J Breast Cancer.
2017 Jun;20(2):183-191. 10.4048/jbc.2017.20.2.183.
Screening Uptake Differences Are Not Implicated in Poorer Breast Cancer Outcomes among Singaporean Malay Women
- Affiliations
-
- 1Department of Radiation Oncology, National Cancer Centre Singapore, Singapore. wong.ru.xin@nccs.com.sg
- KMID: 2389756
- DOI: http://doi.org/10.4048/jbc.2017.20.2.183
Abstract
- PURPOSE
This study was undertaken to examine the impact of screening and race on breast cancer outcomes in Singapore.
METHODS
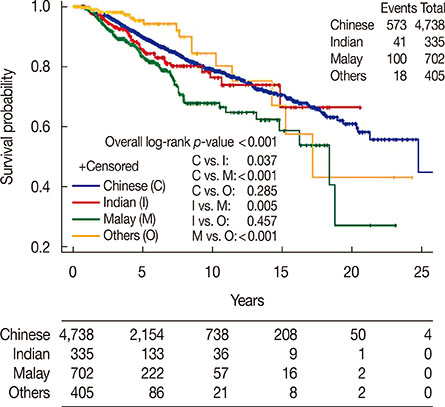
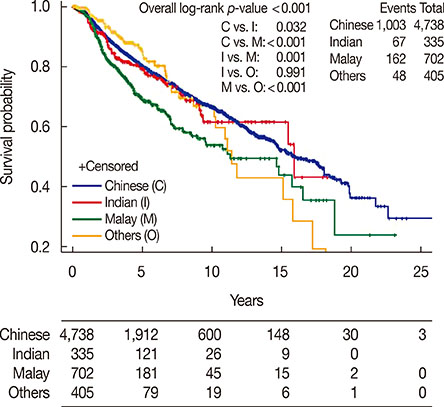
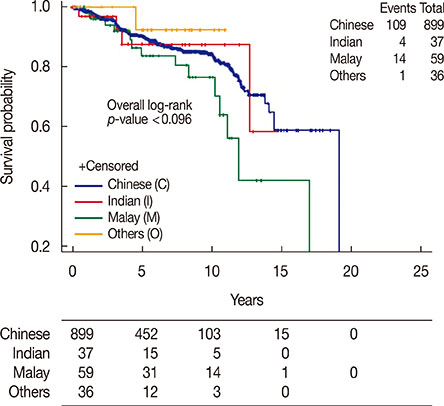
An institutional database was reviewed, and invasive ductal carcinoma (IDC) and ductal carcinoma in situ (DCIS) data were analyzed separately. Overall survival (OS), disease-free survival (DFS), and cancer-specific survival (CSS) were assessed.
RESULTS
The study included 6,180 IDC and 1,031 DCIS patients. The median follow-up time was 4.1 years. Among IDC patients, Malay women were the youngest when first diagnosed, and were more likely to present with advanced stage disease. Malay women also had the highest proportion of T3 and T4 tumors at 14.2%, compared with Chinese women at 8.7% and Indian women at 9.6% (p<0.001). Malay women had a higher incidence of node-positive disease at 58.3% compared with Chinese women at 46.4% and Indian women at 54.9% (p<0.001). Malay subjects also had higher-grade tumors; 61.8% had grade 3 tumors compared with 45.8% of Chinese women and 52% of Indian women (p<0.001). Furthermore, tumors in Malay subjects were less endocrine-sensitive and more human epidermal growth factor receptor 2 enriched. Malay women had the lowest 5- and 10-year OS, DFS, and CSS rates (p<0.001). After separating clinically and screen-detected tumors, multivariate analysis showed that race was still significant for outcomes. For screen-detected tumors, the OS hazard ratio (HR) for Malay women compared to Chinese women was 5.78 (95% confidence interval [CI], 2.64-12.64), the DFS HR was 2.18 (95% CI, 1.19-3.99), and the CSS HR was 5.93 (95% CI, 2.15-16.39). For DCIS, there were no statistically significant differences in the tumor size, grade, histology subtypes, or hormone sensitivity.
CONCLUSION
Malay race is a poor prognostic factor in both clinically and screen-detected IDC. Special attention should be given to the detection and follow-up of breast cancer in this group.
