Ann Rehabil Med.
2017 Aug;41(4):693-700. 10.5535/arm.2017.41.4.693.
A Preliminary Study on qEEG in Burn Patients With Chronic Pruritus
- Affiliations
-
- 1Spaulding Center of Neuromodulation, Spaulding Rehabilitation Hospital, Harvard Medical School, Boston, MA, USA. Fregni.felipe@mgh.harvard.edu
- 2Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital, Harvard Medical School, Boston, MA, USA.
- 3Brown University, Providence, RI, USA.
- 4Surgical Services, Sumner M. Redstone Burn Center, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA.
- 5Shriners Hospitals for Children-Boston, Boston, MA, USA.
- KMID: 2389416
- DOI: http://doi.org/10.5535/arm.2017.41.4.693
Abstract
OBJECTIVE
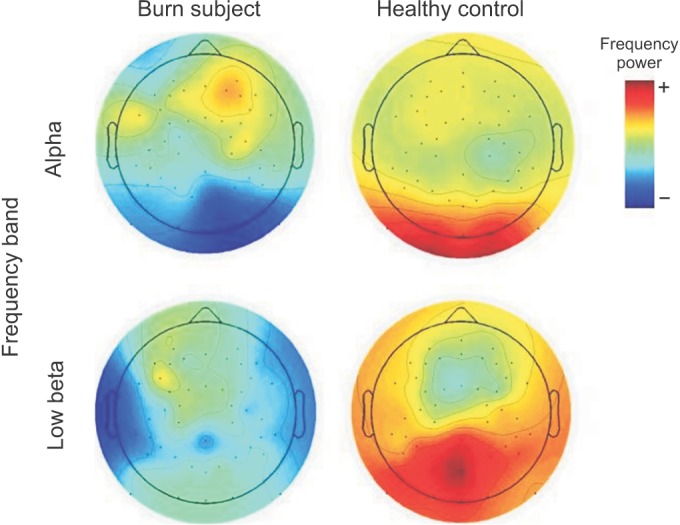
To explore and determine the reorganizational changes in the cortical neural circuits associated with pruritis, this study was undertaken to compare the electroencephalography (EEG) changes in burn patients having primary symptoms of chronic itching (pruritis) and their paired healthy subjects.
METHODS
Eight subjects were recruited for this exploratory pilot study: 4 patients with pruritus after burn injury matched by gender and age with 4 healthy subjects. EEG recordings were analyzed for absolute alpha, low beta, high beta, and theta power for both groups.
RESULTS
The mean age of the burn patients was 41.75 years; while the mean age for the matched healthy subjects was 41.5 years. All subjects were male. A decreased alpha activity was observed in the occipital channels (0.82 vs. 1.4; p=0.01) and a decreased low beta activity in the frontal area (0.22 vs. 0.4; p=0.049) in eyes closed conditions. An overall decreased theta trend was observed in both the eyes open and eyes closed conditions in burn patients, compared to healthy individuals.
CONCLUSION
This preliminary study presents initial evidence that chronic pruritus in burn subjects may be associated with brain reorganizational changes at the cortical level characterized by an EEG pattern.
Keyword
MeSH Terms
Figure
Reference
-
1. Schneider JC, Harris NL, El Shami A, Sheridan RL, Schulz JT 3rd, Bilodeau ML, et al. A descriptive review of neuropathic-like pain after burn injury. J Burn Care Res. 2006; 27:524–528. PMID: 16819359.
Article2. Vitale M, Fields-Blache C, Luterman A. Severe itching in the patient with burns. J Burn Care Rehabil. 1991; 12:330–333. PMID: 1682327.
Article3. Schneider JC, Bassi S, Ryan CM. Barriers impacting employment after burn injury. J Burn Care Res. 2009; 30:294–300. PMID: 19165112.
Article4. Mason ST, Esselman P, Fraser R, Schomer K, Truitt A, Johnson K. Return to work after burn injury: a systematic review. J Burn Care Res. 2012; 33:101–109. PMID: 22138806.5. Carrougher GJ, Martinez EM, McMullen KS, Fauerbach JA, Holavanahalli RK, Herndon DN, et al. Pruritus in adult burn survivors: postburn prevalence and risk factors associated with increased intensity. J Burn Care Res. 2013; 34:94–101. PMID: 23079565.6. Schneider JC, Nadler DL, Herndon DN, Kowalske K, Matthews K, Wiechman SA, et al. Pruritus in pediatric burn survivors: defining the clinical course. J Burn Care Res. 2015; 36:151–158. PMID: 25162949.7. Clark SA, Allard T, Jenkins WM, Merzenich MM. Receptive fields in the body-surface map in adult cortex defined by temporally correlated inputs. Nature. 1988; 332:444–445. PMID: 3352741.
