J Gastric Cancer.
2015 Dec;15(4):262-269. 10.5230/jgc.2015.15.4.262.
Nomogram Estimating the Probability of Intraabdominal Abscesses after Gastrectomy in Patients with Gastric Cancer
- Affiliations
-
- 1Gastric Cancer Branch, Research Institute and Hospital, National Cancer Center, Goyang, Korea. gskim@ncc.re.kr
- 2Biometric Research Branch, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
- KMID: 2391561
- DOI: http://doi.org/10.5230/jgc.2015.15.4.262
Abstract
- PURPOSE
Intraabdominal abscess is one of the most common reasons for re-hospitalization after gastrectomy. This study aimed to develop a model for estimating the probability of intraabdominal abscesses that can be used during the postoperative period.
MATERIALS AND METHODS
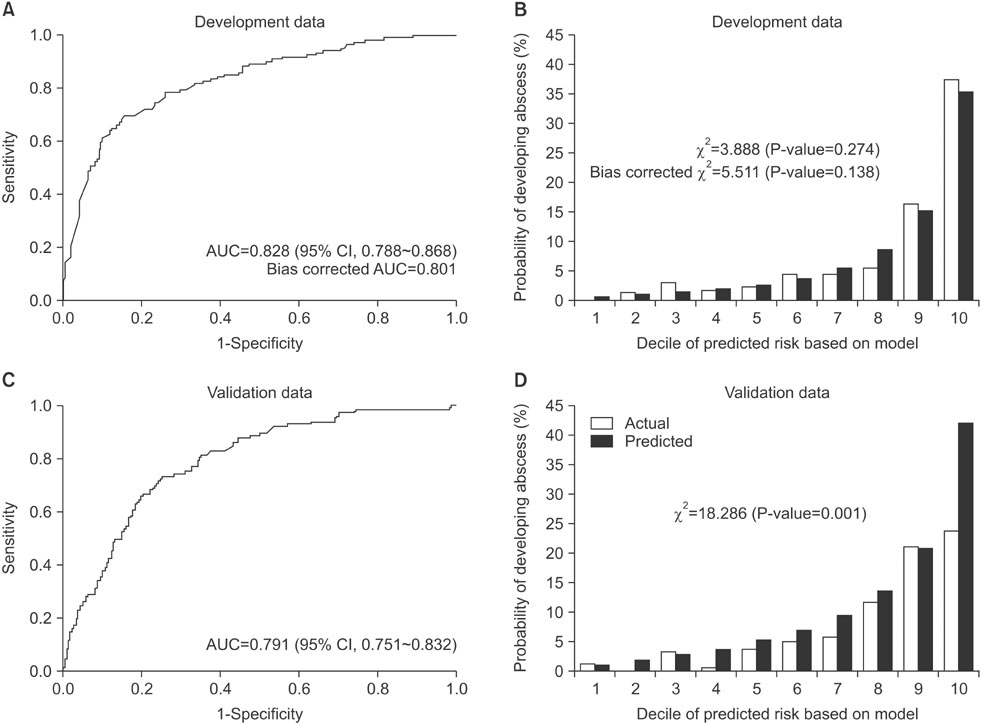
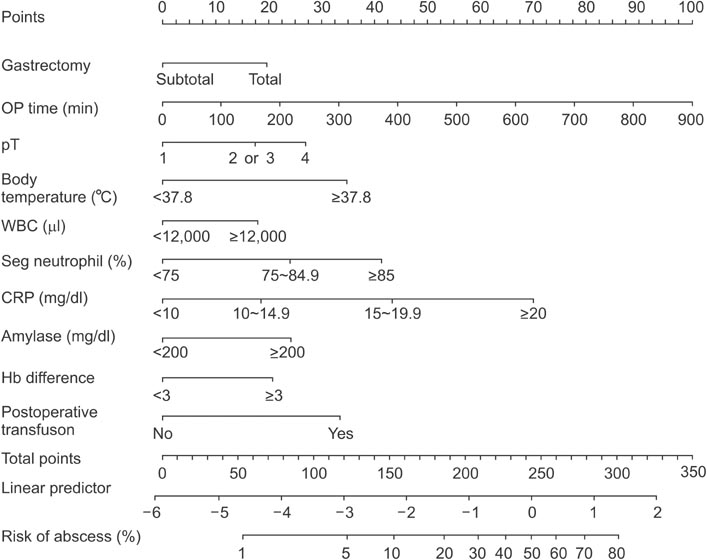
We retrospectively reviewed the clinicopathological data of 1,564 patients who underwent gastrectomy for gastric cancer between 2010 and 2012. Twenty-six related markers were analyzed, and multivariate logistic regression analysis was used to develop the probability estimation model for intraabdominal abscess. Internal validation using a bootstrap approach was employed to correct for bias, and the model was then validated using an independent dataset comprising of patients who underwent gastrectomy between January 2008 and March 2010. Discrimination and calibration abilities were checked in both datasets.
