Clin Endosc.
2017 May;50(3):234-241. 10.5946/ce.2017.079.
Endoscopic Accessories Used for More Advanced Endoluminal Therapeutic Procedures
- Affiliations
-
- 1Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea. hschungmd@gmail.com
- KMID: 2388819
- DOI: http://doi.org/10.5946/ce.2017.079
Abstract
- Endoscopic accessories describe an extensive variety of auxiliary instruments used for diagnostic and therapeutic endoscopy. Various endoscopic accessories have been developed over the previous few decades and are mostly used for treating neoplastic lesions, such as early gastrointestinal (GI) carcinomas and premalignant lesions. Because of extensive research on natural orifice endoluminal surgery (NOTES) in the early 2000s and recent technological developments, new devices have been developed for various advanced endoluminal therapeutic procedures. In particular, a remarkable development of endoscopic management was achieved in the field of gastroesophageal reflux disease (GERD) and obesity. In both conditions, there is treatment gap between medical and surgical therapy. A large proportion of the patients who do not respond to medical treatment and lifestyle modification, still hesitate to directly undergo surgical treatment. To bridge this gap, endoscopic management has been receiving increasing attention. In this article, I review endoscopic and/or endoluminal devices used for the treatment of GERD and obesity with proposed mechanisms of their function.
Keyword
Figure
Reference
-
1. Maradey-Romero C, Fass R. New and future drug development for gastroesophageal reflux disease. J Neurogastroenterol Motil. 2014; 20:6–16.
Article2. Chung H, Chon YE, Kim SU, et al. Noninvasive prediction of erosive esophagitis using a controlled attenuation parameter (CAP)-based risk estimation model. Dig Dis Sci. 2016; 61:507–516.
Article3. Kim KM, Cho YK, Bae SJ, et al. Prevalence of gastroesophageal reflux disease in Korea and associated health-care utilization: a national population-based study. J Gastroenterol Hepatol. 2012; 27:741–745.
Article4. El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014; 63:871–880.
Article5. Lazarus B, Chen Y, Wilson FP, et al. Proton pump inhibitor use and the risk of chronic kidney disease. JAMA Intern Med. 2016; 176:238–246.
Article6. Abraham NS. Proton pump inhibitors: potential adverse effects. Curr Opin Gastroenterol. 2012; 28:615–620.7. Yew KC, Chuah SK. Antireflux endoluminal therapies: past and present. Gastroenterol Res Pract. 2013; 2013:481417.
Article8. Du X, Hu Z, Yan C, Zhang C, Wang Z, Wu J. A meta-analysis of long follow-up outcomes of laparoscopic Nissen (total) versus Toupet (270 degrees ) fundoplication for gastro-esophageal reflux disease based on randomized controlled trials in adults. BMC Gastroenterol. 2016; 16:88.
Article9. Triadafilopoulos G. Stretta: a valuable endoscopic treatment modality for gastroesophageal reflux disease. World J Gastroenterol. 2014; 20:7730–7738.
Article10. Arts J, Bisschops R, Blondeau K, et al. A double-blind sham-controlled study of the effect of radiofrequency energy on symptoms and distensibility of the gastro-esophageal junction in GERD. Am J Gastroenterol. 2012; 107:222–230.
Article11. DiBaise JK, Brand RE, Quigley EM. Endoluminal delivery of radiofrequency energy to the gastroesophageal junction in uncomplicated GERD: efficacy and potential mechanism of action. Am J Gastroenterol. 2002; 97:833–842.
Article12. Noar M, Squires P, Noar E, Lee M. Long-term maintenance effect of radiofrequency energy delivery for refractory GERD: a decade later. Surg Endosc. 2014; 28:2323–2333.
Article13. Auyang ED, Carter P, Rauth T, Fanelli RD; SAGES Guidelines Committee. SAGES clinical spotlight review: endoluminal treatments for gastroesophageal reflux disease (GERD). Surg Endosc. 2013; 27:2658–2672.
Article14. Higuchi K, Fujiwara Y, Okazaki H, et al. Feasibility, safety, and efficacy of the Stretta procedure in Japanese patients with gastroesophageal reflux disease: first report from Asia. J Gastroenterol. 2007; 42:205–210.
