Korean J Crit Care Med.
2017 Aug;32(3):275-283. 10.4266/kjccm.2016.00990.
The Ability of the Acute Physiology and Chronic Health Evaluation (APACHE) IV Score to Predict Mortality in a Single Tertiary Hospital
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Cheongju St. Mary's Hospital, Cheongju, Korea.
- 2Department of Nursing Care, Chungnam National University Hospital, Daejeon, Korea.
- 3Division of Pulmonology and Critical Care Medicine, Department of Internal Medicine, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea.
- 4Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea. diffable@hanmail.net
- 5Clinical Trial Center, Chungnam National University Hospital, Daejeon, Korea.
- 6Division of Pulmonology, Department of Internal Medicine, Chamjoeun Hospital, Gwangju, Korea.
- 7Department of Surgery, Chungbuk National University College of Medicine, Cheongju, Korea.
- KMID: 2391187
- DOI: http://doi.org/10.4266/kjccm.2016.00990
Abstract
- BACKGROUND
The Acute Physiology and Chronic Health Evaluation (APACHE) II model has been widely used in Korea. However, there have been few studies on the APACHE IV model in Korean intensive care units (ICUs). The aim of this study was to compare the ability of APACHE IV and APACHE II in predicting hospital mortality, and to investigate the ability of APACHE IV as a critical care triage criterion.
METHODS
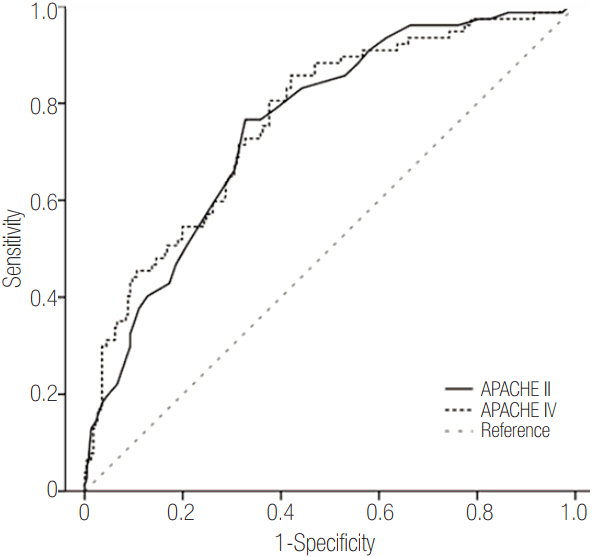
The study was designed as a prospective cohort study. Measurements of discrimination and calibration were performed using the area under the receiver operating characteristic curve (AUROC) and the Hosmer-Lemeshow goodness-of-fit test respectively. We also calculated the standardized mortality ratio (SMR).
RESULTS
The APACHE IV score, the Charlson Comorbidity index (CCI) score, acute respiratory distress syndrome, and unplanned ICU admissions were independently associated with hospital mortality. The calibration, discrimination, and SMR of APACHE IV were good (H = 7.67, P = 0.465; C = 3.42, P = 0.905; AUROC = 0.759; SMR = 1.00). However, the explanatory power of an APACHE IV score >93 alone on hospital mortality was low at 44.1%. The explanatory power was increased to 53.8% when the hospital mortality was predicted using a model that considers APACHE IV >93 scores, medical admission, and risk factors for CCI >3 coincidentally. However, the discriminative ability of the prediction model was unsatisfactory (C index <0.70).
CONCLUSIONS
The APACHE IV presented good discrimination, calibration, and SMR for hospital mortality.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985; 13:818–29.2. Strand K, Flaatten H. Severity scoring in the ICU: a review. Acta Anaesthesiol Scand. 2008; 52:467–78.
Article3. Moreno RP, Metnitz PG, Almeida E, Jordan B, Bauer P, Campos RA, et al. SAPS 3: from evaluation of the patient to evaluation of the intensive care unit. Part 2: development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med. 2005; 31:1345–55.4. Lemeshow S, Teres D, Pastides H, Avrunin JS, Steingrub JS. A method for predicting survival and mortality of ICU patients using objectively derived weights. Crit Care Med. 1985; 13:519–25.
