J Korean Ophthalmol Soc.
2017 Oct;58(10):1145-1154. 10.3341/jkos.2017.58.10.1145.
Anatomical Characteristics of End-stage Exudative Age-related Macular Degeneration Refractory to Intravitreal Anti-vascular Endothelial Growth Factor Injection
- Affiliations
-
- 1Department of Ophthalmology, Daegu Fatima Hospital, Daegu, Korea. mjmom99@naver.com
- KMID: 2393166
- DOI: http://doi.org/10.3341/jkos.2017.58.10.1145
Abstract
- PURPOSE
To analyze the anatomical characteristics on spectral-domain optical coherence tomography (SD-OCT) of patients who are legally blind (less than 20/1,000) due to end-stage exudative age-related macular degeneration (AMD) that does not require intravitreal anti-vascular endothelial growth factor (anti-VEGF) injection.
METHODS
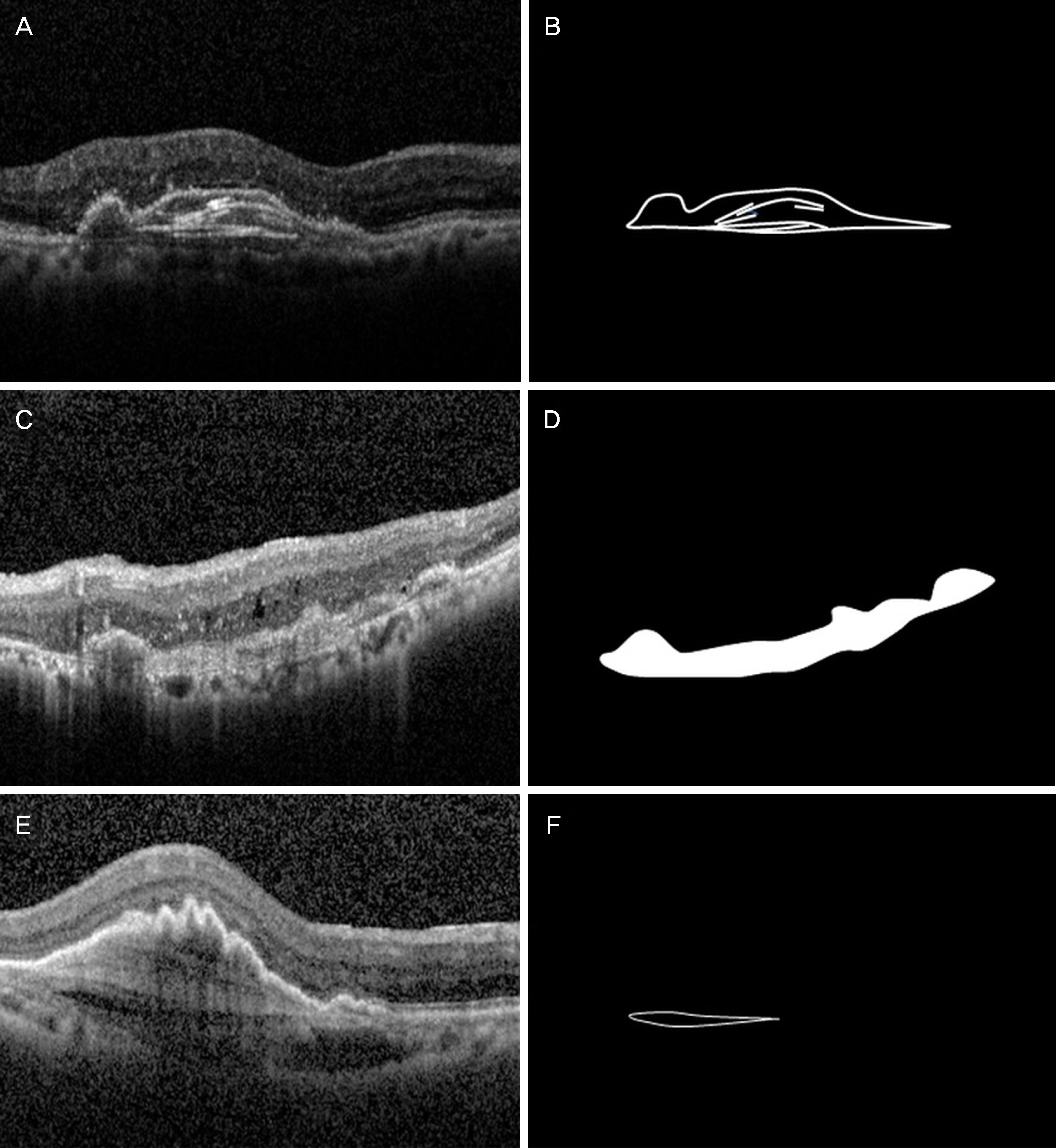
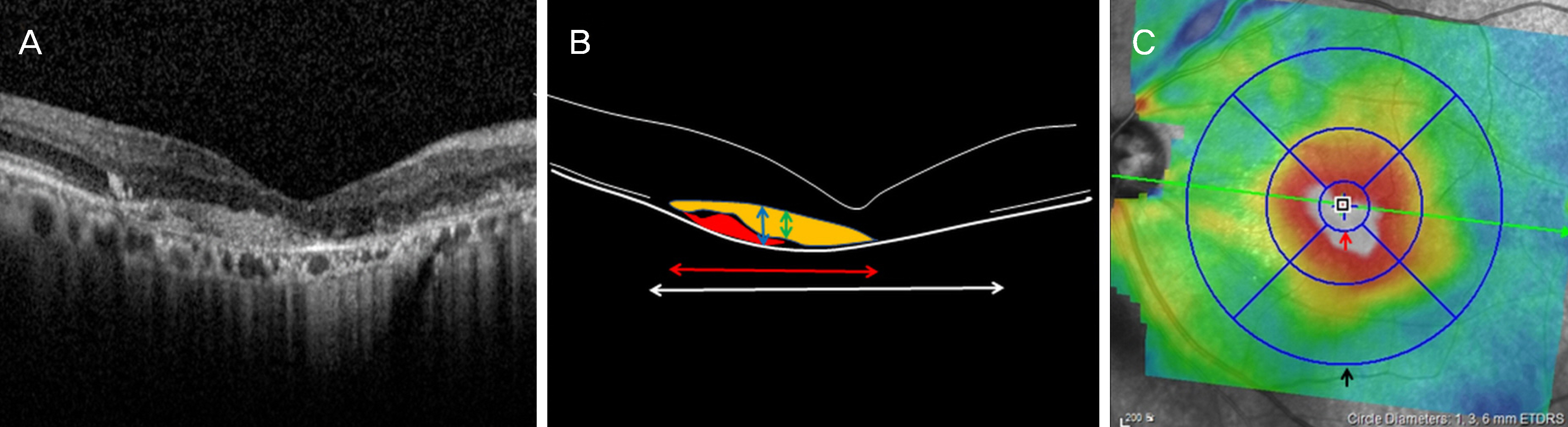
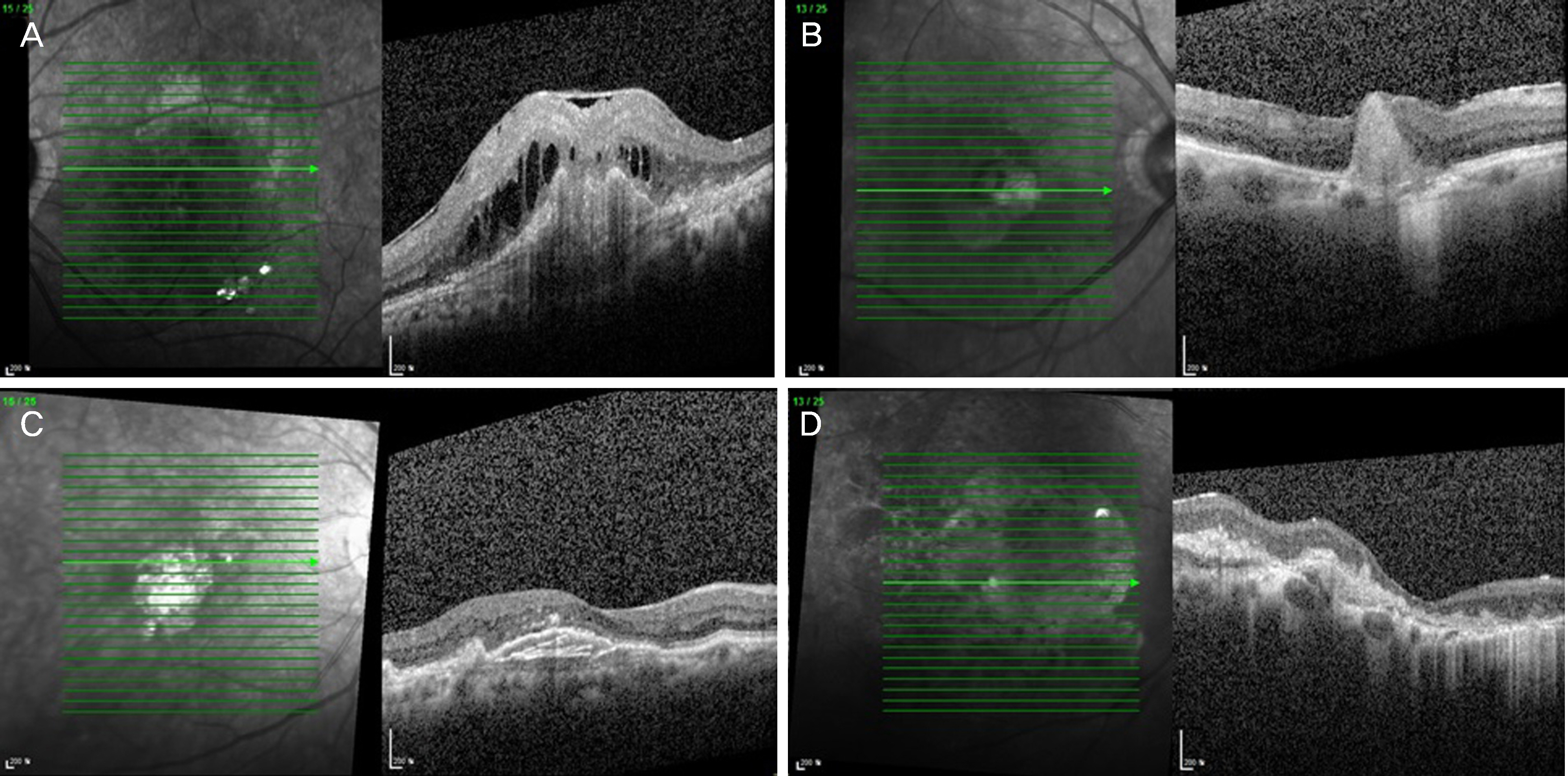
After anti-VEGF injections (active group), 120 eyes of 103 exudative AMD patients experienced visual acuity improved by at least 2 lines or improvement on SD-OCT. In addition, 55 eyes of 54 end-stage exudative AMD patients who did not respond to treatment or who were legally blind due to foveal scar at the first visit (end-stage group) were evaluated retrospectively. Changes in retinal structures of the 2 groups were analyzed by SD-OCT at the last visit.
RESULTS
