Prog Med Phys.
2017 Sep;28(3):100-105. 10.14316/pmp.2017.28.3.100.
Fabrication of a Patient-Customized Helmet with a Three-Dimensional Printer for Radiation Therapy of Scalp
- Affiliations
-
- 1Department of Radiation Oncology, Yeungnam University Medical Center, Daegu, Korea. yjw1160@ynu.ac.kr
- 2Gyeongnam Science High School, Jinju, Korea.
- KMID: 2393370
- DOI: http://doi.org/10.14316/pmp.2017.28.3.100
Abstract
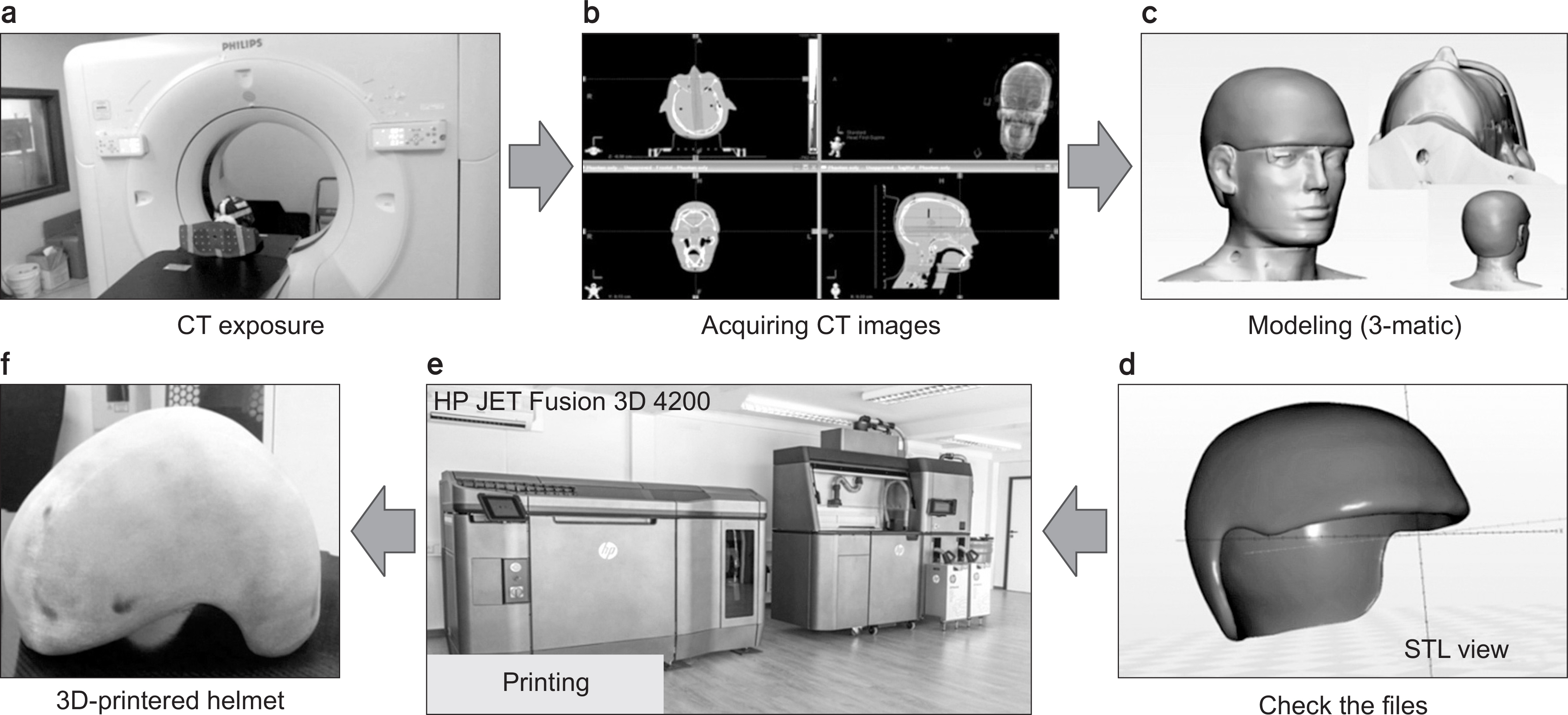
- The purpose of the present study was to develop and evaluate patient-customized helmets with a three-dimensional (3D) printer for radiation therapy of malignant scalp tumors. Computed tomography was performed in a case an Alderson RANDO phantom without bolus (Non_Bolus), in a case with a dental wax bolus on the scalp (Wax_Bolus), and in a case with a patient-customized helmet fabricated using a 3D printer (3D Printing_Bolus); treatment plans for each of the 3 cases were compared. When wax bolus was used to fabricate a bolus, a drier was used to apply heat to the bolus to make the helmet. 3-matic® (Materialise) was used for modeling and polyamide 12 (PA-12) was used as a material, 3D Printing bolus was fabricated using a HP JET Fusion 3D 4200. The average Hounsfield Unit (HU) for the Wax_Bolus was −100, and that of the 3D Printing_Bolus was −10. The average radiation doses to the normal brain with the Non_Bolus, Wax_Bolus, and 3D Printing_Bolus methods were 36.3%, 40.2%, and 36.9%, and the minimum radiation dose were 0.9%, 1.6%, 1.4%, respectively. The organs at risk dose were not significantly difference. However, the 95% radiation doses into the planning target volume (PTV) were 61.85%, 94.53%, and 97.82%, and the minimum doses were 0%, 77.1%, and 82.8%, respectively. The technique used to fabricate patient-customized helmets with a 3D printer for radiation therapy of malignant scalp tumors is highly useful, and is expected to accurately deliver doses by reducing the air gap between the patient and bolus.