Article5. Caldeira VM, Silva Júnior JM, Oliveira AM, Rezende S, Araújo LA, Santana MR, et al. Criteria for patient admission to an intensive care unit and related mortality rates. Rev Assoc Med Bras (1992). 2010; 56:528–34.6. Zimmerman JE, Kramer AA, McNair DS, Malila FM. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today’s critically ill patients. Crit Care Med. 2006; 34:1297–310.
Article7. Le Gall JR, Loirat P, Alperovitch A, Glaser P, Granthil C, Mathieu D, et al. A simplified acute physiology score for ICU patients. Crit Care Med. 1984; 12:975–7.8. Brinkman S, Bakhshi-Raiez F, Abu-Hanna A, de Jonge E, Bosman RJ, Peelen L, et al. External validation of Acute Physiology and Chronic Health Evaluation IV in Dutch intensive care units and comparison with Acute Physiology and Chronic Health Evaluation II and Simplified Acute Physiology Score II. J Crit Care. 2011; 26:105.e11–8.
Article9. Keegan MT, Gajic O, Afessa B. Comparison of APACHE III, APACHE IV, SAPS 3, and MPM0III and influence of resuscitation status on model performance. Chest. 2012; 142:851–8.
Article10. Nassar Junior AP, Mocelin AO, Andrade FM, Brauer L, Giannini FP, Nunes AL, et al. SAPS 3, APACHE IV or GRACE: which score to choose for acute coronary syndrome patients in intensive care units? Sao Paulo Med J. 2013; 131:173–8.
Article11. Berger MM, Marazzi A, Freeman J, Chioléro R. Evaluation of the consistency of Acute Physiology and Chronic Health Evaluation (APACHE II) scoring in a surgical intensive care unit. Crit Care Med. 1992; 20:1681–7.
Article12. Kim JY, Lim SY, Jeon K, Koh Y, Lim CM, Koh SO, et al. External validation of the Acute Physiology and Chronic Health Evaluation II in Korean intensive care units. Yonsei Med J. 2013; 54:425–31.
Article13. Gupta R, Arora VK. Performance evaluation of APACHE II score for an Indian patient with respiratory problems. Indian J Med Res. 2004; 119:273–82.14. Ludwigs U, Csatlos M, Hulting J. Predicting in-hospital mortality in acute myocardial infarction: impact of thrombolytic therapy on APACHE II performance. Scand Cardiovasc J. 2000; 34:371–6.15. Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, et al. The APACHE III prognostic system: risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991; 100:1619–36.16. Sprung CL, Danis M, Iapichino G, Artigas A, Kesecioglu J, Moreno R, et al. Triage of intensive care patients: identifying agreement and controversy. Intensive Care Med. 2013; 39:1916–24.
Article17. Orsini J, Butala A, Ahmad N, Llosa A, Prajapati R, Fishkin E. Factors influencing triage decisions in patients referred for ICU admission. J Clin Med Res. 2013; 5:343–9.
Article18. Orsini J, Blaak C, Yeh A, Fonseca X, Helm T, Butala A, et al. Triage of patients consulted for ICU admission during times of ICU-bed shortage. J Clin Med Res. 2014; 6:463–8.
Article19. Lee H, Shon YJ, Kim H, Paik H, Park HP. Validation of the APACHE IV model and its comparison with the APACHE II, SAPS 3, and Korean SAPS 3 models for the prediction of hospital mortality in a Korean surgical intensive care unit. Korean J Anesthesiol. 2014; 67:115–22.
Article20. Sedloň P, Kameník L, Škvařil J, Malý M, Táborský M, Zavoral M. Comparison of the accuracy and correctness of mortality estimates for intensive care unit patients in internal clinics of the Czech Republic using APACHE II, APACHE IV, SAPS 3 and MPMoIII models. Med Glas (Zenica). 2016; 13:82–9.21. Salluh JI, Soares M. ICU severity of illness scores: APACHE, SAPS and MPM. Curr Opin Crit Care. 2014; 20:557–65.22. Costa e Silva VT, de Castro I, Liaño F, Muriel A, Rodríguez-Palomares JR, Yu L. Performance of the third-generation models of severity scoring systems (APACHE IV, SAPS 3 and MPM-III) in acute kidney injury critically ill patients. Nephrol Dial Transplant. 2011; 26:3894–901.