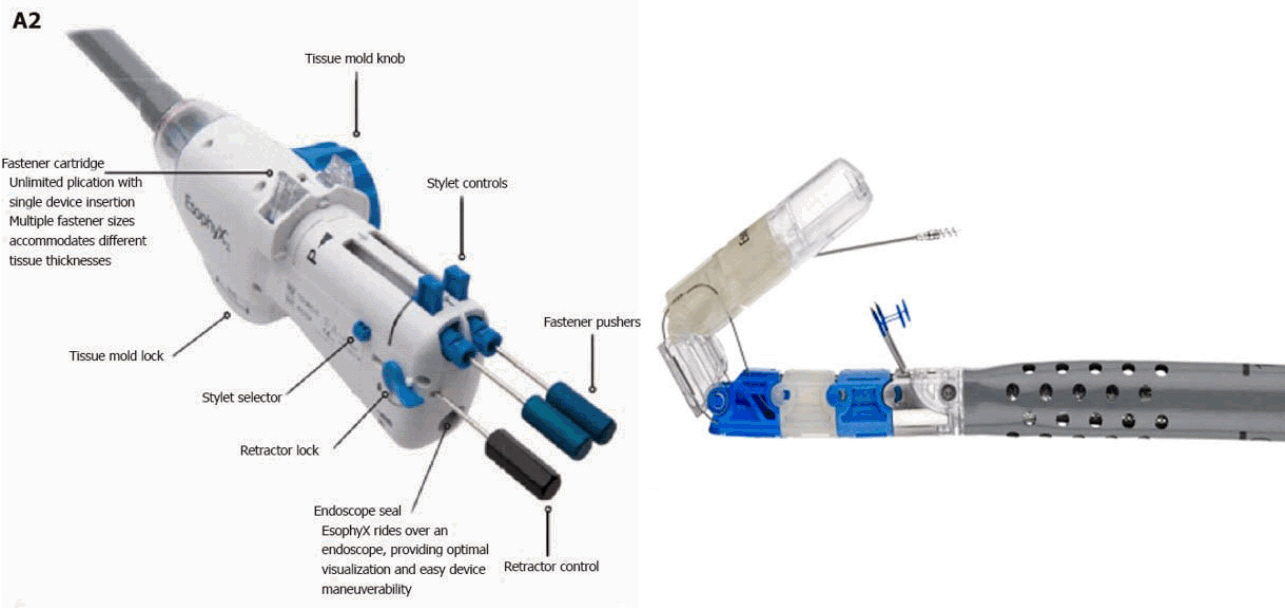
Article15. Herman RM, Wojtysiak D, Rys J, et al. Interstitial cells of Cajal (ICCs) and smooth muscle actin (SMA) activity after non-ablative radiofrequency energy application to the internal anal sphincter (IAS): an animal study [Internet]. Norwalk (CT): Mederi Therapeutics Inc;c2013. [updated 2013; cited 2017 May 21]. Available from: https://www.secca-therapy.com/clinicals/interstitial-cells-of-cajal-iccs-and-smoothmuscle-actin-sma-activity-af.16. Testoni PA, Mazzoleni G, Testoni SG. Transoral incisionless fundoplication for gastro-esophageal reflux disease: techniques and outcomes. World J Gastrointest Pharmacol Ther. 2016; 7:179–189.
Article17. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000; 894:i–xii. 1-253.18. OECD iLibrary. OECD health statistics [Internet]. Paris: OECD;c2015. [cited 2017 May 21]. Available from: http://dx.doi.org/10.1787/healthdata-en.19. Hankey CR. Session 3 (Joint with the British dietetic association): management of obesity: weight-loss interventions in the treatment of obesity. Proc Nutr Soc. 2010; 69:34–38.
Article20. Sjöström L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004; 351:2683–2693.
Article21. Obeid NR, Malick W, Concors SJ, Fielding GA, Kurian MS, Ren-Fielding CJ. Long-term outcomes after Roux-en-Y gastric bypass: 10- to 13- year data. Surg Obes Relat Dis. 2016; 12:11–20.22. van Rijn S, Roebroek YG, Masclee AA, van Heurn EL, Bouvy ND. Structural endoscopic techniques to treat obesity: a review. Surg Technol Int. 2015; 26:84–91.23. Abu Dayyeh BK, Edmundowicz S, Thompson CC. Clinical practice update: expert review on endoscopic bariatric therapies. Gastroenterology. 2017; 152:716–729.24. Kumar N, Peña Sahdala HN, Shaikh S, et al. Endoscopic sleeve gastroplasty for primary therapy of obesity: initial human cases. Gastroenterology. 2014; 146(5 Suppl 1):S571–S572.25. Abu Dayyeh BK, Acosta A, Camilleri M, et al. Endoscopic sleeve gastroplasty alters gastric physiology and induces loss of body weight in obese individuals. Clin Gastroenterol Hepatol. 2017; 15:37–43.e1.26. Abu Dayyeh BK, Rajan E, Gostout CJ. Endoscopic sleeve gastroplasty: a potential endoscopic alternative to surgical sleeve gastrectomy for treatment of obesity. Gastrointest Endosc. 2013; 78:530–535.
