Ann Surg Treat Res.
2017 Oct;93(4):181-185. 10.4174/astr.2017.93.4.181.
Effect of intraperitoneal COâ‚‚ concentration on postoperative pain after laparoscopic cholecystectomy
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Soonchunhyang University Cheonan Hospital, Cheonan, Korea. ksjsk@schmc.ac.kr
- 2Department of Surgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- 3Department of Biostatistics, Soonchunhyang University College of Medicine, Seoul, Korea.
- KMID: 2392367
- DOI: http://doi.org/10.4174/astr.2017.93.4.181
Abstract
- PURPOSE
This study set out to identify the association between the intraperitoneal COâ‚‚ concentrations and postoperative pain by dividing the participants into a control group and 2 experimental groups receiving irrigation (1 L and 2 L), and directly measuring their intraperitoneal COâ‚‚ concentrations with a COâ‚‚ gas detector.
METHODS
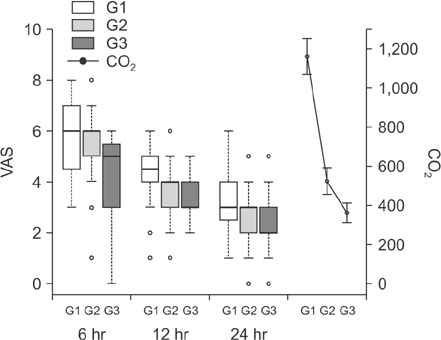
A total of 101 patients, American Society of Anesthesiologists physical status classification I and II patients aged 18-65 years were enrolled in the study. Group 1 did not receive irrigation with normal saline, while groups 2 and 3 were administered irrigation with 1 L and 2 L of normal saline, respectively, after laparoscopic cholecystectomy. Intraperitoneal COâ‚‚ concentrations were measured with a COâ‚‚ gas detector through the port, and postoperative pain was assessed on a visual analogue scale at 6, 12, and 24 hours after surgery.
RESULTS
The intraperitoneal COâ‚‚ concentrations were 1,016.0 ± 960.3 ppm in group 1, 524.5 ± 383.2 ppm in group 2, and 362.2 ± 293.6 ppm in group 3, showing significantly lower concentrations in groups 2 and 3. Postoperative pain was significantly lower in group 3 at 6 hours after surgery, and in groups 2 and 3 at 12 hours after the surgery. However, there was no significant difference between the 3 groups in postoperative pain 24 hours after the surgery.
CONCLUSION
This study found a causal relationship between the amount of normal saline used for irrigation and the intraperitoneal COâ‚‚ concentrations in that irrigation with normal saline reduces pain on the day of the surgery.
Keyword
Figure
Reference
-
1. Hendolin HI, Paakonen ME, Alhava EM, Tarvainen R, Kemppinen T, Lahtinen P. Laparoscopic or open cholecystectomy: a prospective randomised trial to compare postoperative pain, pulmonary function, and stress response. Eur J Surg. 2000; 166:394–399.2. Youn GW, Whang SI, Shin JH. 15 Years of experience in laparoscopic cholecystectomy by a single surgeon. J Korean Surg Soc. 2009; 76:173–178.3. Morsy KM, Abdalla EE. Postoperative pain relief after laparoscopic cholecystectomy: intraperitoneal lidocaine versus nalbuphine. Ain-Shams J Anaesthesiol. 2014; 7:40–44.4. Alexander JI, Hull MG. Abdominal pain after laparoscopy: the value of a gas drain. Br J Obstet Gynaecol. 1987; 94:267–269.5. Bala I, Bhatia N, Mishra P, Verma GR, Kaman L. Comparison of preoperative oral acetazolamide and intraperitoneal normal saline irrigation for reduction of postoperative pain after laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2015; 25:285–290.6. Sarli L, Costi R, Sansebastiano G, Trivelli M, Roncoroni L. Prospective randomized trial of low-pressure pneumoperitoneum for reduction of shoulder-tip pain following laparoscopy. Br J Surg. 2000; 87:1161–1165.7. Dexter SP, Vucevic M, Gibson J, McMahon MJ. Hemodynamic consequences of high- and low-pressure capnoperitoneum during laparoscopic cholecystectomy. Surg Endosc. 1999; 13:376–381.8. Chundrigar T, Hedges AR, Morris R, Stamatakis JD. Intraperitoneal bupivacaine for effective pain relief after laparoscopic cholecystectomy. Ann R Coll Surg Engl. 1993; 75:437–439.9. Madsen MR, Jensen KE. Postoperative pain and nausea after laparoscopic cholecystectomy. Surg Laparosc Endosc. 1992; 2:303–305.10. Moiniche S, Jorgensen H, Wetterslev J, Dahl JB. Local anesthetic infiltration for postoperative pain relief after laparoscopy: a qualitative and quantitative systematic review of intraperitoneal, portsite infiltration and mesosalpinx block. Anesth Analg. 2000; 90:899–912.11. Barczynski M, Herman RM. Low-pressure pneumoperitoneum combined with intraperitoneal saline washout for reduction of pain after laparoscopic cholecystectomy: a prospective randomized study. Surg Endosc. 2004; 18:1368–1373.12. Pappas-Gogos G, Tsimogiannis KE, Zikos N, Nikas K, Manataki A, Tsimoyiannis EC. Preincisional and intraperitoneal ropivacaine plus normal saline infusion for postoperative pain relief after laparoscopic cholecystectomy: a randomized double-blind controlled trial. Surg Endosc. 2008; 22:2036–2045.13. Esmat ME, Elsebae MM, Nasr MM, Elsebaie SB. Combined low pressure pneumoperitoneum and intraperitoneal infusion of normal saline for reducing shoulder tip pain following laparoscopic cholecystectomy. World J Surg. 2006; 30:1969–1973.14. Yilmaz H, Arun O, Apiliogullari S, Acar F, Alptekin H, Calisir A, et al. Effect of laparoscopic cholecystectomy techniques on postoperative pain: a prospective randomized study. J Korean Surg Soc. 2013; 85:149–153.15. Tsimoyiannis EC, Siakas P, Tassis A, Lekkas ET, Tzourou H, Kambili M. Intraperitoneal normal saline infusion for postoperative pain after laparoscopic cholecystectomy. World J Surg. 1998; 22:824–828.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Intraperitoneal Lidocaine on Abdominal and Shoulder Pain after a Laparoscopic Cholecystectomy
- The Topical Intraperitoneal Anesthesia of 0.5% Bupivacaine Before Laparoscopic Cholecystectomy is Effective on the Postoperative Pain Control
- Effects of Preoperative Dexamethasone on Postoperative Pain after Laparoscopic Cholecystectomy
- Comparison of Laparoscopic Cholecystectomy and Minilaparotomy Cholecystectomy
- Pain after a Laparoscopic Cholecystectomy: Comparison between Somatic Pain and Visceral Pain