Article23. Aminiahidashti H, Bozorgi F, Montazer SH, Baboli M, Firouzian A. Comparison of APACHE II and SAPS II scoring systems in prediction of critically ill patients’ outcome. Emerg (Tehran). 2017; 5:e4.24. Daley J, Jencks S, Draper D, Lenhart G, Thomas N, Walker J. Predicting hospital-associated mortality for Medicare patients: a method for patients with stroke, pneumonia, acute myocardial infarction, and congestive heart failure. JAMA. 1988; 260:3617–24.
Article25. Kopterides P, Liberopoulos P, Ilias I, Anthi A, Pragkastis D, Tsangaris I, et al. General prognostic scores in outcome prediction for cancer patients admitted to the intensive care unit. Am J Crit Care. 2011; 20:56–66.
Article26. Gilani MT, Razavi M, Azad AM. A comparison of Simplified Acute Physiology Score II, Acute Physiology and Chronic Health Evaluation II and Acute Physiology and Chronic Health Evaluation III scoring system in predicting mortality and length of stay at surgical intensive care unit. Niger Med J. 2014; 55:144–7.
Article27. Kramer AA, Higgins TL, Zimmerman JE. Comparison of the Mortality Probability Admission Model III, National Quality Forum, and Acute Physiology and Chronic Health Evaluation IV hospital mortality models: implications for national benchmarking. Crit Care Med. 2014; 42:544–53.28. Juneja D, Singh O, Nasa P, Dang R. Comparison of newer scoring systems with the conventional scoring systems in general intensive care population. Minerva Anestesiol. 2012; 78:194–200.29. Xing X, Gao Y, Wang H, Huang C, Qu S, Zhang H, et al. Performance of three prognostic models in patients with cancer in need of intensive care in a medical center in China. PLoS One. 2015; 10:e0131329.
Article30. Wong RS, Ismail NA, Tan CC. An external independent validation of APACHE IV in a Malaysian intensive care unit. Ann Acad Med Singapore. 2015; 44:127–32.31. Bhattacharyya M, Todi S. APACHE IV: benchmarking in an Indian ICU. Crit Care. 2009; 13(Suppl 1):P510.
Article32. Yamin S, Vaswani AK, Afreedi M. Predictive efficasy of APACHE IV at ICU.s of CHK. Pak J Chest Med. 2011; 17.33. Ayazoglu TA. A comparison of APACHE II and APACHE IV scoring systems in predicting outcome in patients admitted with stroke to an intensive care unit. Anaesth Pain Intensive Care. 2011; 15:7–12.34. Garrouste-Orgeas M, Montuclard L, Timsit JF, Misset B, Christias M, Carlet J. Triaging patients to the ICU: a pilot study of factors influencing admission decisions and patient outcomes. Intensive Care Med. 2003; 29:774–81.
Article35. Adeniji KA, Cusack R. The Simple Triage Scoring System (STSS) successfully predicts mortality and critical care resource utilization in H1N1 pandemic flu: a retrospective analysis. Crit Care. 2011; 15:R39.
Article36. Ho KM, Williams TA, Harahsheh Y, Higgins TL. Using patient admission characteristics alone to predict mortality of critically ill patients: a comparison of 3 prognostic scores. J Crit Care. 2016; 31:21–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Validation of the APACHE IV model and its comparison with the APACHE II, SAPS 3, and Korean SAPS 3 models for the prediction of hospital mortality in a Korean surgical intensive care unit
- Comparison of Predict Mortality Scoring Systems for Spontaneous Intracerebral Hemorrhage Patients
- APACHE II Score and Evaluation of Intensive Care Unit Patients
- Performance of APACHE IV in Medical Intensive Care Unit Patients: Comparisons with APACHE II, SAPS 3, and MPMâ‚€ III
- Validation of APACHE II scoring system at 24 hours after admission as a prognostic tool in urosepsis: A prospective observational study