Ann Rehabil Med.
2017 Jun;41(3):339-346. 10.5535/arm.2017.41.3.339.
Prediction of Post-stroke Falls by Quantitative Assessment of Balance
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul, Korea.
- 2Department of Rehabilitation Medicine, Seoul National University Boramae Medical Center, Seoul, Korea. ideale1@snu.ac.kr
- KMID: 2389448
- DOI: http://doi.org/10.5535/arm.2017.41.3.339
Abstract
OBJECTIVE
To evaluate characteristics of the postural instability in patients with stroke and to present a prediction model of post-stroke falls.
METHODS
Patients with a first-ever stroke who had been evaluated by the Balance Master (BM) at post-stroke 3 months (±1 month) between August 2011 and December 2015 were enrolled. Parameters for the postural instability, such as the weight bearing asymmetry (WBA) and postural sway velocity (PSV), were obtained. The fall events in daily lives were assessed via structured telephone interview with a fall related questionnaire.
RESULTS
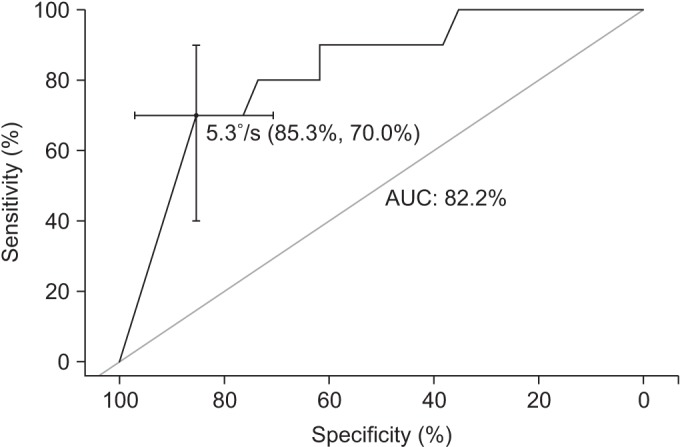
A total of 71 patients (45 men; 45 with ischemic stroke) were enrolled in this study. All subjects underwent BM evaluation at 3.03±0.40 months after stroke. The mean WBA was 17.18%±13.10% and mean PSV (measured as °/s) were noted as 0.66±0.37 (eyes-open on firm surface), 0.89±0.75 (eyes-closed on firm surface), 1.45±1.09 (eyes-open on soft surface), and 3.10±1.76 (eyes-closed on soft surface). A prediction model of post-stroke falls was drawn by multiple logistic regression analysis as follows: Risk of post-stroke falls = -2.848 + 1.878 x (PSV(ECSS)) + 0.154 x (age=1 if age≥65; age=0 if age<65).
CONCLUSION
The weight bearing asymmetry and postural sway were significantly increased in patients with stroke. Older age and impaired postural control increased the risk of post-stroke falls.
Keyword
MeSH Terms
Figure
Reference
-
1. Herman B, Leyten AC, van Luijk JH, Frenken CW, Op de Coul AA, Schulte BP. Epidemiology of stroke in Tilburg, the Netherlands. The population-based stroke incidence register. 2: Incidence, initial clinical picture and medical care, and three-week case fatality. Stroke. 1982; 13:629–634. PMID: 7123595.
Article2. Hochstenbach J, Donders R, Mulder T, Van Limbeek J, Schoonderwaldt H. Long-term outcome after stroke: a disability-orientated approach. Int J Rehabil Res. 1996; 19:189–200. PMID: 8910122.3. Bohannon RW, Leary KM. Standing balance and function over the course of acute rehabilitation. Arch Phys Med Rehabil. 1995; 76:994–996. PMID: 7487452.
Article4. Fong KN, Chan CC, Au DK. Relationship of motor and cognitive abilities to functional performance in stroke rehabilitation. Brain Inj. 2001; 15:443–453. PMID: 11350658.
Article5. Keenan MA, Perry J, Jordan C. Factors affecting balance and ambulation following stroke. Clin Orthop Relat Res. 1984; (182):165–171.
Article6. Sandin KJ, Smith BS. The measure of balance in sitting in stroke rehabilitation prognosis. Stroke. 1990; 21:82–86. PMID: 2300995.
Article7. Cathie AG. The influence of the lower extremities upon the structural integrity of the body. J Am Osteopath Assoc. 1950; 49:443–446. PMID: 15415324.8. Nashner LM, McCollum G. The organization of human postural movements: a formal basis and experimental synthesis. Behav Brain Sci. 1985; 8:135–150.
Article9. Kamphuis JF, de Kam D, Geurts AC, Weerdesteyn V. Is weight-bearing asymmetry associated with postural instability after stroke? A systematic review. Stroke Res Treat. 2013; 2013:692137. PMID: 23738232.
Article10. Mackintosh SF, Hill KD, Dodd KJ, Goldie PA, Culham EG. Balance score and a history of falls in hospital predict recurrent falls in the 6 months following stroke rehabilitation. Arch Phys Med Rehabil. 2006; 87:1583–1589. PMID: 17141637.
Article11. Weerdesteyn V, de Niet M, van Duijnhoven HJ, Geurts AC. Falls in individuals with stroke. J Rehabil Res Dev. 2008; 45:1195–1213. PMID: 19235120.12. Forster A, Young J. Incidence and consequences of falls due to stroke: a systematic inquiry. BMJ. 1995; 311:83–86. PMID: 7613406.13. Nyberg L, Gustafson Y. Patient falls in stroke rehabilitation. A challenge to rehabilitation strategies. Stroke. 1995; 26:838–842. PMID: 7740577.14. Yates JS, Lai SM, Duncan PW, Studenski S. Falls in community-dwelling stroke survivors: an accumulated impairments model. J Rehabil Res Dev. 2002; 39:385–394. PMID: 12173758.15. Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther. 2008; 88:559–566. PMID: 18292215.