The mean age of the end-stage group was about 5 years older than the active group. During the follow-up period, subretinal hemorrhage, intraretinal hemorrhage and retinal pigment epithelium tear occurred more frequently in the end-stage group than in the active group (p < 0.05). Intra-retinal fluids and subretinal fluids were more frequently administered in the active group than in the end-stage group, and thick subretinal hyper-reflective materials (SRHRM), fibrovascular pigment epithelial detachment (PED) and extensive inner segment/outer segment (IS/OS) line disruption were observed in all eyes of the end-stage group. The size and thickness of PED, foveal thickness and SRHRM thickness were significantly larger in the end-stage group than in the active group (p < 0.05). Disciform retinal scars were eventually formed in most of the end-stage group.
CONCLUSIONS
In end-stage exudative AMD, the presence of retinal hemorrhage and retinal pigment epithelium tear during follow-up, or the findings of thick SRHRM, fibrovascular PED, and extensive IS/OS line disruption on SD-OCT suggest weak expected effect of intravitreal anti-VEGF injection, which can act as a reference for determining the timing of treatment termination.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Wong TY, Chakravarthy U, Klein R, et al. The natural history and prognosis of neovascular age-related macular degeneration: a abdominalic review of the literature and meta-analysis. Ophthalmology. 2008; 115:116–26.2. Sunness JS, Gonzalez-Baron J, Applegate CA, et al. Enlargement of atrophy and visual acuity loss in the geographic atrophy form of age-related macular degeneration. Ophthalmology. 1999; 106:1768–79.
Article3. Pauleikhoff D. Neovascular age-related macular degeneration: abdominal history and treatment outcomes. Retina. 2005; 25:1065–84.4. Bressler SB. Introduction: understanding the role of angiogenesis and anti-angiogenic agents in age-related macular degeneration. Ophthalmology. 2009; 116(10 Suppl):S1–7.
Article5. Witmer AN, Vrensen GF, Van Noorden CJ, Schlingemann RO. Vascular endothelial growth factors and angiogenesis in eye disease. Prog Retin Eye Res. 2003; 22:1–29.
Article6. Green WR, Enger C. Age-related macular degeneration abdominal studies. The 1992 Lorenz E. Zimmerman Lecture. Ophthalmology. 1993; 100:1519–35.7. Wilgus TA, Ferreira AM, Oberyszyn TM, et al. Regulation of scar formation by vascular endothelial growth factor. Lab Invest. 2000; 8:579–90.
Article8. Michels S, Rosenfeld PJ, Puliafito CA, et al. Systemic abdominal (Avastin) therapy for neovascular age-related macular degeneration twelve-week results of an uncontrolled open-label clinical study. Ophthalmology. 2005; 112:1035–47.9. Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006; 355:1419–31.
