2009; 193:1731–7.
Article7. Kim H, Han W, Moon HG, Min J, Ahn SK, Kim TY, et al. The value of preoperative staging chest computed tomography to detect asymptomatic lung and liver metastasis in patients with primary breast carcinoma. Breast Cancer Res Treat. 2011; 126:637–41.
Article8. Han A, Moon HG, Kim J, Ahn SK, Park IA, Han W, et al. Reliability of sentinel lymph node biopsy after neoadjuvant chemotherapy in breast cancer patients. J Breast Cancer. 2013; 16:378–85.
Article9. Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008; 26:1364–70.
Article10. Cipolla C, Cabibi D, Fricano S, Vieni S, Gentile I, Latteri MA. The value of intraoperative frozen section examination of sentinel lymph nodes in surgical management of breast carcinoma. Langenbecks Arch Surg. 2010; 395:685–91.
Article11. Schwartz GF, Krill LS, Palazzo JP, Dasgupta A. Value of intraoperative examination of axillary sentinel nodes in carcinoma of the breast. J Am Coll Surg. 2008; 207:758–62.
Article12. Liu W, Zakharia Y, Tan W, Wilding G, Edge S, Tan D, et al. Intraoperative detection of sentinel lymph node metastases from breast cancer: does the pathologist experience, subspecialty or the surgeon experience matter? Lab Invest. 2010; 90:59A.13. Weber WP, Barry M, Stempel MM, Junqueira MJ, Eaton AA, Patil SM, et al. A 10-year trend analysis of sentinel lymph node frozen section and completion axillary dissection for breast cancer: are these procedures becoming obsolete? Ann Surg Oncol. 2012; 19:225–32.
Article14. Chan SW, LaVigne KA, Port ER, Fey JV, Brogi E, Borgen PI, et al. Does the benefit of sentinel node frozen section vary between patients with invasive duct, invasive lobular, and favorable histologic subtypes of breast cancer? Ann Surg. 2008; 247:143–9.
Article15. Chao C, Wong SL, Ackermann D, Simpson D, Carter MB, Brown CM, et al. Utility of intraoperative frozen section analysis of sentinel lymph nodes in breast cancer. Am J Surg. 2001; 182:609–15.
Article16. Tanis PJ, Boom RP, Koops HS, Faneyte IF, Peterse JL, Nieweg OE, et al. Frozen section investigation of the sentinel node in malignant melanoma and breast cancer. Ann Surg Oncol. 2001; 8:222–6.
Article17. Weiser MR, Montgomery LL, Susnik B, Tan LK, Borgen PI, Cody HS. Is routine intraoperative frozen-section examination of sentinel lymph nodes in breast cancer worthwhile? Ann Surg Oncol. 2000; 7:651–5.
Article18. Rahusen FD, Pijpers R, Van Diest PJ, Bleichrodt RP, Torrenga H, Meijer S. The implementation of the sentinel node biopsy as a routine procedure for patients with breast cancer. Surgery. 2000; 128:6–12.
Article19. Veronesi U, Paganelli G, Viale G, Galimberti V, Luini A, Zurrida S, et al. Sentinel lymph node biopsy and axillary dissection in breast cancer: results in a large series. J Natl Cancer Inst. 1999; 91:368–73.
Article20. Noguchi M, Bando E, Tsugawa K, Miwa K, Yokoyama K, Nakajima K, et al. Staging efficacy of breast cancer with sentinel lymphadenectomy. Breast Cancer Res Treat. 1999; 57:221–9.
Article21. Canavese G, Gipponi M, Catturich A, Di Somma C, Vecchio C, Rosato F, et al. Sentinel lymph node mapping opens a new perspective in the surgical management of early-stage breast cancer: a combined approach with vital blue dye lymphatic mapping and radioguided surgery. Semin Surg Oncol. 1998; 15:272–7.
Article22. McLaughlin SA, Ochoa-Frongia LM, Patil SM, Cody HS 3rd, Sclafani LM. Influence of frozen-section analysis of sentinel lymph node and lumpectomy margin status on reoperation rates in patients undergoing breast-conservation therapy. J Am Coll Surg. 2008; 206:76–82.
Article23. Pamilo M, Soiva M, Lavast EM. Real-time ultrasound, axillary mammography, and clinical examination in the detection of axillary lymph node metastases in breast cancer patients. J Ultrasound Med. 1989; 8:115–20.
Article24. Nori J, Vanzi E, Bazzocchi M, Bufalini FN, Distante V, Branconi F, et al. Role of axillary ultrasound examination in the selection of breast cancer patients for sentinel node biopsy. Am J Surg. 2007; 193:16–20.
Article25. Lee MC, Eatrides J, Chau A, Han G, Kiluk JV, Khakpour N, et al. Consequences of axillary ultrasound in patients with T2 or greater invasive breast cancers. Ann Surg Oncol. 2011; 18:72–7.
Article26. March DE, Wechsler RJ, Kurtz AB, Rosenberg AL, Needleman L. CT-pathologic correlation of axillary lymph nodes in breast carcinoma. J Comput Assist Tomogr. 1991; 15:440–4.
Article27. Peare R, Staff RT, Heys SD. The use of FDG-PET in assessing axillary lymph node status in breast cancer: a systematic review and meta-analysis of the literature. Breast Cancer Res Treat. 2010; 123:281–90.
Article28. Kvistad KA, Rydland J, Smethurst HB, Lundgren S, Fjosne HE, Haraldseth O. Axillary lymph node metastases in breast cancer: preoperative detection with dynamic contrast-enhanced MRI. Eur Radiol. 2000; 10:1464–71.
Article29. Yoshimura G, Sakurai T, Oura S, Suzuma T, Tamaki T, Umemura T, et al. Evaluation of axillary lymph node status in breast cancer with MRI. Breast Cancer. 1999; 6:249–58.
Article30. Houssami N, Ciatto S, Turner RM, Cody HS 3rd, Macaskill P. Preoperative ultrasound-guided needle biopsy of axillary nodes in invasive breast cancer: meta-analysis of its accuracy and utility in staging the axilla. Ann Surg. 2011; 254:243–51.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Number of Removed Lymph Nodes for an Acceptable False Negative Rate in Sentinel Lymph Node Biopsy for Breast Cancer
- Clinical Significance of Rotter's Nodes in Patients with Breast Carcinomas
- Optimized Criteria for Sentinel Lymph Node Biopsy in Patients with Clinically Node Negative Breast Cancer
- Use of Mammary Lymphoscintigraphy and Intraoperative Radioguided Gamma Probe in Sentinel Lymph Node Biopsy of Breast Cancer
- Clinical Significance of Rotter's Nodes in Patients with Breast Carcinomas