Article16. Stevenson TJ. Detecting change in patients with stroke using the Berg Balance Scale. Aust J Physiother. 2001; 47:29–38. PMID: 11552860.
Article17. Mansfield A, Danells CJ, Zettel JL, Black SE, McIlroy WE. Determinants and consequences for standing balance of spontaneous weight-bearing on the paretic side among individuals with chronic stroke. Gait Posture. 2013; 38:428–432. PMID: 23357758.
Article18. Chen HY, Wing AM. Independent control of force and timing symmetry in dynamic standing balance: implications for rehabilitation of hemiparetic stroke patients. Hum Mov Sci. 2012; 31:1660–1669. PMID: 22939846.
Article19. Oken O, Yavuzer G. Spatio-temporal and kinematic asymmetry ratio in subgroups of patients with stroke. Eur J Phys Rehabil Med. 2008; 44:127–132. PMID: 18418332.20. Garland SJ, Ivanova TD, Mochizuki G. Recovery of standing balance and health-related quality of life after mild or moderately severe stroke. Arch Phys Med Rehabil. 2007; 88:218–227. PMID: 17270520.
Article21. Marigold DS, Eng JJ. The relationship of asymmetric weight-bearing with postural sway and visual reliance in stroke. Gait Posture. 2006; 23:249–255. PMID: 16399522.
Article22. Peurala SH, Kononen P, Pitkanen K, Sivenius J, Tarkka IM. Postural instability in patients with chronic stroke. Restor Neurol Neurosci. 2007; 25:101–108. PMID: 17726268.23. Pereira LC, Botelho AC, Martins EF. Relationships between body symmetry during weight-bearing and functional reach among chronic hemiparetic patients. Rev Bras Fisioter. 2010; 14:229–266.24. Sackley CM. Falls, sway, and symmetry of weight-bearing after stroke. Int Disabil Stud. 1991; 13:1–4. PMID: 1917796.
Article25. Bronstein AM, Buckwell D. Automatic control of postural sway by visual motion parallax. Exp Brain Res. 1997; 113:243–248. PMID: 9063710.
Article26. Marigold DS, Eng JJ, Tokuno CD, Donnelly CA. Contribution of muscle strength and integration of afferent input to postural instability in persons with stroke. Neurorehabil Neural Repair. 2004; 18:222–229. PMID: 15537993.
Article27. Geurts AC, Nienhuis B, Mulder TW. Intrasubject variability of selected force-platform parameters in the quantification of postural control. Arch Phys Med Rehabil. 1993; 74:1144–1150. PMID: 8239951.28. Lafond D, Corriveau H, Hebert R, Prince F. Intrasession reliability of center of pressure measures of postural steadiness in healthy elderly people. Arch Phys Med Rehabil. 2004; 85:896–901. PMID: 15179642.29. de Haart M, Geurts AC, Huidekoper SC, Fasotti L, van Limbeek J. Recovery of standing balance in postacute stroke patients: a rehabilitation cohort study. Arch Phys Med Rehabil. 2004; 85:886–895. PMID: 15179641.30. Mizrahi J, Solzi P, Ring H, Nisell R. Postural stability in stroke patients: vectorial expression of asymmetry, sway activity and relative sequence of reactive forces. Med Biol Eng Comput. 1989; 27:181–190. PMID: 2601436.
Article31. Barra J, Oujamaa L, Chauvineau V, Rougier P, Perennou D. Asymmetric standing posture after stroke is related to a biased egocentric coordinate system. Neurology. 2009; 72:1582–1587. PMID: 19414725.
Article32. Chien CW, Hu MH, Tang PF, Sheu CF, Hsieh CL. A comparison of psychometric properties of the smart balance master system and the postural assessment scale for stroke in people who have had mild stroke. Arch Phys Med Rehabil. 2007; 88:374–380. PMID: 17321832.
Article33. Liston RA, Brouwer BJ. Reliability and validity of measures obtained from stroke patients using the Balance Master. Arch Phys Med Rehabil. 1996; 77:425–430. PMID: 8629916.
Article34. Di Fabio RP, Badke MB. Relationship of sensory organization to balance function in patients with hemiplegia. Phys Ther. 1990; 70:542–548. PMID: 2392483.
Article35. Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics. 2011; 12:77. PMID: 21414208.
Article36. Ashburn A, Hyndman D, Pickering R, Yardley L, Harris S. Predicting people with stroke at risk of falls. Age Ageing. 2008; 37:270–276. PMID: 18456791.
Article37. Baetens T, De Kegel A, Calders P, Vanderstraeten G, Cambier D. Prediction of falling among stroke patients in rehabilitation. J Rehabil Med. 2011; 43:876–883. PMID: 21947179.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Balance Confidence and Balance Ability among Community-residing Stroke Patients
- Assitive Effect of Gait-aids for the Standing Balance
- Common Disorders Causing Balance Problems
- Efficacy and Safety of Caregiver-Mediated Exercise in Post-stroke Rehabilitation
- Changes to Balance and Trunk Repositioning Sense According to Frequency of Falls in Stroke Patients