Article27. Sharaiha RZ, Kedia P, Kumta N, et al. Initial experience with endoscopic sleeve gastroplasty: technical success and reproducibility in the bariatric population. Endoscopy. 2015; 47:164–166.
Article28. Lopez-Nava G, Galvao M, Bautista-Castaño I, Fernandez-Corbelle JP, Trell M. Endoscopic sleeve gastroplasty with 1-year follow-up: factors predictive of success. Endosc Int Open. 2016; 4:E222–E227.
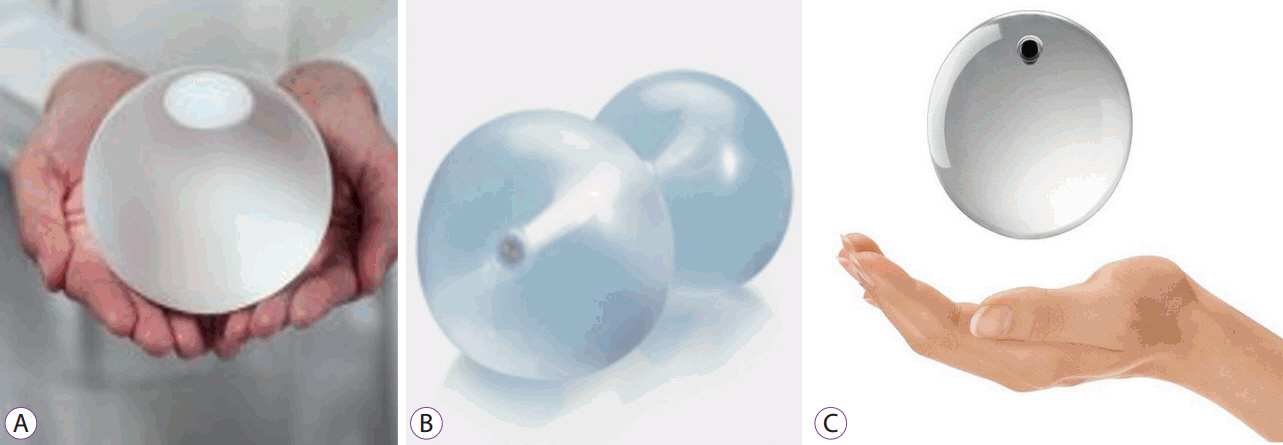
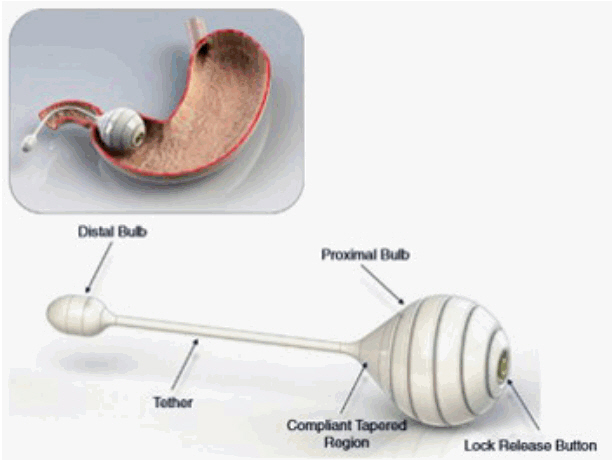
Article29. Lopez-Nava G, Sharaiha RZ, Neto MG, et al. Endoscopic sleeve gastroplasty for obesity: a multicenter study of 242 patients with 18 months follow-up. Gastroenterology. 2016; 150(4 Suppl 1):S26.30. Kumar N, Lopez-Nava G, Peña Sahdala HN, et al. Endoscopic sleeve gastroplasty: multicenter weight loss results. Gastroenterology. 2015; 148(4 Suppl 1):S–179.31. Gomez V, Woodman G, Abu Dayyeh BK. Delayed gastric emptying as a proposed mechanism of action during intragastric balloon therapy: results of a prospective study. Obesity (Silver Spring). 2016; 24:1849–1853.32. Mion F, Napoléon B, Roman S, et al. Effects of intragastric balloon on gastric emptying and plasma ghrelin levels in non-morbid obese patients. Obes Surg. 2005; 15:510–516.
Article33. Genco A, Bruni T, Doldi SB, et al. BioEnterics intragastric balloon: the Italian experience with 2,515 patients. Obes Surg. 2005; 15:1161–1164.