Keyword
MeSH Terms
-
Asian Continental Ancestry Group
Breast Neoplasms*
Breast*
Carcinoma, Ductal
Carcinoma, Intraductal, Noninfiltrating
Continental Population Groups
Disease-Free Survival
Early Detection of Cancer
Ethnic Groups
Female
Follow-Up Studies
Humans
Incidence
Mass Screening*
Multivariate Analysis
Prognosis
Receptor, Epidermal Growth Factor
Singapore
Receptor, Epidermal Growth Factor
Figure
Cited by 1 articles
-
Validation of a Risk Score Incorporating Tumor Characteristics into the American Joint Committee on Cancer Anatomic Stage for Breast Cancer
Yi Heng Seow, Ru Xin Wong, John Heng Chi Lim, Weixiang Lian, Yoon Sim Yap, Fuh Yong Wong
J Breast Cancer. 2019;22(2):260-273. doi: 10.4048/jbc.2019.22.e16.
Reference
-
1. Malay Singaporeans. Wikipedia. Accessed July 17th, 2016. https://en.wikipedia.org/wiki/Malay_Singaporeans#Migration_of_Malays_to_Singapore_after_1819.2. National Registry of Diseases Office. Trends in Cancer Incidence in Singapore 2010-2014, Singapore Cancer Registry Annual Registry Report. Singapore: National Registry of Diseases Office;2015.3. Bhoo-Pathy N, Hartman M, Yip CH, Saxena N, Taib NA, Lim SE, et al. Ethnic differences in survival after breast cancer in South East Asia. PLoS One. 2012; 7:e30995.
Article4. Allgood PC, Duffy SW, Kearins O, O’Sullivan E, Tappenden N, Wallis MG, et al. Explaining the differ-ence in prognosis between screen-detected and symptomatic breast cancers. Br J Cancer. 2011; 104:1680–1685.
Article5. Evans A, Cornford E, James J. Breast screening overdiagnosis: stop treating indolent lesions. BMJ. 2009; 339:b3256.6. Abdullah NA, Wan Mahiyuddin WR, Muhammad NA, Ali ZM, Ibrahim L, Ibrahim Tamim NS, et al. Survival rate of breast cancer patients in Malaysia: a population-based study. Asian Pac J Cancer Prev. 2013; 14:4591–4594.
Article7. Al-Naggar RA, Isa ZM, Shah SA, Nor MI, Chen R, Ismail F, et al. Eight year survival among breast cancer Malaysian women from University Kebangsaan Malaysia Medical Centre. Asian Pac J Cancer Prev. 2009; 10:1075–1078.8. Ibrahim NI, Dahlui M, Aina EN, Al-Sadat N. Who are the breast cancer survivors in Malaysia? Asian Pac J Cancer Prev. 2012; 13:2213–2218.
Article9. Devi CR, Tang TS, Corbex M. Incidence and risk factors for breast cancer subtypes in three distinct South-East Asian ethnic groups: Chinese, Malay and natives of Sarawak, Malaysia. Int J Cancer. 2012; 131:2869–2877.
Article10. Sim HL, Seah M, Tan SM. Breast cancer knowledge and screening practices: a survey of 1,000 Asian women. Singapore Med J. 2009; 50:132–138.11. Anderson KN, Schwab RB, Martinez ME. Reproductive risk factors and breast cancer subtypes: a review of the literature. Breast Cancer Res Treat. 2014; 144:1–10.
Article12. United Kingdom National Case-Control Study Group. Breast feeding and risk of breast cancer in young women. BMJ. 1993; 307:17–20.13. Alvarado M, Ozanne E, Esserman L. Overdiagnosis and overtreatment of breast cancer. Am Soc Clin Oncol Educ Book. 2012; e40–e45.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early screening for breast cancer
- Breast Cancer Screening with MRI
- Temporal Trend in Uptake of the National General Health Checkups and Cancer Screening Program among Korean Women with Breast Cancer
- Trends in breast cancer screening rates among Korean women: results from the Korean National Cancer Screening Survey, 2005-2020
- Medical auditing of whole-breast screening ultrasonography