Article10. Brown DM, Kaiser PK, Michels M, et al. Ranibizumab versus abdominal for neovascular age-related macular degeneration. N Engl J Med. 2006; 355:1432–44.11. Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006; 355:1419–31.
Article12. Fung AE, Lalwani GA, Rosenfeld PJ, et al. An optical coherence tomography-guided, variable dosing regimen with intravitreal abdominal (Lucentis) for neovascular age-related macular degeneration. Am J Ophthalmol. 2007; 143:566–83.13. Gupta OP, Shienbaum G, Patel AH, et al. A treat and extend abdominal using ranibizumab for neovascular age-related macular abdominal clinical and economic impact. Ophthalmology. 2010; 117:2134–40.14. Cohen SY, Oubraham H, Uzzan J, et al. Causes of unsuccessful abdominal treatment in exudative age-related macular abdominal in clinical settings. Retina. 2012; 32:1480–5.15. Daniel E, Toth CA, Grunwald JE, et al. Risk of scar in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2014; 121:656–66.
Article16. Rahimy E, Freund KB, Larsen M, et al. Multilayered pigment abdominal detachment in neovascular age-related macular degeneration. Retina. 2014; 34:1289–95.17. Cho SW, Bae JH, Song SJ. Anatomical non-responder to intravitreal bevacizumab for neovascular age-related macular degeneration. J Korean Ophthalmol Soc. 2010; 51:1464–70.
Article18. Shin JY, Woo SJ, Ahn J, Park KH. Anti-VEGF-refractory abdominal age-related macular degeneration: differential response abdominal to features on optical coherence tomography. J Korean Ophthalmol. 2013; 27:425–32.19. Varshney N, Jain A, Chan V, et al. Anti-VEGF response in macular hemorrhage and incidence of retinal pigment epithelial tears. Can J Ophthamol. 2013; 48:210–5.
Article20. Empeslidis T, Vardarinos A, Konidaris V, et al. Incidence of retinal pigment epithelial tears and associated risk factors after treatment of age-related macular degeneration with intravitreal Anti-VEGF Injections. Open Ophthalmol J. 2014; 8:101–4.
Article21. Gutfleisch M, Heimes B, Schumacher M, et al. abdominal visual outcome of pigment epithelial tears in association with anti-VEGF therapy of pigment epithelial detachment in AMD. Eye (Lond). 2011; 25:1181–6.22. Durkin SR, Farmer LD, Kulasekara S, Gilhotra J. Change in vision after retinal pigment epithelium tear following the use of an-ti-VEGF therapy for age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2016; 254:1–6.
Article23. Jaffe GJ, Martin DF, Toth CA, et al. Comparison of Age-related Macular Degeneration Treatments Trials Research Group. Macular morphology and visual acuity in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2013; 120:1860–70.24. Golbaz I, Ahlers C, Stock G, et al. Quantification of the therapeutic response of intraretinal, subretinal, and subpigment epithelial com-partments in exudative AMD during anti-VEGF therapy. Invest Ophthalmol Vis Sci. 2011; 52:1599–605.
Article25. Simader C, Ritter M, Bolz M, et al. Morphologic parameters relevant for visual outcome during anti-angiogenic therapy of neovascular age-related macular degeneration. Ophthalmology. 2014; 121:1237–45.
Article26. Ores R, Puche N, Querques G, et al. Gray abdominal subretinal exudative lesions in exudative age-related macular degeneration. Am J Ophthalmol. 2014; 158:354–61.27. Shah VP, Shah SA, Mrejen S, Freund KB. Subretinal abdominal exudation associated with neovascular age-related abdominal degeneration. Retina. 2014; 34:1281–8.28. Tan ACS, Simhaee D, Balaratnasignam C, et al. A perspective on the nature and frequency of pigment epithelial detachments. Am J Ophthalmol. 2016; 172:13–27.
Article29. Kim SY, Sadda S, Pearlman J, et al. Morphometric analysis of the macula in eyes with disciform age-related macular degeneration. Retina. 2002; 22:471–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Exudative Age-Related Macular Degeneration
- Intravitreal injection of anti-vascular endothelial growth factor for patients with various retinal diseases
- Peripapillary Choroidal Thickness Change of Polypoidal Choroidal Vasculopathy after Anti-vascular Endothelial Growth Factor
- Intravitreal Anti-vascular Endothelial Growth Factor for Typical Exudative Age-related Macular Degeneration in Eyes with Good Baseline Visual Acuity
- The Effect of Intravitreal Bevacizumab Injection in Wet Age-Related Macular Degeneration Patients with Cataract Surgery