Neurointervention.
2017 Sep;12(2):125-129. 10.5469/neuroint.2017.12.2.125.
Dementia and Parkinsonism-a Rare Presentation of Intracranial Dural Arteriovenous Fistulae
- Affiliations
-
- 1Department of Imaging Sciences and Interventional Radiology, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, Kerala. India. drmanojg@sctimst.ac.in
- KMID: 2389506
- DOI: http://doi.org/10.5469/neuroint.2017.12.2.125
Abstract
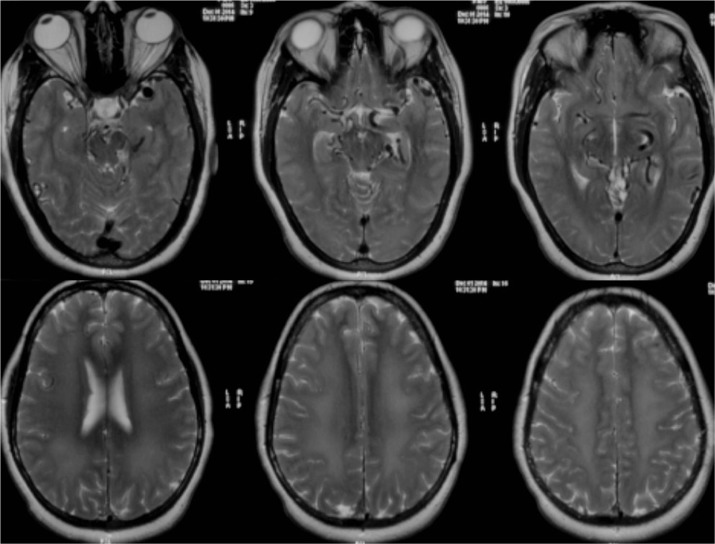
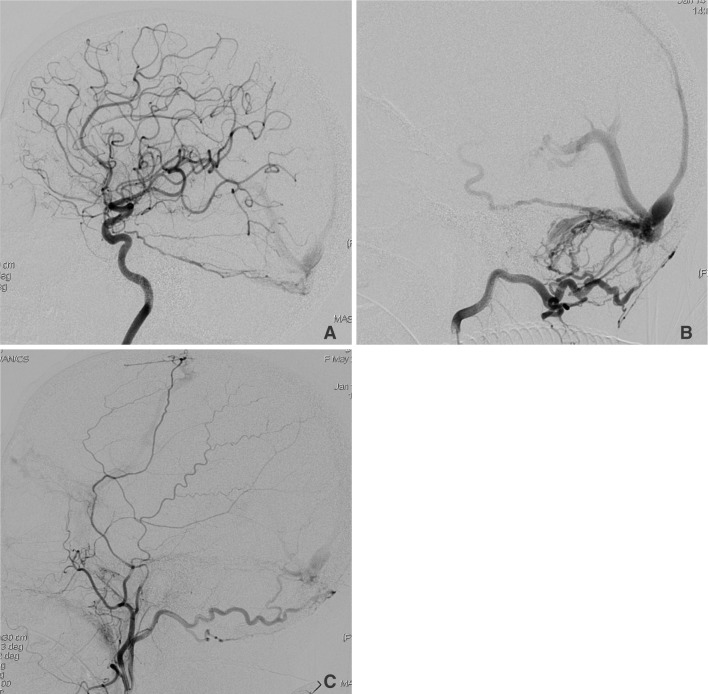
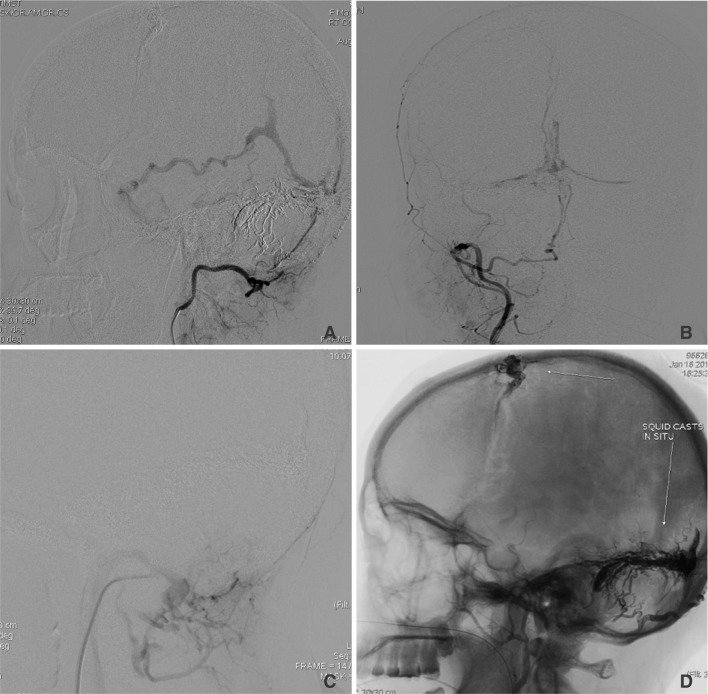
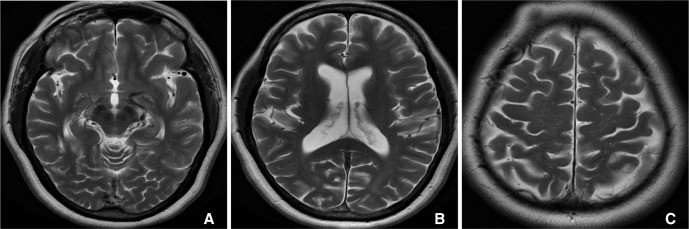
- Intracranial dural arteriovenous fistulae (DAVF) are acquired fistulous communications between dural arterial branches and dural venous sinuses or cortical veins with the nidus located within the leaflets of the duramater. Dementia and Parkinsonism are amongst the rarest of clinical presentations in DAVFs and are important to diagnose early, being treatable with timely intervention. We present an interesting case of a patient who presented with rapidly progressive dementia and features of parkinsonism who was diagnosed to have extensive DAVF and made remarkable recovery after embolization of the fistulae.
MeSH Terms
Figure
Reference
-
1. Lasjaunias P, Chiu M, ter Brugge K, Tolia A, Hurth M, Bernstein M. Neurological manifestations of intracranial dural arteriovenous malformations. J Neurosurg. 1986; 64:724–730. PMID: 3701421.
Article2. Awad IA, Little JR, Akarawi WP, Ahl J. Intracranial dural Arteriovenous malformations: factors predisposing to an aggressive neurological course. J Neurosurg. 1990; 72:839–850. PMID: 2140125.
Article3. Matsuda S, Waragai M, Shinotoh H, Takahashi N, Takagi K, Hattori T. Intracranial dural arteriovenous fistula (DAVF) presenting progressive dementia and parkinsonism. J Neurol Sci. 1999; 165:43–47. PMID: 10426146.
