J Breast Cancer.
2011 Sep;14(3):198-203.
The Role of Lymphovascular Invasion as a Prognostic Factor in Patients with Lymph Node-Positive Operable Invasive Breast Cancer
- Affiliations
-
- 1Department of Surgery, Chonnam National University Medical School, Gwangju, Korea. mhpark@chonnam.ac.kr
Abstract
- PURPOSE
Lymphovascular invasion (LVI) is an important prognostic factor in patients with lymph node-negative patients with invasive breast cancer. However, the prognostic value of LVI it is unclear and controversial about its prognostic value in patients with lymph node-positive breast cancer patients. So, we report the an analysis of the prognostic significance of LVI in a large cohort study of patients with lymph node-positive patients with invasive breast cancer.
METHODS
We retrospectively reviewed 967 patients with invasive breast cancer that had undergone surgical treatment at our hospital, from January 2004 to December 2007. Among these thempatients, 349 patients with lymph node-positive breast cancer patients are were included in this study. We evaluated clinical and pathological data in these patients, we compared with 5-year overall survival and disease-free survival between an LVI-present group and an LVI-absent group.
RESULTS
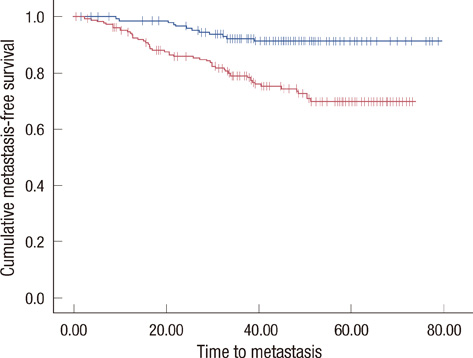
The median follow-up was 48 months (range, 12-78 months), and the mean age of the patients was 48 years (range, 23-78 years). LVI was present in 192 patients (55%) of with tumors and was associated with age < or =40 years (p=0.009), high histologichistological grade (p=0.007), estrogen receptor status (p=0.001), tumor size > or =2 cm (p<0.001), and number of involved lymph nodes (p<0.001), but not with progesterone receptor status, HER2 status, p53 status, or tumor multiplicity. LVI was a significant independent prognostic factor for disease-free survival (p<0.001) and overall survival (p=0.006). By multivariate analysis revealed that LVI (p=0.003), number of involved lymph nodes (> or =4; p=0.005), and high histological grade (II and III; p=0.02) was were an independent significant predictors of disease-free survival and overall survival in the whole group of patients.
CONCLUSION
In this case, we demonstrated that LVI is a significant predictor of poor prognosis in patients with lymph node-positive patients with primary invasive breast cancer, LVI is a significant predictive predictor value of poor prognosis. So, LVI should be considered in the therapeutic strategy as a decision making tool in the adjuvant chemotherapy setting.
MeSH Terms
Figure
Reference
-
1. Clark GM. Harris JR, Lippman ME, Morrow M, Osborne CK, editors. Prognostic and predictive factors. Diseases of the Breast. 2000. 2nd ed. Philadelphia: Lippincott Williams & Wilkins;489–514.2. Woo CS, Silberman H, Nakamura SK, Ye W, Sposto R, Colburn W, et al. Lymph node status combined with lymphovascular invasion creates a more powerful tool for predicting outcome in patients with invasive breast cancer. Am J Surg. 2002. 184:337–340.
Article3. Davis BW, Gelber R, Goldhirsch A, Hartmann WH, Hollaway L, Russell I, et al. Prognostic significance of peritumoral vessel invasion in clinical trials of adjuvant therapy for breast cancer with axillary lymph node metastasis. Hum Pathol. 1985. 16:1212–1218.
Article4. Page DL, Anderson TJ, Connelly JL, Schnitt SF. Page DL, Anderson TJ, editors. Miscellaneous features of carcinoma. Diagnostic Histopathology of the Breast. 1987. Edinburgh: Churchill Livingstone;283–284.5. Fisher B, Bauer M, Wickerham DL, Redmond CK, Fisher ER, Cruz AB, et al. Relation of number of positive axillary nodes to the prognosis of patients with primary breast cancer. An NSABP update. Cancer. 1983. 52:1551–1557.
Article6. Rosai J, Sobin LH, editors. Tumors of the Mammary Gland. 1993. Washington, DC: Armed Forces Institute of Pathology.7. de Mascarel I, MacGrogan G, Debled M, Sierankowski G, Brouste V, Mathoulin-Pthoulin- S, et al. D2-40 in breast cancer: should we detect more vascular emboli? Mod Pathol. 2009. 22:216–222.
Article8. de Mascarel I, Bonichon F, Durand M, Mauriac L, MacGrogan G, Soubeyran I, et al. Obvious peritumoral emboli: an elusive prognostic factor reappraised. Multivariate analysis of 1320 node-negative breast cancers. Eur J Cancer. 1998. 34:58–65.
Article9. Yildirim E, Berberoglu U. Lymph node ratio is more valuable than level III involvement for prediction of outcome in node-positive breast carcinoma patients. World J Surg. 2007. 31:276–289.
Article10. Colleoni M, Rotmensz N, Maisonneuve P, Sonzogni A, Pruneri G, Casadio C, et al. Prognostic role of the extent of peritumoral vascular invasion in operable breast cancer. Ann Oncol. 2007. 18:1632–1640.
Article11. MacGrogan G, Desrousseaux M, de Mascarel I. Prognostic value of Mib1 in a tissue microarray of 855 invasive breast carcinomas. 2006. 4:In : 5th European Breast Cancer Conference; Abstract #261.12. Truong PT, Berthelet E, Lee J, Kader HA, Olivotto IA. The prognostic significance of the percentage of positive/dissected axillary lymph nodes in breast cancer recurrence and survival in patients with one to three positive axillary lymph nodes. Cancer. 2005. 103:2006–2014.
Article13. Rosen PP. Tumor emboli in intramammary lymphatics in breast carcinoma: pathologic criteria for diagnosis and clinical significance. Pathol Annu. 1983. 18 Pt 2:215–232.14. McCready DR, Chapman JA, Hanna WM, Kahn HJ, Murray D, Fish EB, et al. Factors affecting distant disease-free survival for primary invasive breast cancer: use of a log-normal survival model. Ann Surg Oncol. 2000. 7:416–426.
Article15. Mohammed RA, Martin SG, Gill MS, Green AR, Paish EC, Ellis IO. Improved methods of detection of lymphovascular invasion demonstrate that it is the predominant method of vascular invasion in breast cancer and has important clinical consequences. Am J Surg Pathol. 2007. 31:1825–1833.
Article16. Sun Y, Goodison S, Li J, Liu L, Farmerie W. Improved breast cancer prognosis through the combination of clinical and genetic markers. Bioinformatics. 2007. 23:30–37.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictive Factors Affecting Axillary Lymph Node Metastasis in Patients with Invasive Breast Carcinoma of 1 cm or Less
- Prognostic Significance of Peritumoral Vascular Invasion in Patients with Invasive Breast Cancer
- Factors related with Axillary Lymph Nodes Metastases in T1 invasive ductal carcinomas of the Breast
- Prognostic Significance of Immunohistochemical Expression of p53 Gene Product in Operable Breast Cancer
- Clinical Features of Breast Cancer without Axillary Lymph Node Metastasis