J Clin Neurol.
2017 Oct;13(4):351-358. 10.3988/jcn.2017.13.4.351.
Perioperative Stroke, In-Hospital Mortality, and Postoperative Morbidity Following Transcatheter Aortic Valve Implantation: A Nationwide Study
- Affiliations
-
- 1Department of Neurological Surgery, University of Pittsburgh, Pittsburgh, PA, USA. thirumalapd@upmc.edu
- 2Department of Neurology, University of Pittsburgh, Pittsburgh, PA, USA.
- 3Department of Cardiology, University of Pittsburgh, Pittsburgh, PA, USA.
- 4Saints Heart and Vascular Institute, St. Anthony Hospital, Oklahoma City, OK, USA.
- 5Division of Cardiac Surgery, Department of Cardiothoracic Surgery, University of Pittsburgh, Pittsburgh, PA, USA.
- KMID: 2392130
- DOI: http://doi.org/10.3988/jcn.2017.13.4.351
Abstract
- BACKGROUND AND PURPOSE
Perioperative stroke is a significant complication of transcatheter aortic valve implantation (TAVI). This study aimed to quantify perioperative stroke as an independent risk factor for in-hospital mortality and postoperative morbidity in patients receiving TAVI.
METHODS
A retrospective cohort study was conducted using the National Inpatient Sample. Patients undergoing TAVI during 2012 and 2013 were identified using diagnostic codes of International Classification of Diseases, ninth revision. Univariate and multivariate analyses were performed using patient demographics and comorbidities to identify predictors of mortality and morbidity, defined by a length of stay of >14 days and/or discharge to a place other than home.
RESULTS
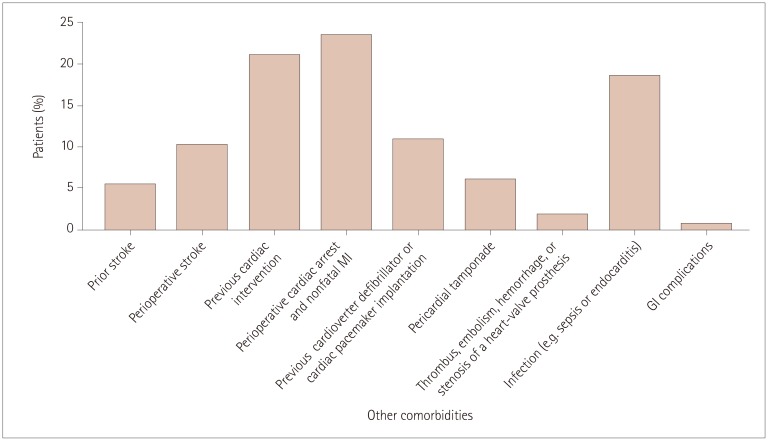
Data were obtained from 7,556 patients undergoing TAVI during 2012 and 2013. The incidence rates of mortality and morbidity were 4.57 and 71.12%, respectively. Perioperative stroke was an independent risk factor for mortality [odds ratio (OR)=3.182, 95% confidence interval (CI)=1.530-6.618, p=0.002], as were infection (OR=17.899, 95% CI=9.876-32.440, p<0.001) and pericardial tamponade (OR=7.272, 95% CI=2.874-18.402, p<0.001). Stroke also predicted morbidity (OR=5.223, 95% CI=2.005-13.608, p=0.001), which was also associated with age, being female, being Asian, moderate and high Van Walraven scores (VWR), and infection.
CONCLUSIONS
In conclusion, perioperative stroke was found to be independently associated with in-hospital mortality and postoperative morbidity, as are age and high VWR. Our findings support the use of further preoperative, intraoperative, and postoperative management strategies during TAVI.