Article4. Lee PH, Lee JS, Shin DH, Kim BM, Huh K. Parkinsonism as an initial manifestation of dural arteriovenous fistula. Eur J Neurol. 2005; 12:403–406. PMID: 15804274.
Article5. Kim HR, Lee JY, Kim YK, Park H, Kim HJ, Son YJ, et al. Dural Arteriovenous Fistula-Associated Reversible Parkinsonism with Presynaptic Dopaminergic Loss. J Mov Disord. 2015; 8:141–143. PMID: 26413242.
Article6. Ma C, Lu Q, Shi W, Su Z, Zhao Y, Li C, et al. Diagnosis and treatment of a dural arteriovenous fistula presenting with progressive parkinsonism and dementia: a case report and literature review. Exp Ther Med. 2015; 9:523–526. PMID: 25574227.
Article7. Hurst RW, Bagley LJ, Galetta S, Glosser G, Lieberman AP, Trojanowski J, et al. Dementia resulting from dural Arteriovenous fistulas: the pathologic findings of venous hypertensive encephalopathy. AJNR Am J Neuroradiol. 1998; 19:1267–1273. PMID: 9726465.8. Netravathi M, Pal PK, Bharath RD, Ravishankar S. Intracranial dural arteriovenous fistula presenting as parkinsonism and cognitive dysfunction. J Clin Neurosci. 2011; 18:138–140. PMID: 20851606.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Occurrence of Metachronous Intracranial Dural Arteriovenous Fistula after Embolization of Intracranial Dural Arteriovenous Fistula: A Case Report
- Role of surgery in management of intracranial dural arteriovenous fistulas
- Syringomyelia Associated with Spinal Dural Arteriovenous Fistula: Clinical and Radiological Improvement after Embolization
- Papillary Meningioma Presenting as Rapidly Progressive Dementia and Parkinsonism
- Ruptured Cerebral Arteriovenous Malformation with Giant Venous Aneurysm: Case Report