RESULTS
The incidence of intraabdominal abscess in the development set was 7.80% (122/1,564). The surgical approach, operating time, pathologic N classification, body temperature, white blood cell count, C-reactive protein level, glucose level, and change in the hemoglobin level were significant predictors of intraabdominal abscess in the multivariate analysis. The probability estimation model that was developed on the basis of these results showed good discrimination and calibration abilities (concordance index=0.828, Hosmer-Lemeshow chi-statistic P=0.274). Finally, we combined both datasets to produce a nomogram that estimates the probability of intraabdominal abscess.
CONCLUSIONS
This nomogram can be useful for identifying patients at a high risk of intraabdominal abscess. Patients at a high risk may benefit from further evaluation or treatment before discharge.
MeSH Terms
-
Abdominal Abscess
Abscess*
Bias (Epidemiology)
Body Temperature
C-Reactive Protein
Calibration
Classification
Dataset
Discrimination (Psychology)
Gastrectomy*
Glucose
Humans
Incidence
Leukocyte Count
Logistic Models
Multivariate Analysis
Nomograms*
Postoperative Complications
Postoperative Period
Retrospective Studies
Stomach Neoplasms*
C-Reactive Protein
Glucose
Figure
Reference
-
1. Bonenkamp JJ, Songun I, Hermans J, Sasako M, Welvaart K, Plukker JT, et al. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet. 1995; 345:745–748.2. Cuschieri A, Fayers P, Fielding J, Craven J, Bancewicz J, Joypaul V, et al. The Surgical Cooperative Group. Postoperative morbidity and mortality after D1 and D2 resections for gastric cancer: preliminary results of the MRC randomised controlled surgical trial. Lancet. 1996; 347:995–999.3. Sano T, Sasako M, Yamamoto S, Nashimoto A, Kurita A, Hiratsuka M, et al. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy: Japan Clinical Oncology Group study 9501. J Clin Oncol. 2004; 22:2767–2773.4. Zilberstein B, Martins BC, Jacob CE, Bresciani C, Lopasso FP, de Cleva R, et al. Complications of gastrectomy with lymphadenectomy in gastric cancer. Gastric Cancer. 2004; 7:254–259.5. Ryu KW, Kim YW, Lee JH, Nam BH, Kook MC, Choi IJ, et al. Surgical complications and the risk factors of laparoscopy-assisted distal gastrectomy in early gastric cancer. Ann Surg Oncol. 2008; 15:1625–1631.6. Ahn CW, Hur H, Han SU, Cho YK. Comparison of intracorporeal reconstruction after laparoscopic distal gastrectomy with extracorporeal reconstruction in the view of learning curve. J Gastric Cancer. 2013; 13:34–43.7. Kim KM, An JY, Kim HI, Cheong JH, Hyung WJ, Noh SH. Major early complications following open, laparoscopic and robotic gastrectomy. Br J Surg. 2012; 99:1681–1687.8. Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU, Kim W, et al. Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report: a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg. 2010; 251:417–420.9. Kim YW, Yoon HM, Eom BW, Park JY. History of minimally invasive surgery for gastric cancer in Korea. J Gastric Cancer. 2012; 12:13–17.10. Wu CW, Hsiung CA, Lo SS, Hsieh MC, Shia LT, Whang-Peng J. Randomized clinical trial of morbidity after D1 and D3 surgery for gastric cancer. Br J Surg. 2004; 91:283–287.11. Tang J, Humes DJ, Gemmil E, Welch NT, Parsons SL, Catton JA. Reduction in length of stay for patients undergoing oesophageal and gastric resections with implementation of enhanced recovery packages. Ann R Coll Surg Engl. 2013; 95:323–328.12. Grantcharov TP, Kehlet H. Laparoscopic gastric surgery in an enhanced recovery programme. Br J Surg. 2010; 97:1547–1551.13. So JB, Lim ZL, Lin HA, Ti TK. Reduction of hospital stay and cost after the implementation of a clinical pathway for radical gastrectomy for gastric cancer. Gastric Cancer. 2008; 11:81–85.14. Choi JW, Xuan Y, Hur H, Byun CS, Han SU, Cho YK. Outcomes of critical pathway in laparoscopic and open surgical treatments for gastric cancer patients: patients selection for fast-track program through retrospective analysis. J Gastric Cancer. 2013; 13:98–105.15. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–123.16. Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg. 2009; 250:177–186.17. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC Cancer Staging Handbook. 7th ed. New York: Springer-Verlag;2010.18. Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996; 15:361–387.19. Simon R. Diagnostic and prognostic prediction using gene expression profiles in high-dimensional microarray data. Br J Cancer. 2003; 89:1599–1604.20. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996; 22:707–710.21. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985; 13:818–829.22. Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993; 270:2957–2963.23. Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg. 1991; 78:355–360.24. Wijesinghe LD, Mahmood T, Scott DJ, Berridge DC, Kent PJ, Kester RC. Comparison of POSSUM and the Portsmouth predictor equation for predicting death following vascular surgery. Br J Surg. 1998; 85:209–212.25. Sagar PM, Hartley MN, MacFie J, Taylor BA, Copeland GP. Comparison of individual surgeon's performance. Risk-adjusted analysis with POSSUM scoring system. Dis Colon Rectum. 1996; 39:654–658.26. Neary B, Whitman B, Foy C, Heather BP, Earnshaw JJ. Value of POSSUM physiology scoring to assess outcome after intraarterial thrombolysis for acute leg ischaemia (short note). Br J Surg. 2001; 88:1344–1345.27. Williams DJ, Walker JD. A nomogram to calculate the Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity (POSSUM). Br J Surg. 2014; 101:239–245.28. Hartgrink HH, van de Velde CJ, Putter H, Bonenkamp JJ, Klein Kranenbarg E, Songun I, et al. Extended lymph node dissection for gastric cancer: who may benefit? Final results of the randomized Dutch gastric cancer group trial. J Clin Oncol. 2004; 22:2069–2077.29. Park DJ, Lee HJ, Kim HH, Yang HK, Lee KU, Choe KJ. Predictors of operative morbidity and mortality in gastric cancer surgery. Br J Surg. 2005; 92:1099–1102.30. Seo SH, Hur H, An CW, Yi X, Kim JY, Han SU, et al. Operative risk factors in gastric cancer surgery for elderly patients. J Gastric Cancer. 2011; 11:116–121.31. Lee JH, Park do J, Kim HH, Lee HJ, Yang HK. Comparison of complications after laparoscopy-assisted distal gastrectomy and open distal gastrectomy for gastric cancer using the Clavien-Dindo classification. Surg Endosc. 2012; 26:1287–1295.32. Bozzetti F, Marubini E, Bonfanti G, Miceli R, Piano C, Crose N, et al. The Italian Gastrointestinal Tumor Study Group. Total versus subtotal gastrectomy: surgical morbidity and mortality rates in a multicenter Italian randomized trial. Ann Surg. 1997; 226:613–620.33. Lo CH, Chen JH, Wu CW, Lo SS, Hsieh MC, Lui WY. Risk factors and management of intra-abdominal infection after extended radical gastrectomy. Am J Surg. 2008; 196:741–745.34. Miletic KG, Taylor TN, Martin ET, Vaidya R, Kaye KS. Readmissions after diagnosis of surgical site infection following knee and hip arthroplasty. Infect Control Hosp Epidemiol. 2014; 35:152–157.35. Avritscher EB, Cooksley CD, Rolston KV, Swint JM, Delclos GL, Franzini L, et al. Serious postoperative infections following resection of common solid tumors: outcomes, costs, and impact of hospital surgical volume. Support Care Cancer. 2014; 22:527–535.36. Keller DS, Swendseid B, Khorgami Z, Champagne BJ, Reynolds HL Jr, Stein SL, et al. Predicting the unpredictable: comparing readmitted versus non-readmitted colorectal surgery patients. Am J Surg. 2014; 207:346–351. discussion 350-35137. Tingstedt B, Isaksson J, Andersson R. Long-term follow-up and cost analysis following surgery for small bowel obstruction caused by intra-abdominal adhesions. Br J Surg. 2007; 94:743–748.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robotic Gastrectomy for Gastric Cancer: A Review of Postoperative and Oncologic Outcomes
- External Validation of a Gastric Cancer Nomogram Derived from a Large-volume Center Using Dataset from a Medium-volume Center
- Entirely Laparoscopic Gastrectomy and Colectomy for Remnant Gastric Cancer with Gastric Outlet Obstruction and Transverse Colon Invasion
- Proximal Gastrectomy for Upper-third Early Gastric Cancer
- Intraabdominal abscess mimicking gastric cancer recurrence: a case report