MeSH Terms
Figure
Reference
-
1. Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016; 374:1609–1620. PMID: 27040324.2. Arnold SV, Reynolds MR, Lei Y, Magnuson EA, Kirtane AJ, Kodali SK, et al. Predictors of poor outcomes after transcatheter aortic valve replacement: results from the PARTNER (Placement of Aortic Transcatheter Valve) trial. Circulation. 2014; 129:2682–2690. PMID: 24958751.3. Rodés-Cabau J, Webb JG, Cheung A, Ye J, Dumont E, Osten M, et al. Long-term outcomes after transcatheter aortic valve implantation: insights on prognostic factors and valve durability from the Canadian multicenter experience. J Am Coll Cardiol. 2012; 60:1864–1875. PMID: 23062535.4. Lansky AJ, Schofer J, Tchetche D, Stella P, Pietras CG, Parise H, et al. A prospective randomized evaluation of the TriGuard™ HDH embolic DEFLECTion device during transcatheter aortic valve implantation: results from the DEFLECT III trial. Eur Heart J. 2015; 36:2070–2078. PMID: 25990342.
Article5. Jones BM, Tuzcu EM, Krishnaswamy A, Kapadia SR. Neurologic events after transcatheter aortic valve replacement. Interv Cardiol Clin. 2015; 4:83–93. PMID: 28582124.
Article6. Tchetche D, Farah B, Misuraca L, Pierri A, Vahdat O, Lereun C, et al. Cerebrovascular events post-transcatheter aortic valve replacement in a large cohort of patients: a FRANCE-2 registry substudy. JACC Cardiovasc Interv. 2014; 7:1138–1145. PMID: 25240554.7. Reynolds MR, Lei Y, Wang K, Chinnakondepalli K, Vilain KA, Magnuson EA, et al. Cost-effectiveness of transcatheter aortic valve replacement with a self-expanding prosthesis versus surgical aortic valve replacement. J Am Coll Cardiol. 2016; 67:29–38. PMID: 26764063.8. Ailawadi G, LaPar DJ, Speir AM, Ghanta RK, Yarboro LT, Crosby IK, et al. Contemporary costs associated with transcatheter aortic valve replacement: a propensity-matched cost analysis. Ann Thorac Surg. 2016; 101:154–160. discussion 160. PMID: 26409710.9. Dua A, Romanelli M, Upchurch GR Jr, Pan J, Hood D, Hodgson KJ, et al. Predictors of poor outcome after carotid intervention. J Vasc Surg. 2016; 64:663–670. PMID: 27209401.
Article10. Walsh JA 3rd, Teirstein PS, Stinis C, Price MJ. Risk assessment in patient selection for transcatheter aortic valve replacement. Interv Cardiol Clin. 2015; 4:1–12. PMID: 28582117.
Article11. Nwachuku EL, Balzer JR, Yabes JG, Habeych ME, Crammond DJ, Thirumala PD. Diagnostic value of somatosensory evoked potential changes during carotid endarterectomy: a systematic review and meta-analysis. JAMA Neurol. 2015; 72:73–80. PMID: 25383418.12. Thirumala PD, Thiagarajan K, Gedela S, Crammond DJ, Balzer JR. Diagnostic accuracy of EEG changes during carotid endarterectomy in predicting perioperative strokes. J Clin Neurosci. 2016; 25:1–9. PMID: 26474501.
Article13. Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011; 365:993–1003. PMID: 21899409.14. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998; 36:8–27. PMID: 9431328.
Article15. Saia F, Latib A, Ciuca C, Gasparetto V, Napodano M, Sticchi A, et al. Causes and timing of death during long-term follow-up after transcatheter aortic valve replacement. Am Heart J. 2014; 168:798–806. PMID: 25440810.
Article16. Xiong TY, Liao YB, Zhao ZG, Xu YN, Wei X, Zuo ZL, et al. Causes of death following transcatheter aortic valve replacement: a systematic review and meta-analysis. J Am Heart Assoc. 2015; 4:e002096. PMID: 26391132.
Article17. The Society of Thoracic Surgeons (US). Online STS adult cardiac surgery risk calculator [Internet]. Chicago (IL): The Society of Thoracic Surgeons;2007. cited 2016 Jul 7. Available from: http://riskcalc.sts.org/stswebriskcalc/#/.18. HCUP Elixhauser Comorbidity Software. Healthcare Cost and Utilization Project (HCUP) [Internet]. Rockville (MD): Agency for Healthcare Research and Quality;2017. cited 2016 June 6. Available from: http://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp.19. HCUP Databases (US). Healthcare Cost and Utilization Project (HCUP) [Internet]. Rockville (MD): Agency for Healthcare Research and Quality;2017. cited 2016 Jun 6. Available from: http://www.hcup-us.ahrq.gov/nisoverview.jsp.20. Jilaihawi H, Chakravarty T, Weiss RE, Fontana GP, Forrester J, Makkar RR. Meta-analysis of complications in aortic valve replacement: comparison of Medtronic-Corevalve, Edwards-Sapien and surgical aortic valve replacement in 8,536 patients. Catheter Cardiovasc Interv. 2012; 80:128–138. PMID: 22415849.
