J Korean Ophthalmol Soc.
2017 Sep;58(9):1074-1079. 10.3341/jkos.2017.58.9.1074.
Association between 7-year Changes in Intraocular Pressure and Systemic Factors in Koreans: A Longitudinal Study
- Affiliations
-
- 1Department of Ophthalmology, Konkuk University School of Medicine, Seoul, Korea. bjcho@kuh.ac.kr
- KMID: 2390071
- DOI: http://doi.org/10.3341/jkos.2017.58.9.1074
Abstract
- PURPOSE
To investigate the changes in intraocular pressure (IOP) and associated systemic factors over 7 years in a healthy Korean population.
METHODS
This longitudinal study included healthy subjects with no history of ocular disease and who had been receiving health examinations seven years apart at the Konkuk University Medical Center, Healthcare Center. The participants completed lifestyle questionnaires and underwent general health examinations (blood pressure, height and weight, and blood biochemical tests) and ocular examinations including noncontact tonometry and fundus photography. Subjects with abnormal fundus photography findings and ocular hypertension were excluded. Changes in IOP and systemic factors over 7 years were analyzed.
RESULTS
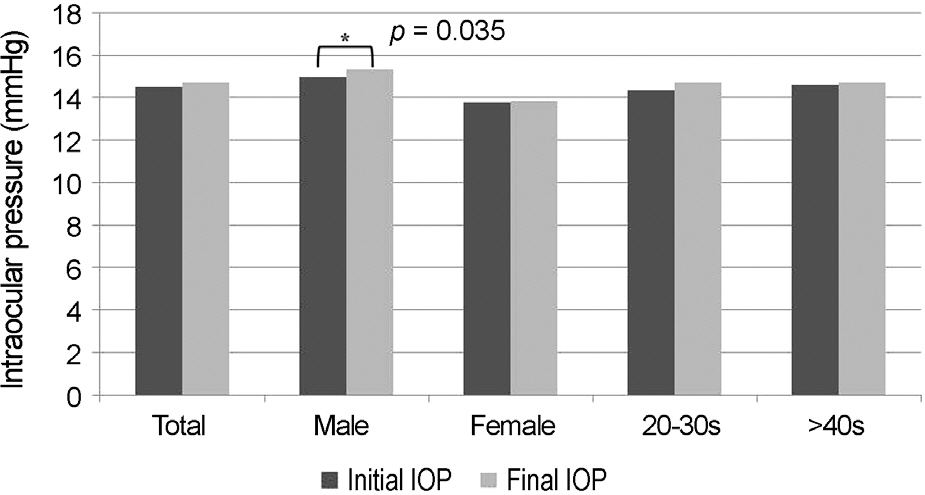
Of 524 possible subjects, 469 were enrolled (55 subjects were excluded: 50 due to abnormal fundus photography and 5 for missing data). The left eye was analyzed in all patients. In all subjects, initial IOP (mean 14.50 ± 3.14 mmHg) was not significantly different from final IOP (14.72 ± 3.38 mmHg) (paired t-test, p = 0.074). In male patients, the final IOP was significantly higher than the initial IOP (paired t-test, p = 0.035). Lifestyle questionnaire variables were associated with a final IOP that was significantly higher than the initial IOP (smokers, alcohol drinkers and less exercisers, paired t-test; p = 0.014, 0.010 and 0.024, respectively). A linear mixed-effects model analysis showed that the change in IOP was negatively associated with age, but this was not statistically significant. Changes in systolic blood pressure (SBP), body mass index (BMI), total cholesterol (T.Chol) and low density lipoprotein (LDL) were positively correlated with change in IOP.
CONCLUSIONS
A linear mixed-model analysis showed IOP decreased with age but this was not statistically significant. Changes in SBP, BMI, T.Chol and LDL were significantly positively correlated with change in IOP.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Mackenzie W. Practical treatise on the diseases of the eye. 2nd ed. London: Longman;1835; 822.2. Dielemans I, Vingerling JR, Wolfs RC. . The prevalence of pri-mary open-angle glaucoma in a population-based study in the Netherlands: the Rotterdam Study. Ophthalmology. 1994; 101:1851–5.3. Carel RS, Korczyn AD, Rock M, Goya I. Association between ocu-lar pressure and certain health parameters. Ophthalmology. 1984; 91:311–4.
Article4. Schulzer M, Drance SM. Intraocular pressure systemic blood pres-sure, and age: a correlational study. Br J Ophthalmol. 1987; 71:245–9.
Article5. Kahn HA, Leibowitz HM, Ganley JP. . The Framingham Eye Study II. Association of ophthalmic pathology with single varia-bles previously measured in the Framingham Heart Study. Am J Epidemiol. 1977; 106:33–41.6. Hollows F, Graham P. Intra-ocular pressure, glaucoma, and glauco-ma suspects in a defined population. Br J Ophthalmol. 1966; 50:570–86.
Article7. Klein BE, Klein R. Intraocular pressure and cardiovascular risk variables. Arch Ophthalmol. 1981; 99:837–9.