Article34. Farina MG, Baratta R, Nigro A, et al. Intragastric balloon in association with lifestyle and/or pharmacotherapy in the long-term management of obesity. Obes Surg. 2012; 22:565–571.
Article35. Sampath K, Rothstein RI. Selected endoscopic gastric devices for obesity. Gastrointest Endosc Clin N Am. 2017; 27:267–275.
Article36. Marinos G, Eliades C, Raman Muthusamy V, Greenway F. Weight loss and improved quality of life with a nonsurgical endoscopic treatment for obesity: clinical results from a 3- and 6-month study. Surg Obes Relat Dis. 2014; 10:929–934.
Article37. Schjoldager B, Mortensen PE, Myhre J, Christiansen J, Holst JJ. Oxyntomodulin from distal gut. Role in regulation of gastric and pancreatic functions. Dig Dis Sci. 1989; 34:1411–1419.38. Tsoli M, Chronaiou A, Kehagias I, Kalfarentzos F, Alexandrides TK. Hormone changes and diabetes resolution after biliopancreatic diversion and laparoscopic sleeve gastrectomy: a comparative prospective study. Surg Obes Relat Dis. 2013; 9:667–677.
Article39. Yousseif A, Emmanuel J, Karra E, et al. Differential effects of laparoscopic sleeve gastrectomy and laparoscopic gastric bypass on appetite, circulating acyl-ghrelin, peptide YY3-36 and active GLP-1 levels in non-diabetic humans. Obes Surg. 2014; 24:241–252.
Article40. Jirapinyo P, Thompson CC. Endoscopic bariatric and metabolic therapies: surgical analogues and mechanisms of action. Clin Gastroenterol Hepatol. 2017; 15:619–630.
Article41. Fishman E, Melanson D, Lamport R, Levine A. A novel endoscopic delivery system for placement of a duodenal-jejunal implant for the treatment of obesity and type 2 diabetes. Conf Proc IEEE Eng Med Biol Soc. 2008; 2008:2501–2503.
Article42. Jain D, Singhal S. Endoscopic bypass using Endobarrier devices: efficacy in treating obesity and metabolic syndrome. J Clin Gastroenterol. 2015; 49:799–803.43. Koehestanie P, Betzel B, Dogan K, et al. The feasibility of delivering a duodenal-jejunal bypass liner (EndoBarrier) endoscopically with patients under conscious sedation. Surg Endosc. 2014; 28:325–330.
Article44. Schouten R, Rijs CS, Bouvy ND, et al. A multicenter, randomized efficacy study of the EndoBarrier gastrointestinal liner for presurgical weight loss prior to bariatric surgery. Ann Surg. 2010; 251:236–243.
Article45. Rohde U. EndoBarrier gastrointestinal liner. Delineation of underlying mechanisms and clinical effects. Dan Med J. 2016; 63.46. Rohde U, Hedbäck N, Gluud LL, Vilsbøll T, Knop FK. Effect of the EndoBarrier gastrointestinal liner on obesity and type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab. 2016; 18:300–305.
Article47. Patel SR, Mason J, Hakim N. The duodenal-jejunal bypass sleeve (EndoBarrier gastrointestinal liner) for weight loss and treatment of type II diabetes. Indian J Surg. 2012; 74:275–277.
Article48. Patel SR, Hakim D, Mason J, Hakim N. The duodenal-jejunal bypass sleeve (EndoBarrier gastrointestinal liner) for weight loss and treatment of type 2 diabetes. Surg Obes Relat Dis. 2013; 9:482–484.
Article49. ASGE Bariatric Endoscopy Task Force; ASGE Technology Committee, Abu Dayyeh BK, et al. Endoscopic bariatric therapies. Gastrointest Endosc. 2015; 81:1073–1086.
Article50. Bennett MC, Badillo R, Sullivan S. Endoscopic management. Gastroenterol Clin North Am. 2016; 45:673–688.
Article51. Cherrington AD, Rajagopalan H, Maggs D, Devière J. Hydrothermal duodenal mucosal resurfacing: role in the treatment of metabolic disease. Gastrointest Endosc Clin N Am. 2017; 27:299–311.52. Rajagopalan H, Cherrington AD, Thompson CC, et al. Endoscopic duodenal mucosal resurfacing for the treatment of type 2 diabetes: 6-month interim analysis from the first-in-human proof-of-concept study. Diabetes Care. 2016; 39:2254–2261.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- History and Development of Accessories for Endoscopic Submucosal Dissection
- Recent Update of Accessories for ERCP
- Future Development of Endoscopic Accessories for Endoscopic Submucosal Dissection
- The development of robotic flexible endoscopic platforms
- Role of Restrictive Endoscopic Procedures in Obesity Treatment