Article21. Patel HJ, Likosky DS, Pruitt AL, Murphy ET, Theurer PF, Prager RL. Aortic valve replacement in the moderately elevated risk patient: a population-based analysis of outcomes. Ann Thorac Surg. 2016; 102:1466–1472. PMID: 27324524.
Article22. Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010; 363:1597–1607. PMID: 20961243.
Article23. Tamburino C, Capodanno D, Ramondo A, Petronio AS, Ettori F, Santoro G, et al. Incidence and predictors of early and late mortality after transcatheter aortic valve implantation in 663 patients with severe aortic stenosis. Circulation. 2011; 123:299–308. PMID: 21220731.
Article24. Stortecky S, Windecker S, Pilgrim T, Heg D, Buellesfeld L, Khattab AA, et al. Cerebrovascular accidents complicating transcatheter aortic valve implantation: frequency, timing and impact on outcomes. Euro-Intervention. 2012; 8:62–70. PMID: 22580250.
Article25. Chaturvedi S, Sacco RL. Are the current risks of asymptomatic carotid stenosis exaggerated?: further evidence supporting the CREST 2 trial. JAMA Neurol. 2015; 72:1233–1234. PMID: 26390399.26. Arrowsmith JE, Ganugapenta MS. Intraoperative brain monitoring in cardiac surgery. In : Bonser RS, Pagano D, Haverich A, editors. Brain Protection in Cardiac Surgery. Vol. 1. London: Springer-Verlag London;2011. p. 83–111.27. Thirumala PD, Muluk S, Udesh R, Mehta A, Schindler J, Mulukutla S, et al. Carotid artery disease and periprocedural stroke risk after transcatheter aortic valve implantation. Ann Card Anaesth. 2017; 20:145–151. PMID: 28393772.
Article28. Kleiman NS, Maini BJ, Reardon MJ, Conte J, Katz S, Rajagopal V, et al. Neurological events following transcatheter aortic valve replacement and their predictors: a report from the CoreValve trials. Circ Cardiovasc Interv. 2016; 9:e003551. PMID: 27601429.29. Adams DH, Popma JJ, Reardon MJ, Yakubov SJ, Coselli JS, Deeb GM, et al. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med. 2014; 370:1790–1798. PMID: 24678937.
Article30. Hemmann K, Sirotina M, De Rosa S, Ehrlich JR, Fox H, Weber J, et al. The STS score is the strongest predictor of long-term survival following transcatheter aortic valve implantation, whereas access route (transapical versus transfemoral) has no predictive value beyond the periprocedural phase. Interact Cardiovasc Thorac Surg. 2013; 17:359–364. PMID: 23644728.
Article31. Mandava P, Kent TA. A method to determine stroke trial success using multidimensional pooled control functions. Stroke. 2009; 40:1803–1810. PMID: 19286598.
Article32. König IR, Ziegler A, Bluhmki E, Hacke W, Bath PM, Sacco RL, et al. Predicting long-term outcome after acute ischemic stroke: a simple index works in patients from controlled clinical trials. Stroke. 2008; 39:1821–1826. PMID: 18403738.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Severe Aortic Stenosis Patient With High Operative Risk Treated by Transcatheter Aortic-Valve Implantation
- Recent updates in transcatheter aortic valve implantation
- Expanding transcatheter aortic valve replacement into uncharted indications
- Right anterior mini-thoracotomy aortic valve replacement versus transcatheter aortic valve implantation in octogenarians: a single-center retrospective study
- Similar Morphology, but Different Function: Acute Improvement of Myocardial Longitudinal Strain after Percutaneous Transcatheter Aortic Valve Implantation Therapy in a Severe Aortic Stenosis Patient