Article8. Jensen MP, Sherlin LH, Gertz KJ, Braden AL, Kupper AE, Gianas A, et al. Brain EEG activity correlates of chronic pain in persons with spinal cord injury: clinical implications. Spinal Cord. 2013; 51:55–58. PMID: 22801188.
Article9. Boord P, Siddall PJ, Tran Y, Herbert D, Middleton J, Craig A. Electroencephalographic slowing and reduced reactivity in neuropathic pain following spinal cord injury. Spinal Cord. 2008; 46:118–123. PMID: 17502876.
Article10. Stander S, Weisshaar E, Mettang T, Szepietowski JC, Carstens E, Ikoma A, et al. Clinical classification of itch: a position paper of the International Forum for the Study of Itch. Acta Derm Venereol. 2007; 87:291–294. PMID: 17598029.
Article11. 1997 SSNR (Society for the Study of Neuronal Regulation) Presented Paper Abstracts. J Neuropathy. 1997; 2:61–69.12. Zachariah JR, Rao AL, Prabha R, Gupta AK, Paul MK, Lamba S. Post burn pruritus: a review of current treatment options. Burns. 2012; 38:621–629. PMID: 22244605.13. Portilla AS, Bravo GL, Miraval FK, Villamar MF, Schneider JC, Ryan CM, et al. A feasibility study assessing cortical plasticity in chronic neuropathic pain following burn injury. J Burn Care Res. 2013; 34:e48–e52. PMID: 23292595.
Article14. Egner T, Gruzelier JH. EEG biofeedback of low beta band components: frequency-specific effects on variables of attention and event-related brain potentials. Clin Neurophysiol. 2004; 115:131–139. PMID: 14706480.
Article15. Stinson B, Arthur D. A novel EEG for alpha brain state training, neurobiofeedback and behavior change. Complement Ther Clin Pract. 2013; 19:114–118. PMID: 23890456.
Article16. de Vries M, Wilder-Smith OH, Jongsma ML, van den Broeke EN, Arns M, van Goor H, et al. Altered resting state EEG in chronic pancreatitis patients: toward a marker for chronic pain. J Pain Res. 2013; 6:815–824. PMID: 24379694.
Article17. Lopes da. Neural mechanisms underlying brain waves: from neural membranes to networks. Electroencephalogr Clin Neurophysiol. 1991; 79:81–93. PMID: 1713832.18. Ray WJ, Cole HW. EEG alpha activity reflects attentional demands, and beta activity reflects emotional and cognitive processes. Science. 1985; 228:750–752. PMID: 3992243.
Article19. Mendham JE. Gabapentin for the treatment of itching produced by burns and wound healing in children: a pilot study. Burns. 2004; 30:851–853. PMID: 15555801.
Article20. LaSalle L, Rachelska G, Nedelec B. Naltrexone for the management of post-burn pruritus: a preliminary report. Burns. 2008; 34:797–802. PMID: 18325676.
Article21. Casaer M, Kums V, Wouters PJ, Van den kerckhove E, Van den Berghe G. Pruritus in patients with small burn injuries. Burns. 2008; 34:185–191. PMID: 17706362.
Article22. Kudina TA, Sudnitsyn VV, Kutyreva EV, Kichigina VF. The serotonin reuptake inhibitor fluoxetine suppresses theta oscillations in the electroencephalogram of the rabbit hippocampus. Neurosci Behav Physiol. 2004; 34:929–933. PMID: 15686138.
Article23. Sarnthein J, Stern J, Aufenberg C, Rousson V, Jeanmonod D. Increased EEG power and slowed dominant frequency in patients with neurogenic pain. Brain. 2006; 129:55–64. PMID: 16183660.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Skin Rehabilitation Massage Therapy on Pruritus, Skin Status, and Depression in Burn Survivors
- Chronic Pruritus: Clinics and Treatment
- Addiction and Quantitative Electroencephalography
- Clinical Applications of Quantitative EEG
- Relation between heart rate variability and spectral analysis of electroencephalogram in chronic neuropathic pain patients