Article8. Dielemans I, de Jong PT, Stolk R. . Primary open-angle glauco-ma, intraocular pressure, and diabetes mellitus in the general elderly population: the Rotterdam Study. Ophthalmology. 1996; 103:1271–5.9. Dielemans I, Vingerling JR, Algra D. . Primary open-angle glaucoma, intraocular pressure, and systemic blood pressure in the general elderly population: the Rotterdam Study. Ophthalmology. 1995; 102:54–60.10. Klein B, Klein R, Linton K. Intraocular pressure in an American community. The Beaver Dam Eye Study. Invest Ophthalol Vis Sci. 1992; 33:2224–8.11. Shiose Y. The aging effect on intraocular pressure in an apparently normal population. Arch Ophthalmol. 1984; 102:883–7.
Article12. Kurokawa M. Studies on the normal intraocular pressure. I. The average distribution and difference of both sexes and the aging of the normal intraocular pressure. Nippon Ganka Gakkai Zasshi. 1969; 73:112–22.13. Kashiwagi K, Shibuya T, Tsukahara S. De novo age-related retinal disease and intraocular-pressure changes during a 10-year period in a Japanese adult population. Jpn J Ophalmol. 2005; 49:36–40.
Article14. Baek S, Kee C, Suh W. Longitudinal analysis of age-related changes in intraocular pressure in South Korea. Eye (Lond). 2015; 29:625–9.
Article15. Park SC, Kee C. The effect of age and gender on the intraocular pressure in Koreans: a cross-sectional study. J Korean Ophthalml Soc. 2008; 49:135–42.
Article16. Jung SC, Choi YR, Lee JS. The relationship between intraocular pressure and cardiovascular risk factors. J Korean Ophthalml Soc. 2005; 46:1518–25.17. Lee JS, Kim CM, Choi HY, Oum BS. A relationship between intra-ocular pressure and age and body mass index in a Korean population. J Korean Ophthalml Soc. 44:1559–66.18. McLeod S, West SK, Quigley HA, Fozard J. A longitudinal study of the relationship between intraocular and blood pressures. Invest Ophthalol Vis Sci. 1990; 31:2361–6.19. Mori K, Ando F, Nomura H. . Relationship between intraocular pressure and obesity in Japan. Int J Epidemiol. 2000; 29:661–6.
Article20. Lee JS, Lee SH, Oum BS. . Relationship between intraocular pressure and systemic health parameters in a Korean population. Clin Exp Ophthalmol. 2002; 30:237–41.
Article21. Armaly MF. Age and sex correction of applanation pressure. Arch of Ophthalmol. 1967; 78:480–4.
Article22. Xu L, Li J, Zheng Y. . Intraocular pressure in Northern China in an urban and rural population: the Beijing eye study. Am J Ophthalmol. 2005; 140:913–5.
Article23. Rochtchina E, Mitchell P, Wang JJ. Relationship between age and intraocular pressure: the Blue Mountains Eye Study. Clin Exp Ophthalmol. 2002; 30:173–5.
Article24. Weih LM, Mukesh BN, McCarty CA, Taylor HR. Association of demographic, familial, medical, and ocular factors with intraocular pressure. Arch of Ophthalmol. 2001; 119:875–80.
Article25. Bengtsson B. Some factors affecting the distribution of intraocular pressures in a population. Acta Ophthalmol (Copenh). 1972; 50:33–46.
Article26. Graham PA. Epidemiology of simple glaucoma and ocular hypertension. Br J Ophthalmol. 1972; 56:223–9.
Article27. Armaly MF. On the distribution of applanation pressure: I. Statistical features and the effect of age, sex, and family history of glaucoma. Arch Ophthalmol. 1965; 73:11–8.28. Klein BE, Klein R, Moss SE. Intraocular pressure in diabetic persons. Ophthalmology. 1984; 91:1356–60.
Article29. Nomura H, Shimokata H, Ando F. . Age-related changes in in-traocular pressure in a large japanese population: A cross-sectional and longitudinal study11The authors have no financial interests re-lated to the article. Ophthalmology. 1999; 106:2016–22.30. Nakano T, Tatemichi M, Miura Y. . Long-term physiologic changes of intraocular pressure: a 10-year longitudinal analysis in young and middle-aged Japanese men. Ophthalmology. 2005; 112:609–16.31. Zhao D, Kim MH. . A longitudinal study of age-related changes in intraocular pressure: the Kangbuk Samsung Health Study. Invest Ophthalol Vis Sci. 2014; 55:6244–50.
Article32. Bulpitt C, Hodes C, Everitt M. Intraocular pressure and systemic blood pressure in the elderly. Br J Ophthalmol. 1975; 59:717–20.
Article33. Shiose Y, Kawase Y. A new approach to stratified normal intra-ocular pressure in a general population. Am J ophthalmol. 1986; 101:714–21.
Article34. Koçak I, Orgül S, Saruhan A. . Measurement of intraocular pressure with a modern noncontact tonometer. Ophthalmologica. 1998; 212:81–7.
Article35. Lam AK, Chan R, Lam CH. The validity of a new noncontact ton-ometer and its comparison with the Goldmann tonometer. Optom Vis Sci. 2004; 81:601–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Short Term Effect of Xalatan in Normal Koreans
- A Study on the Intraocular Pressure of Koreans Part 1: The Intraocular Pressure(I.O.P.) of 405 Normal Koreans
- The Association between Intraocular Pressure and Predictors of Coronary Heart Disease Risk in Koreans
- The Effect of Short Term Use of Azopt in Normal Koreans
- The Effect of Age and Gender on the Intraocular Pressure in Koreans: A Cross-sectional Study