MeSH Terms
Figure
Reference
-
1. Ostheimer C, Hübsch P, Janich M, Gerlach R, Vordermark D. Dosimetric comparison of intensity-modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT) in total scalp irradiation: a single institutional experience. Radiat Oncol J. 2016; 34:313.
Article2. Fujimoto K, Shiinoki T, Yuasa Y, Hanazawa H, Shibuya K. Efficacy of patient-specific bolus created using three-dimensional printing technique in photon radiotherapy. Phys Med. 2017; 38:1–9.
Article3. Wojcicka JB, Lasher DE, McAfee SS, Fortier GA. Dosimetric comparison of three different treatment techniques in extensive scalp lesion irradiation. Radiother Oncol. 2009; 91:255–60.
Article4. Sponseller P, Paravathaneni U. A case study of radiotherapy planning for intensity modulation radiation therapy for the whole scalp with matching electron treatment. Med Dosim. 2013; 38:122–4.
Article5. Song JH, Jung J-Y, Park H-W, et al. Dosimetric comparison of three different treatment modalities for total scalp irradiation: the conventional lateral photon-electron technique, helical tomotherapy, and volumetric-modulated arc therapy. J Rad Res. 2014; 56:717–26.
Article6. Vyas V, Palmer L, Mudge R, et al. On bolus for megavoltage photon and electron radiation therapy. Med Dosim. 2013; 38:268–73.
Article7. Song YM, Kim JS, Hong CS, Ju SG, Park JY, Park SY. Comparison of three different helmet bolus device for total scalp irradiation. J Korean Soc Rad Ther. 2012; 24:7.8. Bush K, Gagne I, Zavgorodni S, Ansbacher W, Beckham W. Dosimetric validation of Acuros® XB with Monte Carlo methods for photon dose calculations. Med Phys. 2011; 38:2208–21.9. Oh SA, Yea JW, Kang MK, Park JW, Kim SK. Analysis of the setup uncertainty and margin of the daily exactrac 6D image guide system for patients with brain tumors. PloS One. 2016; 11:e0151709.
Article10. Oh SA, Kang MK, Kim SK, Yea JW. Comparison of IMRT and VMAT techniques in spine stereotactic radiosurgery with international spine radiosurgery consortium consensus guidelines. Prog Med Phys. 2013; 24:145–53.
Article11. Yea JW, Park JW, Kim SK, et al. Feasibility of a 3D-printed anthropomorphic patient-specific head phantom for patient-specific quality assurance of intensity-modulated radiotherapy. PloS One. 2017; 12:e0181560.
Article12. Park JW, Oh SA, Yea JW, Kang MK. Fabrication of malleable three-dimensional-printed customized bolus using three-dimensional scanner. PloS One. 2017; 12:e0177562.
Article13. http://h20195.www2.hp.com/v2/GetDocument.aspx?docname=4AA6-4892EEP
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Angiosarcoma of the Scalp: A Case Report and the Radiotherapy Technique
- Optimal microcatheter shaping method customized for a patient-specific vessel using a three-dimensional printer
- Efficacy and Accuracy of Patient Specific Customize Bolus Using a 3-Dimensional Printer for Electron Beam Therapy
- Outcome Analysis of Cranial Molding Therapy in Nonsynostotic Plagiocephaly
- A Simple Evaluation Method Using a "Sun-Wukong's Headband" Wire for Positional Plagiocephaly Correction after Cranial Remodeling Helmet Therapy