J Korean Med Sci.
2017 Nov;32(11):1814-1819. 10.3346/jkms.2017.32.11.1814.
Prediction of Post-Endoscopic Retrograde Cholangiopancreatography Pancreatitis Using 4-Hour Post-Endoscopic Retrograde Cholangiopancreatography Serum Amylase and Lipase Levels
- Affiliations
-
- 1Department of Gastroenterology, Ajou University School of Medicine, Suwon, Korea. jinhkim@ajou.ac.kr
- KMID: 2390308
- DOI: http://doi.org/10.3346/jkms.2017.32.11.1814
Abstract
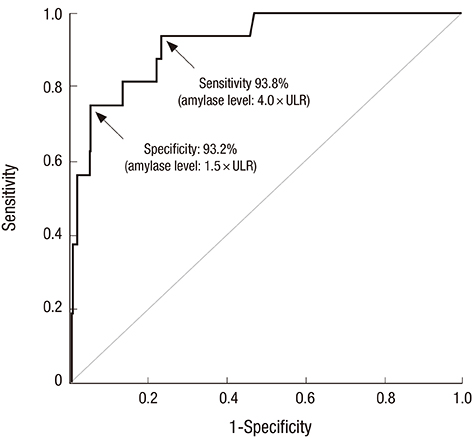
- Early post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis (PEP) prediction may allow safe same-day outpatients discharge after ERCP and earlier proper management. This study aimed to assess the usefulness of the 4-hour post-ERCP serum amylase and lipase levels for PEP early prediction and to investigate predictive cut-off values for 4-hour post-ERCP serum amylase and lipase levels for safe discharge and urgent initiation of resuscitation. The data of 516 consecutive patients with native papilla who underwent ERCP between January 2013 and August 2014 were retrospectively reviewed. Serum amylase and lipase levels were measured before, and 4 and 24 hours after ERCP. PEP occurred in 16 (3.1%) patients. The receiver-operator characteristic curve for 4-hour post-ERCP serum amylase and lipase levels showed that the areas under the curve were 0.919 and 0.933, respectively, demonstrating good test performances as predictors for PEP (both P values < 0.001). The amylase level > 1.5 × the upper limit of reference (ULR) was found useful for PEP exclusion with a sensitivity of 93.8%, while 4 × ULR was found useful to guide preventive therapy with the best specificity of 93.2%. Similarly, the lipase level 2 × ULR showed best sensitivity, while 8 × ULR had the best specificity. Logistic regression analysis showed that 4-hour post-ERCP amylase level > 4 × ULR, lipase level > 8 × ULR, precut sphincterotomy, and pancreatic sphincterotomy were significant predictors for PEP. In conclusion, 4-hour post-ERCP amylase and lipase levels are useful early predictors of PEP that can ensure safe discharge or prompt resuscitation after ERCP.
MeSH Terms
Figure
Reference
-
1. Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, Pilotto A, Forlano R. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007; 102:1781–1788.2. Rustagi T, Jamidar PA. Endoscopic retrograde cholangiopancreatography (ERCP)-related adverse events: post-ERCP pancreatitis. Gastrointest Endosc Clin N Am. 2015; 25:107–121.3. Jeurnink SM, Poley JW, Steyerberg EW, Kuipers EJ, Siersema PD. ERCP as an outpatient treatment: a review. Gastrointest Endosc. 2008; 68:118–123.4. Gottlieb K, Sherman S, Pezzi J, Esber E, Lehman GA. Early recognition of post-ERCP pancreatitis by clinical assessment and serum pancreatic enzymes. Am J Gastroenterol. 1996; 91:1553–1557.5. Testoni PA, Bagnolo F, Caporuscio S, Lella F. Serum amylase measured four hours after endoscopic sphincterotomy is a reliable predictor of postprocedure pancreatitis. Am J Gastroenterol. 1999; 94:1235–1241.6. Testoni PA, Caporuscio S, Bagnolo F, Lella F. Twenty-four-hour serum amylase predicting pancreatic reaction after endoscopic sphincterotomy. Endoscopy. 1999; 31:131–136.7. Thomas PR, Sengupta S. Prediction of pancreatitis following endoscopic retrograde cholangiopancreatography by the 4-h post procedure amylase level. J Gastroenterol Hepatol. 2001; 16:923–926.8. Sutton VR, Hong MK, Thomas PR. Using the 4-hour post-ERCP amylase level to predict post-ERCP pancreatitis. JOP. 2011; 12:372–376.9. Tulassay Z, Papp J, Koranyi L, Szathmari M, Tamas G Jr. Hormonal and biochemical changes following endoscopic retrograde cholangio-pancreatography. Acta Gastroenterol Belg. 1981; 44:538–544.10. Ito K, Fujita N, Noda Y, Kobayashi G, Horaguchi J, Takasawa O, Obana T. Relationship between post-ERCP pancreatitis and the change of serum amylase level after the procedure. World J Gastroenterol. 2007; 13:3855–3860.11. Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991; 37:383–393.12. LaFerla G, Gordon S, Archibald M, Murray WR. Hyperamylasaemia and acute pancreatitis following endoscopic retrograde cholangiopancreatography. Pancreas. 1986; 1:160–163.13. Testoni PA, Bagnolo F. Pain at 24 hours associated with amylase levels greater than 5 times the upper normal limit as the most reliable indicator of post-ERCP pancreatitis. Gastrointest Endosc. 2001; 53:33–39.14. Sultan S, Baillie J. What are the predictors of post-ERCP pancreatitis, and how useful are they? JOP. 2002; 3:188–194.15. Koizumi M, Takada T, Kawarada Y, Hirata K, Mayumi T, Yoshida M, Sekimoto M, Hirota M, Kimura Y, Takeda K, et al. JPN Guidelines for the management of acute pancreatitis: diagnostic criteria for acute pancreatitis. J Hepatobiliary Pancreat Surg. 2006; 13:25–32.16. Lee TH. Diagnosis and treatment of acute pancreatitis. Korean J Med. 2015; 89:494–506.17. Panteghini M, Pagani F, Alebardi O, Lancini G, Cestari R. Time course of changes in pancreatic enzymes, isoenzymes and, isoforms in serum after endoscopic retrograde cholangiopancreatography. Clin Chem. 1991; 37:1602–1605.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevention of Post-endoscopic Retrograde Cholangiopancreatography Pancreatitis: An Endoscopic Perspective
- Clinical Study of Endoscopic Retrograde Cholangiopancreatography (ERCP) Induced Pancreatitis
- Nafamostat for Prophylaxis against Post-Endoscopic Retrograde Cholangiopancreatography Pancreatitis Compared with Gabexate
- Endoscopic retrograde cholangiopancreatography complications: Techniques to reduce risk and management strategies
- Prevention of Postendoscopic Retrograde Cholangiopancreatography Pancreatitis: The Endoscopic Technique