Korean J Gastroenterol.
2017 Oct;70(4):198-201. 10.4166/kjg.2017.70.4.198.
A Case of Hypertensive Crisis without a Surge in Adrenal Hormones after Radiofrequency Ablation as a Treatment for Primary Hepatocellular Carcinoma
- Affiliations
-
- 1Department of Internal Medicine, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea. rshdrryu@hanmail.net
- KMID: 2392916
- DOI: http://doi.org/10.4166/kjg.2017.70.4.198
Abstract
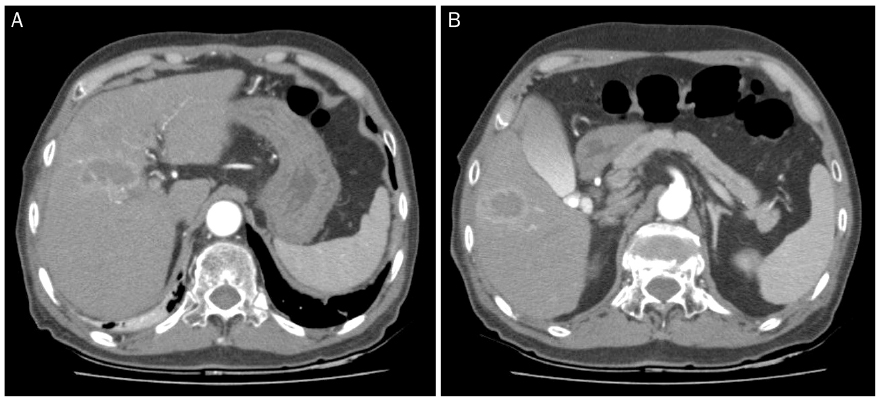
- Radiofrequency ablation (RFA) is a minimally invasive procedure that has been considered as a relatively safe treatment for patients with small hepatocellular carcinoma (HCC). However, RFA has been shown to be associated with complications including mechanical and thermal damage. A 74-year-old man with hepatitis C virus-associated HCC was admitted to our hospital. Abdominal computed tomography revealed two lobulated-HCC in segments 4 and 5. He had no medical history of hypertension and cardiac disease. During RFA, blood pressure was elevated to 200/140 mmHg. There was no evidence of pulmonary embolism, aortic dissection, or ischemic heart disease. Laboratory findings for catecholamine surge were all within normal limits. After continuous intravenous nitroglycerin and oral beta-blocker treatment, patient's blood pressure gradually decreased and back within the normal range. Hypertensive crisis after RFA treatment for HCC is rare. Most reported cases of hypertensive crisis during RFA were related to adrenal gland injury with a release of catecholamine. In our case, the site of HCC was not close to the adrenal gland, and there was no evidence of catecholamine surge. Herein, we report a very rare case of hypertensive crisis without a surge in adrenal hormones after RFA treatment for HCC.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Percutaneous Adrenal Radiofrequency Ablation: A Short Review for Endocrinologists
Byung Kwan Park
Endocrinol Metab. 2020;35(4):750-755. doi: 10.3803/EnM.2020.880.
Reference
-
1. Zhou L, Rui JA, Wang SB, et al. Outcomes and prognostic factors of cirrhotic patients with hepatocellular carcinoma after radical major hepatectomy. World J Surg. 2007; 31:1782–1787.2. McGhana JP, Dodd GD 3rd. Radiofrequency ablation of the liver: current status. AJR Am J Roentgenol. 2001; 176:3–16.3. Mazzanti R, Arena U, Pantaleo P, et al. Survival and prognostic factors in patients with hepatocellular carcinoma treated by percutaneous ethanol injection: a 10-year experience. Can J Gastroenterol. 2004; 18:611–618.4. Vogl TJ, Zangos S, Balzer JO, et al. Transarterial chemoembolization (TACE) in hepatocellular carcinoma: technique, indication and results. Rofo. 2007; 179:1113–1126.5. Curley SA, Marra P, Beaty K, et al. Early and late complications after radiofrequency ablation of malignant liver tumors in 608 patients. Ann Surg. 2004; 239:450–458.6. Chen TM, Huang PT, Lin LF, Tung JN. Major complications of ultrasound-guided percutaneous radiofrequency ablations for liver malignancies: single center experience. J Gastroenterol Hepatol. 2008; 23(8 Pt 2):e445–e450.7. Zavaglia C, Corso R, Rampoldi A, et al. Is percutaneous radiofrequency thermal ablation of hepatocellular carcinoma a safe procedure? Eur J Gastroenterol Hepatol. 2008; 20:196–201.8. Jansen MC, van Duijnhoven FH, van Hillegersberg R, et al. Adverse effects of radiofrequency ablation of liver tumours in the Netherlands. Br J Surg. 2005; 92:1248–1254.9. Onik G, Onik C, Medary I, et al. Life-threatening hypertensive crises in two patients undergoing hepatic radiofrequency ablation. AJR Am J Roentgenol. 2003; 181:495–497.10. Varon J, Marik PE. The diagnosis and management of hypertensive crises. Chest. 2000; 118:214–227.11. Rhim H, Goldberg SN, Dodd GD 3rd, et al. Essential techniques for successful radio-frequency thermal ablation of malignant hepatic tumors. Radiographics. 2001; 21 Spec No:S17–S35. discussion S36-S39.12. Chini EN, Brown MJ, Farrell MA, Charboneau JW. Hypertensive crisis in a patient undergoing percutaneous radiofrequency ablation of an adrenal mass under general anesthesia. Anesth Analg. 2004; 99:1867–1869. table of contents.13. Keeling AN, Sabharwal T, Allen MJ, Hegarty NJ, Adam A. Hypertensive crisis during radiofrequency ablation of the adrenal gland. J Vasc Interv Radiol. 2009; 20:990–991.14. You Z, Deng Y, Shrestha A, Li F, Cheng N. Primary malignant hepatic paraganglioma mimicking liver tumor: a case report. Oncol Lett. 2015; 10:1176–1178.15. Abboud I, Lerolle N, Urien S, et al. Pharmacokinetics of epinephrine in patients with septic shock: modelization and interaction with endogenous neurohormonal status. Crit Care. 2009; 13:R120.16. Beloeil H, Mazoit JX, Benhamou D, Duranteau J. Norepinephrine kinetics and dynamics in septic shock and trauma patients. Br J Anaesth. 2005; 95:782–788.17. Dekkers T, Deinum J, Schultzekool LJ, et al. Plasma metanephrine for assessing the selectivity of adrenal venous sampling. Hypertension. 2013; 62:1152–1157.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypertensive crisis during percutaneous radiofrequency ablation of a metastatic adrenal tumor under general anesthesia: A case report
- Chemoembolization combined with radiofrequency ablation is the best option for the local treatment of early hepatocellular carcinoma?
- Microwave thermosphere versus radiofrequency ablation for hepatocellular carcinoma: Are we approaching the time to end the debate?
- A Metastatic Adrenal Tumor from a Hepatocellular Carcinoma: Combination Therapy with Transarterial Chemoembolization and Radiofrequency Ablation
- The Role of Combination of Transarterial Chemoebolization and Radiofrequency Ablation for Hepatocellular Carcinoma Treatment